Investig Magn Reson Imaging.
2019 Jun;23(2):125-135. 10.13104/imri.2019.23.2.125.
Prediction of Axillary Lymph Node Metastasis in Early Breast Cancer Using Dynamic Contrast-Enhanced Magnetic Resonance Imaging and Diffusion-Weighted Imaging
- Affiliations
-
- 1Department of Radiology and Research Institute of Clinical Medicine of Chonbuk National University-Biomedical Research Institute of Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju, Korea. cejcej80@hanmail.net
- 2Department of Statistics, Chonbuk National University, Research Institute of Applied Statistics, Jeonju, Korea.
- KMID: 2452526
- DOI: http://doi.org/10.13104/imri.2019.23.2.125
Abstract
- PURPOSE
The purpose of this study was to evaluate dynamic contrast-enhanced breast magnetic resonance imaging (DCE-MRI), and diffusion-weighted imaging (DWI) variables, for axillary lymph node (ALN) metastasis in the early stage of breast cancer.
MATERIALS AND METHODS
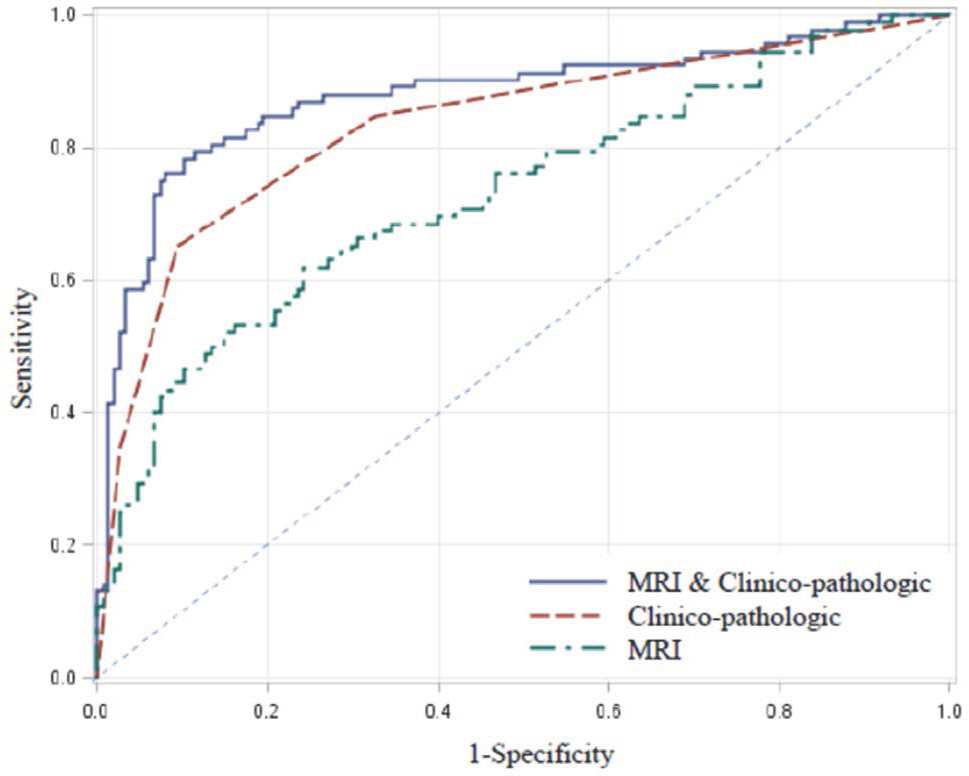
January 2011-April 2015, 787 patients with early stage of breast cancer were retrospectively reviewed. Only cases of invasive ductal carcinoma, were included in the patient population. Among them, 240 patients who underwent 3.0-T DCE-MRI, including DWI with b value 0 and 800 s/mm² were enrolled. MRI variables (adjacent vessel sign, whole-breast vascularity, initial enhancement pattern, quantitative kinetic parameters, signal enhancement ratio (SER), tumor apparent diffusion coefficient (ADC), peritumoral ADC, and peritumor-tumor ADC ratio) clinico-pathologic variables (age, T stage, multifocality, extensive intraductal carcinoma component (EIC), estrogen receptor, progesterone receptor, HER-2 status, Ki-67, molecular subtype, histologic grade, and nuclear grade) were compared between patients with axillary lymph node metastasis and those with no lymph node metastasis. Multivariate regression analysis was performed, to determine independent variables associated with ALN metastasis, and the area under the receiver operating characteristic curve (AUC), for predicting ALN metastasis was analyzed, for those variables.
RESULTS
On breast MRI, moderate or prominent ipsilateral whole-breast vascularity (moderate, odds ratio [OR] 3.45, 95% confidence interval [CI] 1.28-9.51 vs. prominent, OR = 15.59, 95% CI 2.52-96.46), SER (OR = 1.68, 95% CI 1.09-2.59), and peritumor-tumor ADC ratio (OR = 6.77, 95% CI 2.41-18.99), were independently associated with ALN metastasis. Among clinico-pathologic variables, HER-2 positivity was independently associated, with ALN metastasis (OR = 23.71, 95% CI 10.50-53.54). The AUC for combining selected MRI variables and clinico-pathologic variables, was higher than that of clinico-pathologic variables (P < 0.05).
CONCLUSION
SER, moderate or prominent increased whole breast vascularity, and peritumor-tumor ADC ratio on breast MRI, are valuable in predicting ALN metastasis, in patients with early stage of breast cancer.
Keyword
MeSH Terms
-
Area Under Curve
Breast Neoplasms*
Breast*
Carcinoma, Ductal
Carcinoma, Intraductal, Noninfiltrating
Diffusion
Diffusion Magnetic Resonance Imaging
Estrogens
Humans
Lymph Nodes*
Magnetic Resonance Imaging*
Neoplasm Metastasis*
Odds Ratio
Receptors, Progesterone
Retrospective Studies
ROC Curve
Estrogens
Receptors, Progesterone
Figure
Reference
-
References
1. Park EH, Min SY, Kim Z, et al. Basic facts of breast cancer in Korea in 2014: The 10-year overall survival progress. J Breast Cancer. 2017; 20:1–11.
Article2. Kuijs VJ, Moossdorff M, Schipper RJ, et al. The role of MRI in axillary lymph node imaging in breast cancer patients: a systematic review. Insights Imaging. 2015; 6:203–215.
Article3. Qiu SQ, Zeng HC, Zhang F, et al. A nomogram to predict the probability of axillary lymph node metastasis in early breast cancer patients with positive axillary ultrasound. Sci Rep. 2016; 6:21196.
Article4. Roaten JB, Pearlman N, Gonzalez R, Gonzalez R, McCarter MD. Identifying risk factors for complications following sentinel lymph node biopsy for melanoma. Arch Surg. 2005; 140:85–89.
Article5. Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011; 305:569–575.6. Caudle AS, Hunt KK, Tucker SL, et al. American College of Surgeons Oncology Group (ACOSOG) Z0011: impact on surgeon practice patterns. Ann Surg Oncol. 2012; 19:3144–3151.
Article7. Kvistad KA, Rydland J, Smethurst HB, Lundgren S, Fjosne HE, Haraldseth O. Axillary lymph node metastases in breast cancer: preoperative detection with dynamic contrast-enhanced MRI. Eur Radiol. 2000; 10:1464–1471.
Article8. Valente SA, Levine GM, Silverstein MJ, et al. Accuracy of predicting axillary lymph node positivity by physical examination, mammography, ultrasonography, and magnetic resonance imaging. Ann Surg Oncol. 2012; 19:1825–1830.
Article9. Bahri S, Chen JH, Yu HJ, Kuzucan A, Nalcioglu O, Su MY. Can dynamic contrast-enhanced MRI (DCE-MRI) predict tumor recurrence and lymph node status in patients with breast cancer? Ann Oncol. 2008; 19:822–824.
Article10. Zaiton F, Shehata SM, Abo Warda MH, Alekrashy MA. Diagnostic value of MRI for predicting axillarylymph nodes metastasis in newly diagnosed breastcancer patients: Diffusion-weighted MRI. Egypt J Radiol Nucl Med. 2016; 47:659–667.11. Hatakenaka M, Soeda H, Yabuuchi H, et al. Apparent diffusion coefficients of breast tumors: clinical application. Magn Reson Med Sci. 2008; 7:23–29.
Article12. Marini C, Iacconi C, Giannelli M, Cilotti A, Moretti M, Bartolozzi C. Quantitative diffusion-weighted MR imaging in the differential diagnosis of breast lesion. Eur Radiol. 2007; 17:2646–2655.
Article13. Dietzel M, Baltzer PA, Vag T, et al. Application of breast MRI for prediction of lymph node metastases – systematic approach using 17 individual descriptors and a dedicated decision tree. Acta Radiol. 2010; 51:885–894.
Article14. Luo N, Su D, Jin G, et al. Apparent diffusion coefficient ratio between axillary lymph node with primary tumor to detect nodal metastasis in breast cancer patients. J Magn Reson Imaging. 2013; 38:824–828.
Article15. Razek AA, Gaballa G, Denewer A, Nada N. Invasive ductal carcinoma: correlation of apparent diffusion coefficient value with pathological prognostic factors. NMR Biomed. 2010; 23:619–623.
Article16. Dietzel M, Baltzer PA, Vag T, et al. The adjacent vessel sign on breast MRI: new data and a subgroup analysis for 1,084 histologically verified cases. Korean J Radiol. 2010; 11:178–186.
Article17. Knopp MV, Bourne MW, Sardanelli F, et al. Gadobenate dimeglumine-enhanced MRI of the breast: analysis of dose response and comparison with gadopentetate dimeglumine. AJR Am J Roentgenol. 2003; 181:663–676.18. Kang DK, Kim EJ, Kim HS, Sun JS, Jung YS. Correlation of whole-breast vascularity with ipsilateral breast cancers using contrast-enhanced MDCT. AJR Am J Roentgenol. 2008; 190:496–504.
Article19. Esserman L, Hylton N, George T, Weidner N. Contrast-enhanced magnetic resonance imaging to assess tumor histopathology and angiogenesis in breast carcinoma. Breast J. 1999; 5:13–21.
Article20. Mori N, Mugikura S, Takasawa C, et al. Peritumoral apparent diffusion coefficients for prediction of lymphovascular invasion in clinically node-negative invasive breast cancer. Eur Radiol. 2016; 26:331–339.
Article21. Sardanelli F, Iozzelli A, Fausto A, Carriero A, Kirchin MA. Gadobenate dimeglumine-enhanced MR imaging breast vascular maps: association between invasive cancer and ipsilateral increased vascularity. Radiology. 2005; 235:791–797.
Article22. Wright H, Listinsky J, Quinn C, Rim A, Crowe J, Kim J. Increased ipsilateral whole breast vascularity as measured by contrast-enhanced magnetic resonance imaging in patients with breast cancer. Am J Surg. 2005; 190:576–579.
Article23. Han M, Kim TH, Kang DK, Kim KS, Yim H. Prognostic role of MRI enhancement features in patients with breast cancer: value of adjacent vessel sign and increased ipsilateral whole-breast vascularity. AJR Am J Roentgenol. 2012; 199:921–928.
Article24. Bielenberg DR, Zetter BR. The contribution of angiogenesis to the process of metastasis. Cancer J. 2015; 21:267–273.
Article25. Li KL, Henry RG, Wilmes LJ, et al. Kinetic assessment of breast tumors using high spatial resolution signal enhancement ratio (SER) imaging. Magn Reson Med. 2007; 58:572–581.
Article26. Loiselle CR, Eby PR, Peacock S, Kim JN, Lehman CD. Dynamic contrast-enhanced magnetic resonance imaging and invasive breast cancer: primary lesion kinetics correlated with axillary lymph node extracapsular extension. J Magn Reson Imaging. 2011; 33:96–101.
Article27. Cichon MA, Degnim AC, Visscher DW, Radisky DC. Microenvironmental influences that drive progression from benign breast disease to invasive breast cancer. J Mammary Gland Biol Neoplasia. 2010; 15:389–397.
Article28. Uematsu T, Kasami M, Watanabe J. Is evaluation of the presence of prepectoral edema on T2-weighted with fat-suppression 3 T breast MRI a simple and readily available noninvasive technique for estimation of prognosis in patients with breast cancer? Breast Cancer. 2014; 21:684–692.29. Durur-Subasi I, Durur-Karakaya A, Karaman A, Seker M, Demirci E, Alper F. Is the necrosis/wall ADC ratio useful for the differentiation of benign and malignant breast lesions? Br J Radiol. 2017; 90:20160803.
Article30. Ahmed AR. HER2 expression is a strong independent predictor of nodal metastasis in breast cancer. J Egypt Natl Canc Inst. 2016; 28:219–227.
Article31. Dittrich A, Gautrey H, Browell D, Tyson-Capper A. The HER2 signaling network in breast cancer–like a spider in its web. J Mammary Gland Biol Neoplasia. 2014; 19:253–270.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Abbreviated Breast Magnetic Resonance Imaging: Background, Evidence From Studies, and Future Considerations
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- Metachronous Contralateral Axillary Lymph Node Metastasis from Invasive Breast Carcinoma: A Case Report with Imaging Findings
- Diagnostic value of magnetic resonance imaging using superparamagnetic iron oxide for axillary node metastasis in patients with breast cancer: a meta-analysis
- (18)F-FDG PET/CT with Contrast Enhancement for Evaluation of Axillary Lymph Node Involvement in T1 Breast Cancer