Obstet Gynecol Sci.
2017 Jan;60(1):18-25. 10.5468/ogs.2017.60.1.18.
The efficacy of pre-delivery prophylactic trans-catheter arterial balloon occlusion of bilateral internal iliac artery in patients with suspected placental adhesion
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Gachon University Gil Medical Center, Incheon, Korea. ksyob@gilhospital.com
- 2Department of Interventional Radiology, Gachon University Gil Medical Center, Incheon, Korea.
- KMID: 2383203
- DOI: http://doi.org/10.5468/ogs.2017.60.1.18
Abstract
OBJECTIVE
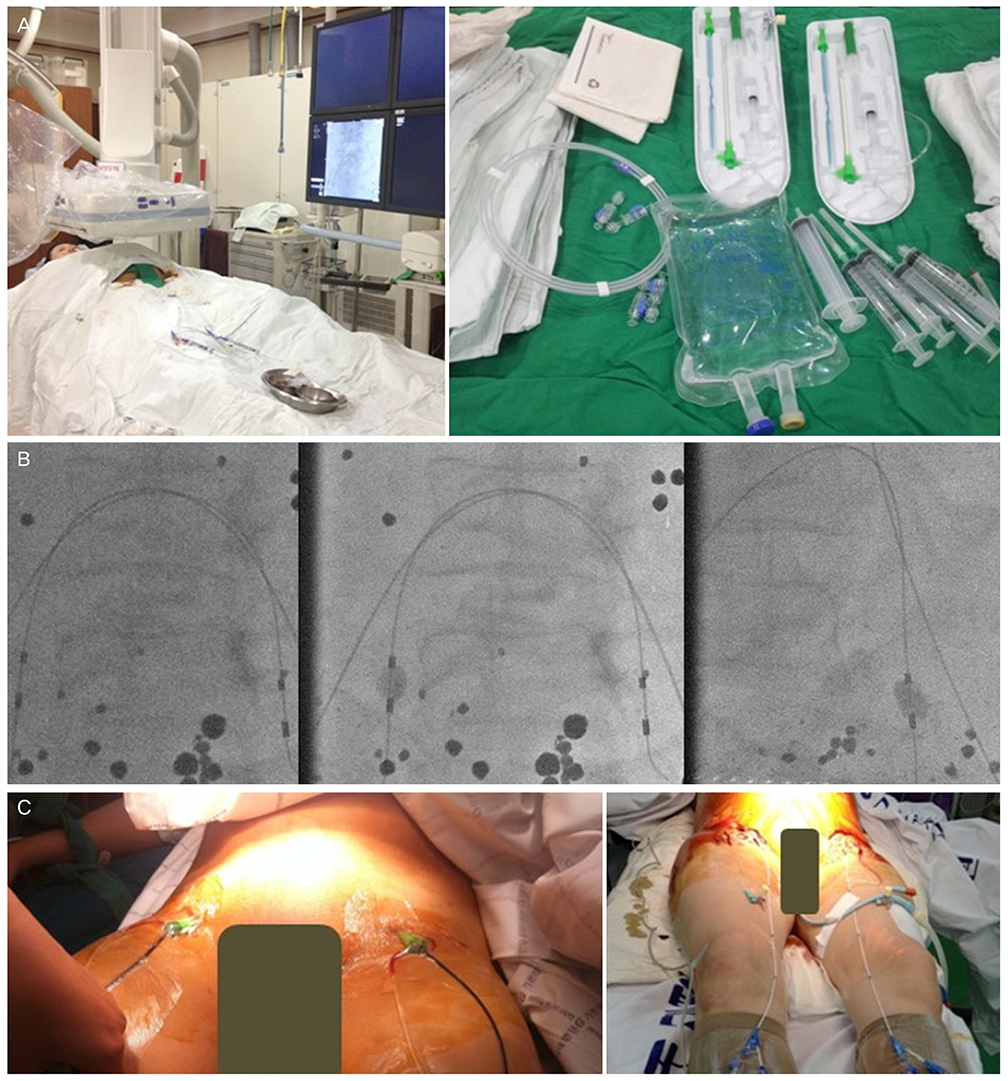
Prophylactic trans-catheter arterial balloon occlusion (PTABO) before cesarean section of placenta previa totalis has been introduced to prevent massive hemorrhage. The purpose of this study is to evaluate the clinical usefulness of PTABO in cases of suspected placental adhesion and to examine antepartal risk factors and perinatal outcomes in women with placental adhesion.
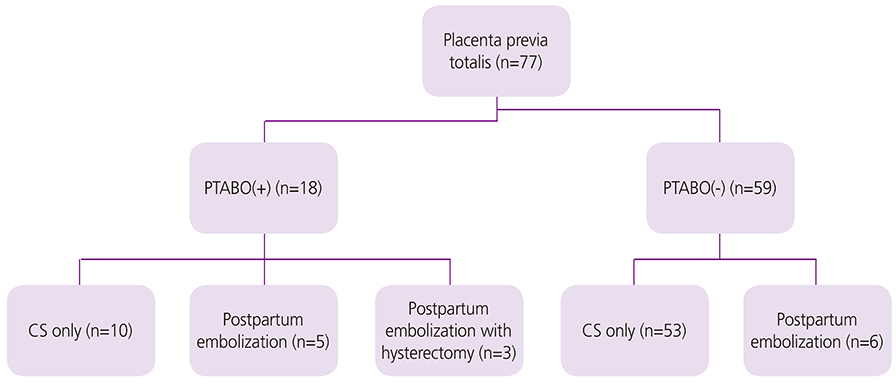
METHODS
Between January 2012 and December 2015, 77 patients who had undergone ultrasonography for evaluation of placenta previa were enrolled in this study. Seventeen of these patients with suspected placental adhesion by ultrasonography and Pelvic MRI underwent PTABO before cesarean section and another 59 patients underwent cesarean section without PTABO. Antepartal risk factors and peripartum maternal and neonatal outcomes were compared between patients with PTABO and those without PTABO.
RESULTS
More advanced maternal age, longer in gestational weeks at delivery, and more common previous cesarean section history were observed in the PTABO group. Placenta adhesion, abnormal Doppler findings, and frequency of transfusion were more common in the PTABO group. However there was no significant difference in estimated blood loss, hospital days, and neonatal outcome. It had occurred 3 cases of hysterectomy and 1 case of uterine artery embolization after cesarean section in the PTABO group.
CONCLUSION
Close surveillance of antepartum risk factors for placental adhesion using ultrasonography and pelvic magnetic resonance imaging is important to prevention of massive hemorrhage during cesarean section. PTABO before cesarean section might result in reduced blood loss and requirement for transfusion during the operation.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Management and Outcomes of Placental Adhesion
Suk Young Kim, Su Kyeong Kong, Yoo Jung Lee
Perinatology. 2019;30(2):47-53. doi: 10.14734/PN.2019.30.2.47.
Reference
-
1. Cali G, Forlani F, Giambanco L, Amico ML, Vallone M, Puccio G, et al. Prophylactic use of intravascular balloon catheters in women with placenta accreta, increta and percreta. Eur J Obstet Gynecol Reprod Biol. 2014; 179:36–41.2. Fitzpatrick KE, Sellers S, Spark P, Kurinczuk JJ, Brocklehurst P, Knight M. The management and outcomes of placenta accreta, increta, and percreta in the UK: a populationbased descriptive study. BJOG. 2014; 121:62–70.3. Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta accreta. Am J Obstet Gynecol. 1997; 177:210–214.4. Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with greater number of cesarean deliveries and higher parity. Obstet Gynecol. 2002; 99:976–980.5. Duan XH, Wang YL, Han XW, Chen ZM, Chu QJ, Wang L, et al. Caesarean section combined with temporary aortic balloon occlusion followed by uterine artery embolisation for the management of placenta accreta. Clin Radiol. 2015; 70:932–937.6. Teixidor Vinas M, Chandraharan E, Moneta MV, Belli AM. The role of interventional radiology in reducing haemorrhage and hysterectomy following caesarean section for morbidly adherent placenta. Clin Radiol. 2014; 69:e345–e351.7. Giambattista E, Ossola MW, Duiella SF, Crovetto F, Acaia B, Somigliana E, et al. Predicting factors for emergency peripartum hysterectomy in women with placenta previa. Arch Gynecol Obstet. 2012; 285:901–906.8. Tan CH, Tay KH, Sheah K, Kwek K, Wong K, Tan HK, et al. Perioperative endovascular internal iliac artery occlusion balloon placement in management of placenta accreta. AJR Am J Roentgenol. 2007; 189:1158–1163.9. Minas V, Gul N, Shaw E, Mwenenchanya S. Prophylactic balloon occlusion of the common iliac arteries for the management of suspected placenta accreta/percreta: conclusions from a short case series. Arch Gynecol Obstet. 2015; 291:461–465.10. Tosato F, Carnevale L, Monsellato I, Martone N, Martire I, Leonardo G, et al. Intragastric balloon in bariatric surgery. G Chir. 2006; 27:53–58.11. Gronvall M, Tikkanen M, Metsatahti M, Loukovaara M, Paavonen J, Stefanovic V. Pelvic arterial embolization in severe obstetric hemorrhage. Acta Obstet Gynecol Scand. 2014; 93:716–719.12. Ballas J, Hull AD, Saenz C, Warshak CR, Roberts AC, Resnik RR, et al. Preoperative intravascular balloon catheters and surgical outcomes in pregnancies complicated by placenta accreta: a management paradox. Am J Obstet Gynecol. 2012; 207:216.e1–216.e5.13. Bodner LJ, Nosher JL, Gribbin C, Siegel RL, Beale S, Scorza W. Balloon-assisted occlusion of the internal iliac arteries in patients with placenta accreta/percreta. Cardiovasc Intervent Radiol. 2006; 29:354–361.14. Dilauro MD, Dason S, Athreya S. Prophylactic balloon occlusion of internal iliac arteries in women with placenta accreta: literature review and analysis. Clin Radiol. 2012; 67:515–520.15. Howard TF, Grobman WA. The relationship between timing of postpartum hemorrhage interventions and adverse outcomes. Am J Obstet Gynecol. 2015; 213:239.e1–239.e3.16. Sadashivaiah J, Wilson R, Thein A, McLure H, Hammond CJ, Lyons G. Role of prophylactic uterine artery balloon catheters in the management of women with suspected placenta accreta. Int J Obstet Anesth. 2011; 20:282–287.17. Mok M, Heidemann B, Dundas K, Gillespie I, Clark V. Interventional radiology in women with suspected placenta accreta undergoing caesarean section. Int J Obstet Anesth. 2008; 17:255–261.18. Kim MA, Hwang HS, Kim YR, Kim BN, Yang ES, Lim JH, et al. The indications, effectiveness and complications of the selective arterial embolization in the management of obstetrical hemorrhage. Korean J Obstet Gynecol. 2007; 50:969–975.19. Clausen C, Lonn L, Langhoff-Roos J. Management of placenta percreta: a review of published cases. Acta Obstet Gynecol Scand. 2014; 93:138–143.20. Yoon JY, Ryoo UN, Noh SK, Song SE, Seo ES, Lee SH, et al. Emergent hysterectomy and angiographic embolization for the management of obstetrical hemorrhage: 8-year experiences. Korean J Obstet Gynecol. 2009; 52:180–187.21. Kim JR, Cho YK, Kim HM, Choi EJ, Kim DW, Seo YS, et al. Angiographic findings and effect of superselective embolization for early and late postpartum bleeding. Korean J Obstet Gynecol. 2009; 52:44–52.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Embolization of carotid-cavernous fistula using a silicone balloon and a tracker catheter system
- External Iliac Artery Transection Managed by Iliofemoral Bypass Grafting Using Temporary Balloon Occlusion
- Endovascular Treatment for Common Iliac Artery Injury Complicating Lumbar Disc Surgery : Limited Usefulness of Temporary Balloon Occlusion
- Placement of Balloon-Expandable Intraluminal Stent in Recurrent Iliac Artery Stenosis
- A Catheter Fragment in External Iliac Artery Cutted during Femoral Artery Cannulation: A case report