Perinatology.
2019 Jun;30(2):47-53. 10.14734/PN.2019.30.2.47.
The Management and Outcomes of Placental Adhesion
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Gachon University Gil Medical Center, College of Medicine, Gachon University, Incheon, Korea. ksyob@gilhospital.com
- KMID: 2453037
- DOI: http://doi.org/10.14734/PN.2019.30.2.47
Abstract
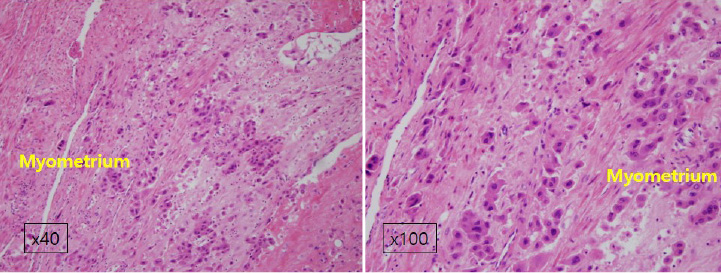
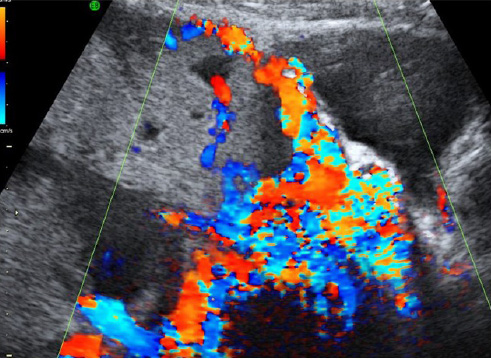
- Placenta adhesion, often involving placenta accreta, placenta increta, and placenta percreta, is a clinical term used to describe placenta that does not separate spontaneously and cannot be removed without causing abnormally high blood loss. Prior cesarean section, other uterine surgery, assisted reproduction techniques and placenta previa are all risk factors for placental adhesion and their prevalence has increased steadily. Maternal mortality and morbidity are reduced when accurate prenatal diagnosis of placental adhesion is made. Currently, grayscale ultrasonography, with or without color Doppler has been used widely. However, the performance of these markers shows considerable variability and most of findings are poorly defined. The standardized ultrasonography description should always be reported when performing an ultrasonography scan for suspected placental adhesion to advance diagnosis and treatment. When suspicious findings are identified preoperatively, management should be tailored accordingly. The location and timing of delivery, access to a multidisciplinary care team, availability of the appropriate surgical approach, and access adjunctive techniques are key issues. In conclusion, placental adhesion is a clinically relevant, difficult-to-manage problem with rising incidence worldwide. Tertiary care hospital with an experienced optimum management should be considered and the basis for appropriate risk assessment and delivery planning improves maternal outcome.
Keyword
MeSH Terms
Figure
Reference
-
1. Irving FC, Hertig AT. A study of placenta accreta. Surg Gynec Obst. 1937; 64:178.2. Silver RM. Delivery after previous cesarean: long-term maternal outcomes. Semin Perinatol. 2010; 34:258–266.
Article3. Silver RM. Implications of the first cesarean: perinatal and future reproductive health and subsequent cesareans, placentation issues, uterine rupture risk, morbidity, and mortality. Semin Perinatol. 2012; 36:315–323.
Article4. Jauniaux E, Collins SL, Jurkovic D, Burton GJ. Accreta placentation: a systematic review of prenatal ultrasound imaging and grading of villous invasiveness. Am J Obstet Gynecol. 2016; 215:712–721.
Article5. Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997; 177:210–214.
Article6. Collins SL, Ashcroft A, Braun T, Calda P, Langhoff-Roos J, Morel O, et al. Proposal for standardized ultrasound descriptors of abnormally invasive placenta (AIP). Ultrasound Obstet Gynecol. 2016; 47:271–275.
Article7. Bauer ST, Bonanno C. Abnormal placentation. Semin Perinatol. 2009; 33:88–96.
Article8. Wu S, Kocherginsky M, Hibbard JU. Abnormal placentation: twenty-year analysis. Am J Obstet Gynecol. 2005; 192:1458–1461.
Article9. Publications Committee, Society for Maternal-Fetal Medicine. Belfort MA. Placenta accreta. Am J Obstet Gynecol. 2010; 203:430–439.
Article10. Hull AD, Moore TR. Multiple repeat cesareans and the threat of placenta accreta: incidence, diagnosis, management. Clin Perinatol. 2011; 38:285–296.
Article11. Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA, et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol. 2006; 107:1226–1232.
Article12. Jauniaux E, Jurkovic D. Placenta accreta: pathogenesis of a 20th century iatrogenic uterine disease. Placenta. 2012; 33:244–251.
Article13. Eller AG, Porter TF, Soisson P, Silver RM. Optimal management strategies for placenta accreta. BJOG. 2009; 116:648–654.
Article14. Greenberg JI, Suliman A, Iranpour P, Angle N. Prophylactic balloon occlusion of the internal iliac arteries to treat abnormal placentation: a cautionary case. Am J Obstet Gynecol. 2007; 197:470.e1–470.e4.
Article15. Timmermans S, van Hof AC, Duvekot JJ. Conservative management of abnormally invasive placentation. Obstet Gynecol Surv. 2007; 62:529–539.
Article16. Mazouni C, Gorincour G, Juhan V, Bretelle F. Placenta accreta: a review of current advances in prenatal diagnosis. Placenta. 2007; 28:599–603.
Article17. Zhou J, Li J, Yan P, Ye YH, Peng W, Wang S, et al. Maternal plasma levels of cell-free β-HCG mRNA as a prenatal diagnostic indicator of placenta accrete. Placenta. 2014; 35:691–695.
Article18. Sekizawa A, Jimbo M, Saito H, Iwasaki M, Sugito Y, Yukimoto Y, et al. Increased cell-free fetal DNA in plasma of two women with invasive placenta. Clin Chem. 2002; 48:353–354.
Article19. Beuker JM, Erwich JJ, Khong TY. Is endomyometrial injury during termination of pregnancy or curettage following miscarriage the precursor to placenta accreta? J Clin Pathol. 2005; 58:273–275.
Article20. Bartels HC, Postle JD, Downey P, Brennan DJ. Placenta accreta spectrum: a review of pathology, molecular biology, and biomarkers. Dis Markers. 2018; 2018:1507674.
Article21. Eller AG, Bennett MA, Sharshiner M, Masheter C, Soisson AP, Dodson M, et al. Maternal morbidity in cases of placenta accreta managed by a multidisciplinary care team compared with standard obstetric care. Obstet Gynecol. 2011; 117:331–337.
Article22. Chantraine F, Braun T, Gonser M, Henrich W, Tutschek B. Prenatal diagnosis of abnormally invasive placenta reduces maternal peripartum hemorrhage and morbidity. Acta Obstet Gynecol Scand. 2013; 92:439–444.
Article23. Comstock CH. Antenatal diagnosis of placenta accreta: a review. Ultrasound Obstet Gynecol. 2005; 26:89–96.
Article24. Wong HS, Cheung YK, Strand L, Carryer P, Parker S, Tait J, et al. Specific sonographic features of placenta accreta: tissue interface disruption on gray-scale imaging and evidence of vessels crossing interface-disruption sites on Doppler imaging. Ultrasound Obstet Gynecol. 2007; 29:239–240.25. Dwyer BK, Belogolovkin V, Tran L, Rao A, Carroll I, Barth R, et al. Prenatal diagnosis of placenta accreta: sonography or magnetic resonance imaging? J Ultrasound Med. 2008; 27:1275–1281.26. Nguyen D, Nguyen C, Yacobozzi M, Bsat F, Rakita D. Imaging of the placenta with pathologic correlation. Semin Ultrasound CT MR. 2012; 33:65–77.
Article27. D'Antonio F, Iacovella C, Bhide A. Prenatal identification of invasive placentation using ultrasound: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2013; 42:509–517.28. Cho GJ, Kim LY, Hong HR, Lee CE, Hong SC, Oh MJ, et al. Trends in the rates of peripartum hysterectomy and uterine artery embolization. PLoS One. 2013; 8:e60512.
Article29. Robinson BK, Grobman WA. Effectiveness of timing strategies for delivery of individuals with placenta previa and accreta. Obstet Gynecol. 2010; 116:835–842.
Article30. Dubois J, Garel L, Grignon A, Lemay M, Leduc L. Placenta percreta: balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. Am J Obstet Gynecol. 1997; 176:723–726.
Article31. Hull AD, Resnik R. Placenta accreta and postpartum hemorrhage. Clin Obstet Gynecol. 2010; 53:228–236.
Article32. Bodner LJ, Nosher JL, Gribbin C, Siegel RL, Beale S, Scorza W. Balloon-assisted occlusion of the internal iliac arteries in patients with placenta accreta/percreta. Cardiovasc Intervent Radiol. 2006; 29:354–361.
Article33. Shih JC, Liu KL, Shyu MK. Temporary balloon occlusion of the common iliac artery: new approach to bleeding control during cesarean hysterectomy for placenta percreta. Am J Obstet Gynecol. 2005; 193:1756–1758.
Article34. Minas V, Gul N, Shaw E, Mwenenchanya S. Prophylactic balloon occlusion of the common iliac arteries for the management of suspected placenta accreta/percreta: conclusions from a short case series. Arch Gynecol Obstet. 2015; 291:461–465.
Article35. Chou MM, Kung HF, Hwang JI, Chen WC, Tseng JJ. Temporary prophylactic intravascular balloon occlusion of the common iliac arteries before cesarean hysterectomy for controlling operative blood loss in abnormal placentation. Taiwan J Obstet Gynecol. 2015; 54:493–498.
Article36. Cho YJ, Oh YT, Kim SY, Kim JY, Jung SY, Chon SJ, et al. The efficacy of pre-delivery prophylactic trans-catheter arterial balloon occlusion of bilateral internal iliac artery in patients with suspected placental adhesion. Obstet Gynecol Sci. 2017; 60:18–25.
Article37. Sentilhes L, Ambroselli C, Kayem G, Provansal M, Fernandez H, Perrotin F, et al. Maternal outcome after conservative treatment of placenta accreta. Obstet Gynecol. 2010; 115:526–534.
Article38. Tseng JJ, Chou MM, Hsieh YT, Wen MC, Ho ES, Hsu SL. Differential expression of vascular endothelial growth factor, placenta growth factor and their receptors in placentae from pregnancies complicated by placenta accreta. Placenta. 2006; 27:70–78.
Article39. McMahon K, Karumanchi A, Stillman IE, Cummings P, Patton D, Eastering T. Dose soluble fms-like tyrosine kinase-1 regulate placental invasion? Insight from the invasive placenta. Am J Obstet Gynecol. 2014; 210:68.e1–68.e4.40. Xie L, Sadovsky Y. The function of miR-519d in cell migration, invasion, and proliferation suggests a role in early placentation. Placenta. 2016; 48:34–37.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The efficacy of pre-delivery prophylactic trans-catheter arterial balloon occlusion of bilateral internal iliac artery in patients with suspected placental adhesion
- Subchorionic Placental Cyst with Placental Infarction on Maternal Floor: A Case Report
- Endogenous Digoxin-like Substance in Neonatal Serum, Pregnant Women and Placental Extracts
- Treatment of placental abruption following blunt abdominal trauma: a case report
- Recent advances in management of fetal growth restriction