Kosin Med J.
2018 Dec;33(3):297-306. 10.7180/kmj.2018.33.3.297.
Diagnostic value of magnetic resonance imaging using superparamagnetic iron oxide for axillary node metastasis in patients with breast cancer: a meta-analysis
- Affiliations
-
- 1Department of Surgery, College of Medicine, Kosin University, Busan, Korea. mammomaster@naver.com
- 2Department of Radiology, College of Medicine, Kosin University, Busan, Korea.
- KMID: 2442540
- DOI: http://doi.org/10.7180/kmj.2018.33.3.297
Abstract
OBJECTIVES
Identification of axillary metastases in breast cancer is important for staging disease and planning treatment, but current techniques are associated with a number of adverse events. This report evaluates the diagnostic accuracy of superparamagnetic iron oxide (SPIO)-enhanced magnetic resonance imaging (MRI) techniques for identification of axillary metastases in breast cancer patients.
METHODS
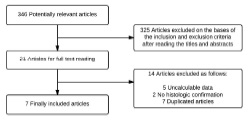
We performed a meta-analysis of previous studies that compared SPIO enhanced MRI with histological diagnosis after surgery or biopsy. We searched PubMed, Ovid, Springer Link, and Cochrane library to identify studies reporting data for SPIO enhanced MRI for detection of axillary lymph node metastases in breast cancer until December 2013. The following keywords were used: "magnetic resonance imaging AND axilla" and "superparamagnetic iron oxide AND axilla". Eligible studies were those that compared SPIO enhanced MRI with histological diagnosis. Sensitivity and specificity were calculated for every study; summary receiver operating characteristic and subgroup analyses were done. Study quality and heterogeneity were also assessed.
RESULTS
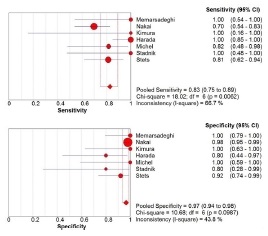
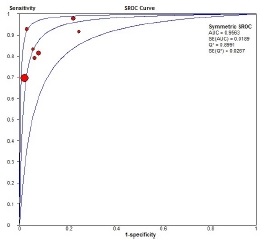
There were 7 publications that met the criteria for inclusion in our meta-analysis. SROC curve analysis for per patient data showed an overall sensitivity of 0.83 (95% Confidence interval (CI): 0.75-0.89) and overall specificity of 0.97 (95% CI: 0.94-0.98). Overall weighted area under the curve was 0.9563.
CONCLUSIONS
SPIO enhanced MRI showed a trend toward high diagnostic accuracy in detection of lymph node metastases for breast cancer. So, when the breast cancer patients has axillary metastases histologically, SPIO enhanced MRI may be effective diagnostic imaging modality for axillary metastases.
MeSH Terms
Figure
Reference
-
1. Banerjee M, George J, Song EY, Roy A, Hryniuk W. Tree-based model for breast cancer prognostication. J Clin Oncol. 2004; 22:2567–2575.
Article2. Cianfrocca M, Goldstein LJ. Prognostic and predictive factors in early-stage breast cancer. Oncologist. 2004; 9:606–616.
Article3. Fisher B, Bauer M, Wickerham DL, Redmond CK, Fisher ER, Cruz AB, et al. Relation of number of positive axillary nodes to the prognosis of patients with primary breast cancer. An NSABP update. Cancer. 1983; 52:1551–1557.
Article4. Wilking N, Rutqvist LE, Carstensen J, Mattsson A, Skoog L. Prognostic significance of axillary nodal status in primary breast cancer in relation to the number of resected nodes. Stockholm Breast Cancer Study Group. Acta Oncol. 1992; 31:29–35.
Article5. Swenson KK, Nissen MJ, Ceronsky C, Swenson L, Lee MW, Tuttle TM. Comparison of side effects between sentinel lymph node and axillary lymph node dissection for breast cancer. Ann Surg Oncol. 2002; 9:745–753.
Article6. Mansel RE, Fallowfield L, Kissin M, Goyal A, Newcombe RG, Dixon JM, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst. 2006; 98:599–609.
Article7. Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003; 349:546–553.
Article8. Liu CQ, Guo Y, Shi JY, Sheng Y. Late morbidity associated with a tumour-negative sentinel lymph node biopsy in primary breast cancer patients: a systematic review. Eur J Cancer. 2009; 45:1560–1568.
Article9. Robertson IJ, Hand F, Kell MR. FDG-PET/CT in the staging of local/regional metastases in breast cancer. Breast. 2011; 20:491–494.
Article10. Taylor K, O'Keeffe S, Britton PD, Wallis MG, Treece GM, Housden J, et al. Ultrasound elastography as an adjuvant to conventional ultrasound in the preoperative assessment of axillary lymph nodes in suspected breast cancer: a pilot study. Clin Radiol. 2011; 66:1064–1071.
Article11. Sianesi M, Ceci G, Ghirarduzzi A, Del Rio P, Guazzi A, Pisanelli B, et al. Use of axillary ultrasonography in breast cancer: a useful tool to reduce sentinel node procedures. Ann Ital Chir. 2009; 80:315–318.12. Cooper KL, Meng Y, Harnan S, Ward SE, Fitzgerald P, Papaioannou D, et al. Positron emission tomography (PET) and magnetic resonance imaging (MRI) for the assessment of axillary lymph node metastases in early breast cancer: systematic review and economic evaluation. Health Technol Assess. 2011; 15:iii–iiv. 1–134.
Article13. Ahmed M, Douek M. What is the future of magnetic nanoparticles in the axillary management of breast cancer? Breast Cancer Res Treat. 2014; 143:213–218.
Article14. Deserno WM, Harisinghani MG, Taupitz M, Jager GJ, Witjes JA, Mulders PF, et al. Urinary bladder cancer: preoperative nodal staging with ferumoxtran-10-enhanced MR imaging. Radiology. 2004; 233:449–456.
Article15. Keller TM, Michel SC, Fröhlich J, Fink D, Caduff R, Marincek B, et al. USPIO-enhanced MRI for preoperative staging of gynecological pelvic tumors: preliminary results. Eur Radiol. 2004; 14:937–944.
Article16. Koh DM, Brown G, Temple L, Raja A, Toomey P, Bett N, et al. Rectal cancer: mesorectal lymph nodes at MR imaging with USPIO versus histopathologic findings--initial observations. Radiology. 2004; 231:91–99.
Article17. Rockall AG, Sohaib SA, Harisinghani MG, Babar SA, Singh N, Jeyarajah AR, et al. Diagnostic performance of nanoparticle-enhanced magnetic resonance imaging in the diagnosis of lymph node metastases in patients with endometrial and cervical cancer. J Clin Oncol. 2005; 23:2813–2821.
Article18. Harisinghani MG, Barentsz J, Hahn PF, Deserno WM, Tabatabaei S, van de Kaa CH, et al. Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. N Engl J Med. 2003; 348:2491–2499.
Article19. Yezhelyev M, Yacoub R, O'Regan R. Inorganic nanoparticles for predictive oncology of breast cancer. Nanomedicine (Lond). 2009; 4:83–103.
Article20. Harada T, Tanigawa N, Matsuki M, Nohara T, Narabayashi I. Evaluation of lymph node metastases of breast cancer using ultrasmall superparamagnetic iron oxide-enhanced magnetic resonance imaging. Eur J Radiol. 2007; 63:401–407.
Article21. Motomura K, Ishitobi M, Komoike Y, Koyama H, Noguchi A, Sumino H, et al. SPIO-enhanced magnetic resonance imaging for the detection of metastases in sentinel nodes localized by computed tomography lymphography in patients with breast cancer. Ann Surg Oncol. 2011; 18:3422–3429.
Article22. Fleiss JL. Analysis of data from multiclinic trials. Control Clin Trials. 1986; 7:267–275.
Article23. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560.
Article24. Memarsadeghi M, Riedl CC, Kaneider A, Galid A, Rudas M, Matzek W, et al. Axillary lymph node metastases in patients with breast carcinomas: assessment with nonenhanced versus uspio-enhanced MR imaging. Radiology. 2006; 241:367–377.
Article25. Nakai G, Matsuki M, Harada T, Tanigawa N, Yamada T, Barentsz J, et al. Evaluation of axillary lymph nodes by diffusion-weighted MRI using ultrasmall superparamagnetic iron oxide in patients with breast cancer: initial clinical experience. J Magn Reson Imaging. 2011; 34:557–562.
Article26. Kimura K, Tanigawa N, Matsuki M, Nohara T, Iwamoto M, Sumiyoshi K, et al. High-resolution MR lymphography using ultrasmall superparamagnetic iron oxide (USPIO) in the evaluation of axillary lymph nodes in patients with early stage breast cancer: preliminary results. Breast cancer. 2010; 17:241–246.
Article27. Michel SC, Keller TM, Fröhlich JM, Fink D, Caduff R, Seifert B, et al. Preoperative breast cancer staging: MR imaging of the axilla with ultrasmall superparamagnetic iron oxide enhancement. Radiology. 2002; 225:527–536.
Article28. Stadnik TW, Everaert H, Makkat S, Sacré R, Lamote J, Bourgain C. Breast imaging. Preoperative breast cancer staging: comparison of USPIO-enhanced MR imaging and 18F-fluorodeoxyglucose (FDC) positron emission tomography (PET) imaging for axillary lymph node staging--initial findings. Eur Radiol. 2006; 16:2153–2160.
Article29. Stets C, Brandt S, Wallis F, Buchmann J, Gilbert FJ, Heywang-Köbrunner SH. Axillary lymph node metastases: a statistical analysis of various parameters in MRI with USPIO. J Magn Reson Imaging. 2002; 16:60–68.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diagnostic Effectiveness of USPIO versus Gadolinium Based MRI for Axillary Metastasis in Breast Cancer: A Meta-analysis
- Metachronous Contralateral Axillary Lymph Node Metastasis from Invasive Breast Carcinoma: A Case Report with Imaging Findings
- Cancer -Targeted MR Molecular Imaging
- Focal Nodular Hyperplasia of the Liver: Imaging Findings with Emphasis on the Findings of Superparamagnetic Iron Oxide-enhanced MR Imaging
- Clinical Significance of Preoperative Magnetic Resonance Imaging in Staging of Rectal Cancer