J Surg Ultrasound.
2020 May;7(1):1-6. 10.46268/jsu.2020.7.1.1.
Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- Affiliations
-
- 1Division of BreastㆍThyroid Surgery, Department of Surgery, Jeonbuk National University Medical School, Jeonju, Korea
- KMID: 2502952
- DOI: http://doi.org/10.46268/jsu.2020.7.1.1
Abstract
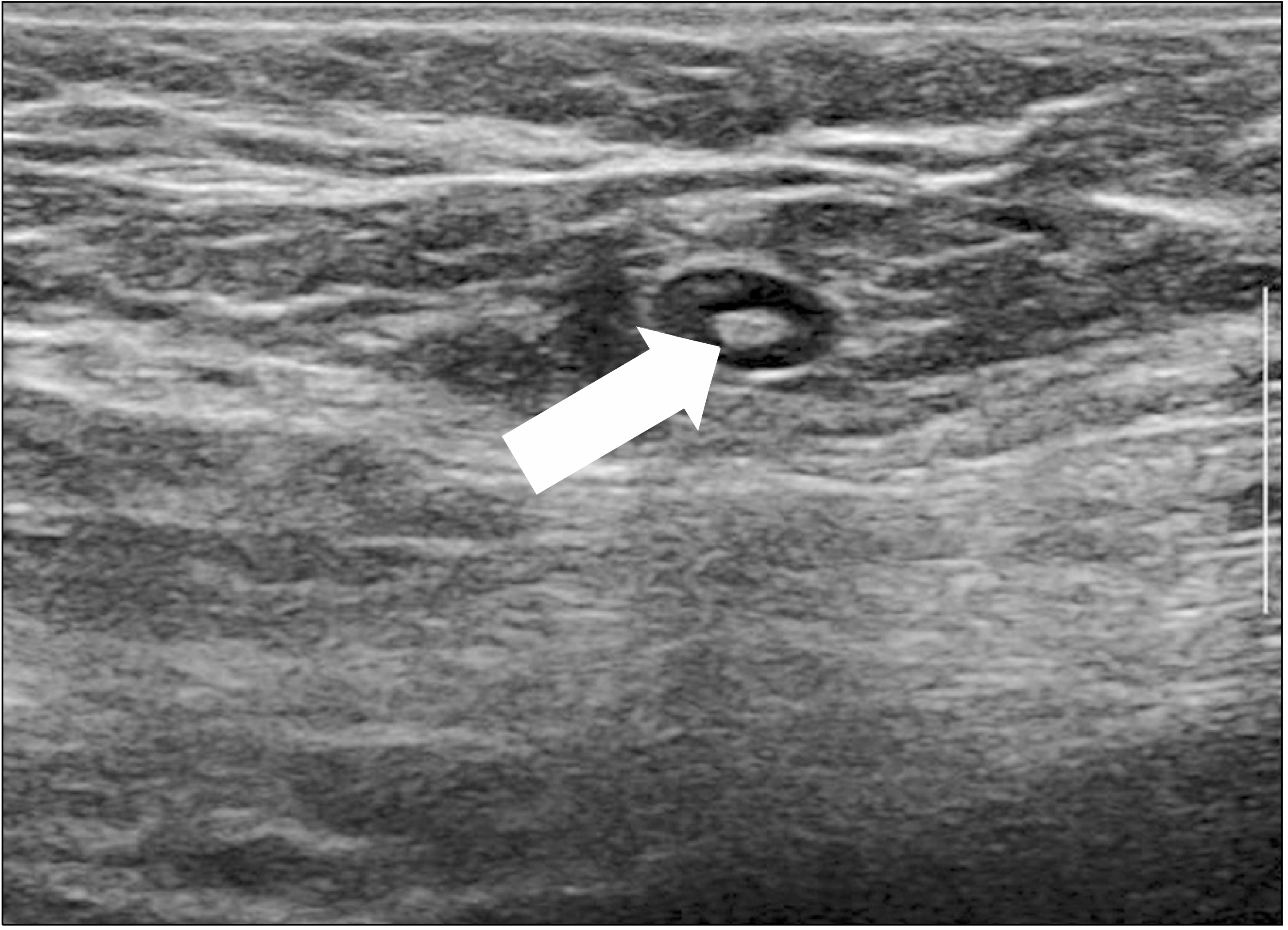
- The identification of axillary lymph node metastases in breast cancer patients is a critical factor in determining the stage, deciding the treatment modality, and predicting the prognosis. Over the years, axillary staging has evolved from a radical axillary lymph node dissection to a more conservative sentinel lymph node biopsy. The main goal of axillary imaging techniques is to identify metastatic lymph nodes with optimal accuracy, high enough to initially select patients for an upfront lymph node dissection. Features suggestive of an axillary lymph node metastasis may be seen with a range of imaging modalities. On the other hand, ultrasonography is the method of choice for evaluating the node morphology and allowing image- guided interventions of abnormal nodes. Gray-scale ultrasonography is not perfect on its own. Newer techniques, such as elastography or contrast-enhanced ultrasonography, have shown promise in identifying axillary lymph node metastases. This review provides a comprehensive overview of ultrasonography for an axillary lymph node assessment in breast cancer patients.
Keyword
Figure
Cited by 1 articles
-
Clinical Value of Axillary Ultrasonography in Breast Cancer with Lymph Node Metastases
Jung Ho Park, Hyun Ryung Kim, Sanghwa Kim, Young Ah Lim, Kyoonsoon Jung, Lee Su Kim
J Surg Ultrasound. 2021;8(2):41-47. doi: 10.46268/jsu.2021.8.2.41.
Reference
-
Fisher B., Bauer M., Wickerham DL., Redmond CK., Fisher ER., Cruz AB, et al. 1983. Relation of number of positive axillary nodes to the prognosis of patients with primary breast cancer. An NSABP update. Cancer. 52:1551–7. DOI: 10.1002/1097-0142(19831101)52:9<1551::AID-CNCR2820520902>3.0.CO;2-3.
ArticleCarlson GW., Wood WC. 2011. Management of axillary lymph node metastasis in breast cancer: making progress. JAMA. 305:606–7. DOI: 10.1001/jama.2011.131. PMID: 21304087.
ArticleHarlow SP., Krag DN., Julian TB., Ashikaga T., Weaver DL., Feldman SA, et al. 2005. Prerandomization surgical training for the national surgical adjuvant breast and bowel project (NSABP) B-32 trial: a randomized phase III clinical trial to compare sentinel node resection to conventional axillary dissection in clinically node-negative breast cancer. Ann Surg. 241:48–54. DOI: 10.1097/01.sla.0000149429.39656.94. PMID: 15621990. PMCID: PMC1356845.
ArticleLyman GH., Giuliano AE., Somerfield MR., Benson AB 3rd., Bodurka DC., Burstein HJ, et al. 2005. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol. 23:7703–20. DOI: 10.1200/JCO.2005.08.001. PMID: 16157938.
ArticleHumphrey KL., Saksena MA., Freer PE., Smith BL., Rafferty EA. 2014. To do or not to do: axillary nodal evaluation after ACOSOG Z0011 trial. Radiographics. 34:1807–16. DOI: 10.1148/rg.347130141. PMID: 25384280.
ArticleKim T., Giuliano AE., Lyman GH. 2006. Lymphatic mapping and sentinel lymph node biopsy in early-stage breast carcinoma: a metaanalysis. Cancer. 106:4–16. DOI: 10.1002/cncr.21568. PMID: 16329134.
ArticleBarthelmes L., Goyal A., Newcombe RG., McNeill F., Mansel RE. NEW START and ALMANAC Study Groups. 2010. Adverse reactions to patent blue V dye- The NEW START and ALMANAC experience. Eur J Surg Oncol. 36:399–403. DOI: 10.1016/j.ejso.2009.10.007. PMID: 19939618.
ArticleMarino MA., Avendano D., Zapata P., Riedl CC., Pinker K. 2020. Lymph node imaging in patients with primary breast cancer: concurrent diagnostic tools. Oncologist. 25:e231–42. DOI: 10.1634/theoncologist.2019-0427. PMID: 32043792. PMCID: PMC7011661.
ArticleManca G., Rubello D., Tardelli E., Giammarile F., Mazzarri S., Boni G, et al. 2016. Sentinel lymph node biopsy in breast cancer: indications, contraindications, and controversies. Clin Nucl Med. 41:126–33. DOI: 10.1097/RLU.0000000000000985. PMID: 26447368.Giuliano AE., Kirgan DM., Guenther JM., Morton DL. 1994. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Ann Surg. 220:391–8. discussion 398-401. DOI: 10.1097/00000658-199409000-00015. PMID: 8092905. PMCID: PMC1234400.
ArticleBedi DG., Krishnamurthy R., Krishnamurthy S., Edeiken BS., Le-Petross H., Fornage BD, et al. 2008. Cortical morphologic features of axillary lymph nodes as a predictor of metastasis in breast cancer: in vitro sonographic study. AJR Am J Roentgenol. 191:646–52. DOI: 10.2214/AJR.07.2460. PMID: 18716089.
ArticleEcanow JS., Abe H., Newstead GM., Ecanow DB., Jeske JM. 2013. Axillary staging of breast cancer: what the radiologist should know. Radiographics. 33:1589–612. DOI: 10.1148/rg.336125060. PMID: 24108553.
ArticleLowes S., Leaver A., Cox K., Satchithananda K., Cosgrove D., Lim A. 2018. Evolving imaging techniques for staging axillary lymph nodes in breast cancer. Clin Radiol. 73:396–409. DOI: 10.1016/j.crad.2018.01.003. PMID: 29439780.
ArticleCho N., Moon WK., Han W., Park IA., Cho J., Noh DY. 2009. Preoperative sonographic classification of axillary lymph nodes in patients with breast cancer: node-to-node correlation with surgical histology and sentinel node biopsy results. AJR Am J Roentgenol. 193:1731–7. DOI: 10.2214/AJR.09.3122. PMID: 19933672.
ArticleYang WT., Chang J., Metreweli C. 2000. Patients with breast cancer: differences in color Doppler flow and gray-scale US features of benign and malignant axillary lymph nodes. Radiology. 215:568–73. DOI: 10.1148/radiology.215.2.r00ap20568. PMID: 10796941.
ArticleLee B., Lim AK., Krell J., Satchithananda K., Coombes RC., Lewis JS, et al. 2013. The efficacy of axillary ultrasound in the detection of nodal metastasis in breast cancer. AJR Am J Roentgenol. 200:W314–20. DOI: 10.2214/AJR.12.9032. PMID: 23436877.
ArticleSidibé S., Coulibaly A., Traoré S., Touré M., Traoré I. 2007. [Role of ultrasonography in the diagnosis of axillary lymph node metastases in breast cancer: a systematic review]. Mali Med. 22:9–13. French. PMID: 19434975.Alvarez S., Añorbe E., Alcorta P., López F., Alonso I., Cortés J. 2006. Role of sonography in the diagnosis of axillary lymph node metastases in breast cancer: a systematic review. AJR Am J Roentgenol. 186:1342–8. DOI: 10.2214/AJR.05.0936. PMID: 16632729.
ArticleHoussami N., Ciatto S., Turner RM., Cody HS 3rd., Macaskill P. 2011. Preoperative ultrasound-guided needle biopsy of axillary nodes in invasive breast cancer: meta-analysis of its accuracy and utility in staging the axilla. Ann Surg. 254:243–51. DOI: 10.1097/SLA.0b013e31821f1564. PMID: 21597359.Rao R., Lilley L., Andrews V., Radford L., Ulissey M. 2009. Axillary staging by percutaneous biopsy: sensitivity of fine-needle aspiration versus core needle biopsy. Ann Surg Oncol. 16:1170–5. DOI: 10.1245/s10434-009-0421-9. PMID: 19263171.
ArticleGruber I., Hahn M., Fehm T., Hann von Weyhern C., Stäbler A., Winckelmann A, et al. 2012. Relevance and methods of interventional breast sonography in preoperative axillary lymph node staging. Ultraschall Med. 33:337–43. DOI: 10.1055/s-0031-1273317. PMID: 21618166.
ArticleQiu SQ., Zeng HC., Zhang F., Chen C., Huang WH., Pleijhuis RG, et al. 2016. A nomogram to predict the probability of axillary lymph node metastasis in early breast cancer patients with positive axillary ultrasound. Sci Rep. 6:21196. DOI: 10.1038/srep21196. PMID: 26875677. PMCID: PMC4753408.
ArticleBevilacqua JL., Kattan MW., Fey JV., Cody HS 3rd., Borgen PI., Van Zee KJ. 2007. Doctor, what are my chances of having a positive sentinel node? A validated nomogram for risk estimation. J Clin Oncol. 25:3670–9. DOI: 10.1200/JCO.2006.08.8013. PMID: 17664461.
ArticleAzmil A., Bansal GJ. 2018. Can nomograms predict preoperative axillary lymph node metastasis in patients with breast cancer to guide second look ultrasonography? J Ultrasound Med. 37:1447–53. DOI: 10.1002/jum.14485. PMID: 29152824.
ArticleFaruk T., Islam MK., Arefin S., Haq MZ. 2015. The journey of elastography: background, current status, and future possibilities in breast cancer diagnosis. Clin Breast Cancer. 15:313–24. DOI: 10.1016/j.clbc.2015.01.002. PMID: 25858446.
ArticleChang W., Jia W., Shi J., Yuan C., Zhang Y., Chen M. 2018. Role of elastography in axillary examination of patients with breast cancer. J Ultrasound Med. 37:699–707. DOI: 10.1002/jum.14538. PMID: 29344976.
ArticleLee SH., Chang JM., Cho N., Koo HR., Yi A., Kim SJ, et al. 2014. Practice guideline for the performance of breast ultrasound elastography. Ultrasonography. 33:3–10. DOI: 10.14366/usg.13012. PMID: 24936489. PMCID: PMC4058975.
ArticleWojcinski S., Dupont J., Schmidt W., Cassel M., Hillemanns P. 2012. Real-time ultrasound elastography in 180 axillary lymph nodes: elasticity distribution in healthy lymph nodes and prediction of breast cancer metastases. BMC Med Imaging. 12:35. DOI: 10.1186/1471-2342-12-35. PMID: 23253859. PMCID: PMC3536617.
ArticleYouk JH., Son EJ., Gweon HM., Kim H., Park YJ., Kim JA. 2014. Comparison of strain and shear wave elastography for the differentiation of benign from malignant breast lesions, combined with B-mode ultrasonography: qualitative and quantitative assessments. Ultrasound Med Biol. 40:2336–44. DOI: 10.1016/j.ultrasmedbio.2014.05.020. PMID: 25130444.
ArticleTourasse C., Dénier JF., Awada A., Gratadour AC., Nessah-Bousquet K., Gay J. 2012. Elastography in the assessment of sentinel lymph nodes prior to dissection. Eur J Radiol. 81:3154–9. DOI: 10.1016/j.ejrad.2012.04.031. PMID: 22656671.
ArticleYouk JH., Son EJ., Kim JA., Gweon HM. 2017. Pre-operative evaluation of axillary lymph node status in patients with suspected breast cancer using shear wave elastography. Ultrasound Med Biol. 43:1581–6. DOI: 10.1016/j.ultrasmedbio.2017.03.016. PMID: 28511961.
ArticleEvans A., Rauchhaus P., Whelehan P., Thomson K., Purdie CA., Jordan LB, et al. 2014. Does shear wave ultrasound independently predict axillary lymph node metastasis in women with invasive breast cancer? Breast Cancer Res Treat. 143:153–7. DOI: 10.1007/s10549-013-2747-z. PMID: 24305976. PMCID: PMC4363519.
ArticleSever A., Jones S., Cox K., Weeks J., Mills P., Jones P. 2009. Preoperative localization of sentinel lymph nodes using intradermal microbubbles and contrast-enhanced ultrasonography in patients with breast cancer. Br J Surg. 96:1295–9. DOI: 10.1002/bjs.6725. PMID: 19847869.
ArticleGoldberg BB., Merton DA., Liu JB., Thakur M., Murphy GF., Needleman L, et al. 2004. Sentinel lymph nodes in a swine model with melanoma: contrast-enhanced lymphatic US. Radiology. 230:727–34. DOI: 10.1148/radiol.2303021440. PMID: 14990839.
ArticleCox K., Weeks J., Mills P., Chalmers R., Devalia H., Fish D, et al. 2016. Contrast-enhanced ultrasound biopsy of sentinel lymph nodes in patients with breast cancer: implications for axillary metastases and conservation. Ann Surg Oncol. 23:58–64. DOI: 10.1245/s10434-015-4606-0. PMID: 25990967.
ArticleNielsen Moody A., Bull J., Culpan AM., Munyombwe T., Sharma N., Whitaker M, et al. 2017. Preoperative sentinel lymph node identification, biopsy and localisation using contrast enhanced ultrasound (CEUS) in patients with breast cancer: a systematic review and meta-analysis. Clin Radiol. 72:959–71. DOI: 10.1016/j.crad.2017.06.121. PMID: 28774472.
ArticleGentilini O., Veronesi U. 2012. Abandoning sentinel lymph node biopsy in early breast cancer? A new trial in progress at the European Institute of Oncology of Milan (SOUND: Sentinel node vs Observation after axillary UltraSouND). Breast. 21:678–81. DOI: 10.1016/j.breast.2012.06.013. PMID: 22835916.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Value of Axillary Ultrasonography in Breast Cancer with Lymph Node Metastases
- Ipsilateral Breast Tumor Recurrence with Metachronous Contralateral Axillary Lymph Node Metastasis after Breast-Conserving Surgery with Axillary Lymph Node Dissection
- Sentinel Lymph Node Imaging in Breast Cancer
- Accuracy of Radiological Axillary Staging for Breast Cancer Patients with Neoadjuvant Chemotherapy
- Short Term Follow-up Data in Breast Cancer Patients with Sentinel Lymph Node Biopsy Alone