J Korean Acad Nurs.
2019 Jun;49(3):340-348. 10.4040/jkan.2019.49.3.340.
Nutritional Status of Liver Transplantation Recipients and Factors Influencing Nutritional Status
- Affiliations
-
- 1College of Nursing, Seoul National University, Seoul, Korea. smi@snu.ac.kr
- KMID: 2451301
- DOI: http://doi.org/10.4040/jkan.2019.49.3.340
Abstract
- PURPOSE
This study aimed to investigate the nutritional status of liver transplantation (LT) recipients and explore certain factors that influence nutritional status, including dietary patterns and physical activities.
METHODS
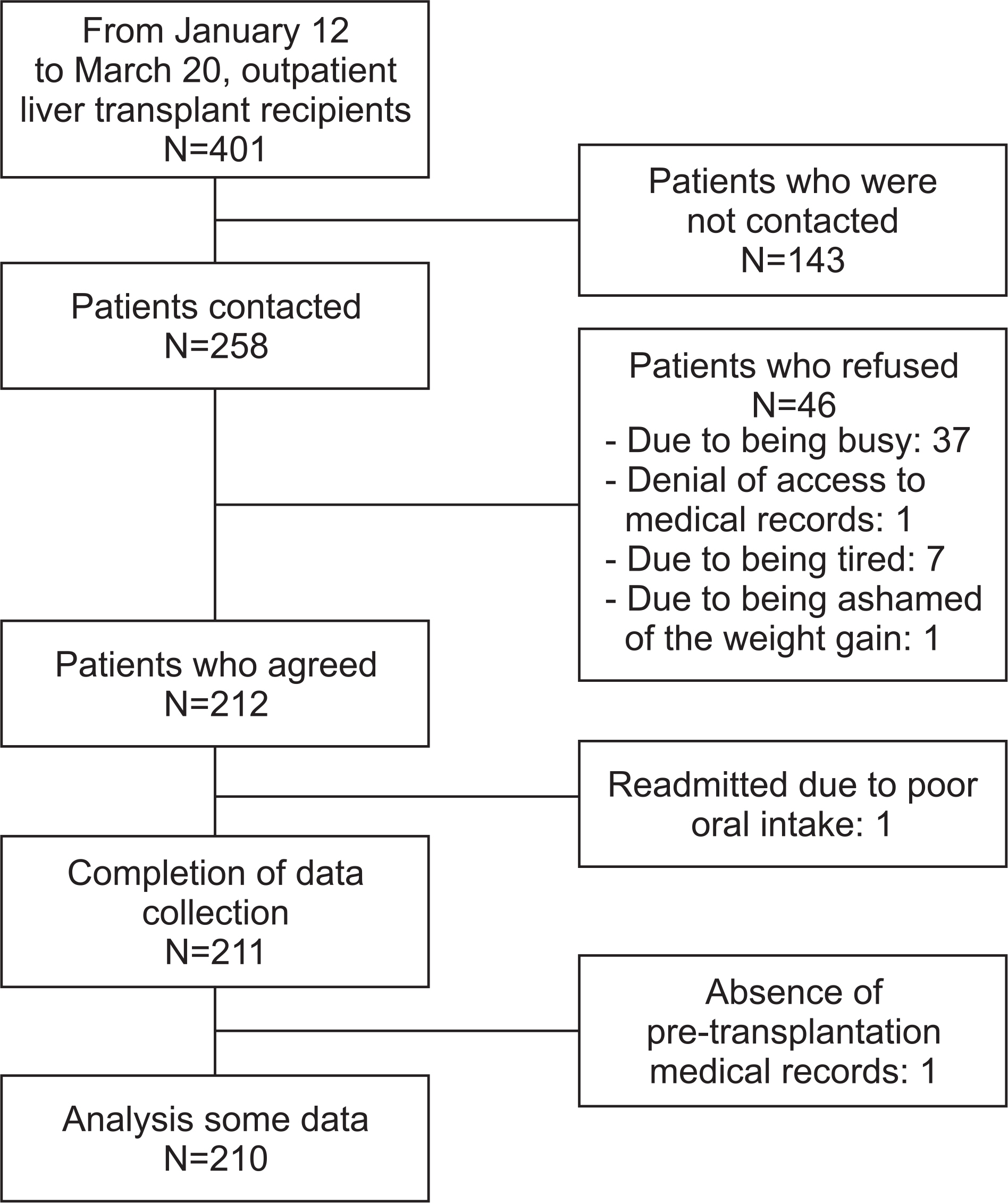
This was a cross-sectional, descriptive study. The subjects included 211 LT recipients at a medical center outpatient clinic located in Seoul, Korea. The nutritional status, dietary patterns, and physical activities of each subject were measured using the body mass index (BMI), Mini Dietary Assessment (MDA), and Global Physical Activity Questionnaire. Independent t-test, one-way analysis of variance, and multiple linear regression analysis were used to analyze the data.
RESULTS
The percentages of living and deceased donor LTs were 81.0% and 19.0%, respectively. The mean BMIs pre- and post-LT were 23.88 and 23.16 kg/m2, respectively, and the average MDA score was 36.55. More than 60.0% of the subjects had a moderate or high level of physical activity. In multivariate analysis, a higher BMI before LT (β=.72, p<.001), a lower Model for End-stage Liver Disease (MELD) score (β=−.18, p<.001), and being male (β=−.10, p=.024) contributed to better nutritional status post-LT. Patients within six months of LT were less engaged in muscle exercises than those post six months of LT (p=.020).
CONCLUSION
LT recipients in Korea have good nutritional status and a good level of physical activity. To improve recipients' post-LT nutritional status, the pre-LT nutritional status should be considered, particularly in those with a higher MELD score. In addition, physical activity including muscle-strengthening exercises should be encouraged from an earlier stage.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Reuben A. Long‐term management of the liver transplant patient: Diabetes, hyperlipidemia, and obesity. Liver Transplantation. 2001; 7(11B):S13–S21. https://doi.org/10.1053/jlts.2001.29167.
Article2. Moon M, Yi NJ. Nutrition support in liver transplantation patients. Journal of Clinical Nutrition. 2013; 5(1):20–23. https://doi.org/10.15747/jcn.2013.5.1.20.
Article3. Plauth M, Bernal W, Dasarathy S, Merli M, Plank LD, Schütz T, et al. ESPEN guideline on clinical nutrition in liver disease. Clinical Nutrition. 2019; 38(2):485–521. https://doi.org/10.1016/j.clnu.2018.12.022.
Article4. Anastácio LR, Davisson Correia MIT. Nutrition therapy: Integral part of liver transplant care. World Journal of Gastroenterology. 2016; 22(4):1513–1522. https://doi.org/10.3748/wjg.v22.i4.1513.
Article5. Korean Society for the Study of Obesity. Diagnosis and evaluation of obesity [Internet]. Seoul: Korean Society for the Study of Obesity;c2017. [cited 2017 Sep 2]. Available from:. http://www.kosso.or.kr/general/general/sub02.html/.6. Plank LD, Russell K. Nutrition in liver transplantation: Too little or too much? Current Opinion in Clinical Nutrition and Metabolic Care. 2015; 18(5):501–507. https://doi.org/10.1097/MCO.0000000000000205.7. Masuda T, Shirabe K, Ikegami T, Harimoto N, Yoshizumi T, Soejima Y, et al. Sarcopenia is a prognostic factor in living donor liver transplantation. Liver Transplantation. 2014; 20(4):401–407. https://doi.org/10.1002/lt.23811.
Article8. Merli M, Giusto M, Giannelli V, Lucidi C, Riggio O. Nutritional status and liver transplantation. Journal of Clinical and Experimental Hepatology. 2011; 1(3):190–198. https://doi.org/10.1016/s0973-6883(11)60237-5.
Article9. De Carvalho L, Parise ER, Samuel D. Factors associated with nutritional status in liver transplant patients who survived the first year after transplantation. Journal of Gastroenterology and Hepatology. 2010; 25(2):391–396. https://doi.org/10.1111/j.1440-1746.2009.06033.x.
Article10. Richards J, Gunson B, Johnson J, Neuberger J. Weight gain and obesity after liver transplantation. Transplant International. 2005; 18(4):461–466. https://doi.org/10.1111/j.1432-2277.2004.00067.x.
Article11. Chen CL, Kabiling CS, Concejero AM. Why does living donor liver transplantation flourish in Asia? Nature Reviews Gastro- enterology & Hepatology. 2013; 10(12):746–751. https://doi.org/10.1038/nrgastro.2013.194.
Article12. Lee SG. Current status of liver transplantation in Korea. The Korean Society of Gastroenterology. 2005; 46(2):75–83.13. Lim HS, Kim HC, Park YH, Kim SK. Evaluation of malnutrition risk after liver transplantation using nutritional screening tools. Clinical Nutrition Research. 2015; 4(4):242–249. https://doi.org/10.7762/cnr.2015.4.4.242.14. Korean Network for Organ Sharing (KONOS). Organ transplantation and donation of human tissue statistical yearbook2017. Sejong: Ministry of Health and Welfare;2018. Aug. Report No.: 11-1351155-000001-10.15. Kim WY, Cho MS, Lee HS. Development and validation of mini dietary assessment index for Koreans. The Korean Nutrition Society. 2003; 36(1):83–92.16. Lee B, Kim YM, Kim YJ, Seo EO, Lee DG, Lee SH, et al. The relationship of health behaviors and residence types of university students. The Journal of the Korean Society of School Health. 2012; 25(1):77–84.17. Lee S, Kim Y, Seo S, Cho MS. A study on dietary habits and food intakes in adults aged 50 or older according to depression status. Journal of Nutrition and Health. 2014; 47(1):67–76. https://doi.org/10.4163/jnh.2014.47.1.67.
Article18. Bull FC, Maslin TS, Armstrong T. Global Physical Activity Questionnaire (GPAQ): Nine country reliability and validity study. Journal of Physical Activity and Health. 2009; 6(6):790–804. https://doi.org/10.1123/jpah.6.6.790.
Article19. Lee C. Reliability and validity of the global physical activity questionnaire of Korean version [master’s thesis]. Seoul: Yonsei University;2014. p. 1–81.20. Korea Centers for Disease Control & Prevention (KCDC). Korea Health Statistics 2016: Korea National Health and Nutrition Examination Survey. Sejong: Ministry of Health and Welfare;2017. Dec. Report No.: 11-1351159-000027-10.21. Pasqua IC, Moreno CR. The nutritional status and eating habits of shift workers: A chronobiological approach. Chronobiology International. 2004; 21(6):949–960.
Article22. Bogacka A, Sobczak-Czynsz A, Kucharska E, Madaj M, Stucka K. Analysis of nutrition and nutritional status of haemodialysis patients. Roczniki Państwowego Zakładu Higieny. 2018; 69(2):165–174.23. Cheung A, Levitsky J. Follow-up of the post-liver transplantation patient: A primer for the practicing gastroenterologist. Clinics in Liver Disease. 2017; 21(4):793–813. https://doi.org/10.1016/j.cld.2017.06.006.24. Sharma P, Goodrich NP, Schaubel DE, Smith AR, Merion RM. National assessment of early hospitalization after liver transplantation: Risk factors and association with patient survival. Liver Transplantation. 2017; 23(9):1143–1152. https://doi.org/10.1002/lt.24813.
Article25. Kim H, Choi M, Kim SS, Kim SI. Self-care, social support, and biological markers in liver transplant recipients. Korean Journal of Adult Nursing. 2015; 27(2):170–179. https://doi.org/10.7475/kjan.2015.27.2.170.
Article26. Miller CM, Quintini C, Dhawan A, Durand F, Heimbach JK, Kim-Schluger HL, et al. The International Liver Transplantation Society living donor liver transplant recipient guideline. Transplantation. 2017; 101(5):938–944. https://doi.org/10.1097/TP.0000000000001571.
Article27. Sanchez AJ, Aranda‐Michel J. Nutrition for the liver transplant patient. Liver Transplantation. 2006; 12(9):1310–1316. https://doi.org/10.1002/lt.20894.
Article28. Ferreira LG, Santos LF, Anastácio LR, Lima AS, Correia MI. Resting energy expenditure, body composition, and dietary intake: A longitudinal study before and after liver transplantation. Transplantation. 2013; 96(6):579–585. https://doi.org/10.1097/TP.0b013e31829d924e.29. Lunati ME, Grancini V, Agnelli F, Gatti S, Masserini B, Zim-balatti D, et al. Metabolic syndrome after liver transplantation: Short-term prevalence and pre- and post-operative risk factors. Digestive and Liver Disease. 2013; 45(10):833–839. https://doi.org/10.1016/j.dld.2013.03.009.
Article30. Sarkar M, Watt KD, Terrault N, Berenguer M. Outcomes in liver transplantation: Does sex matter? Journal of Hepatology. 2015; 62(4):946–955. https://doi.org/10.1016/j.jhep.2014.11.023.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perioperative nutritional management to improve long-term outcomes in critically ill perioperative organ transplant patients: a narrative review
- Changes in health status of North Korean children and emerging health challenges of North Korean refugee children
- Association between nutritional status, sarcopenia, and frailty in rural elders
- Influence of Frailty, Nutritional Status, Positive Thinking and Family Function on Health Conservation of the Elderly at Home
- Nutritional Supplementation in Stroke Rehabilitation: A Narrative Review