Ann Surg Treat Res.
2019 Jul;97(1):21-26. 10.4174/astr.2019.97.1.21.
Minimally-invasive neonatal surgery: laparoscopic excision of choledochal cysts in neonates
- Affiliations
-
- 1Department of Pediatric Surgery, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea. namgoong2940@naver.com
- 2Department of Pediatric Surgery, Chonnam National University Children's Hospital, Chonnam National University School of Medicine, Gwangju, Korea.
- KMID: 2450986
- DOI: http://doi.org/10.4174/astr.2019.97.1.21
Abstract
- PURPOSE
Improvements in surgical techniques and a better understanding of the unique anesthetic requirements in neonates undergoing laparoscopy have suggested that laparoscopic surgery may be effective in newborns. This study therefore evaluated the safety and feasibility of laparoscopic excision of the cyst (LEC) in neonates.
METHODS
This retrospective study included 43 neonates who underwent excision of choledochal cysts between November, 2001, and January, 2018, including 21 who underwent open excision and 22 who underwent LEC. Their perioperative and surgical outcomes were reviewed. The patients were followed up for a median 37 months (range, 3-141 months).
RESULTS
Baseline characteristics did not differ significantly in the open and LEC groups. Mean intraoperative peak partial pressure of arterial CO2 (PaCO2) (45.5 mmHg vs. 48.0 mmHg) and total operation time (208.3 ± 71.0 minutes vs. 235.0 ± 47.2 minutes) were similar in both groups. Parents of the patients in the LEC group provided a more positive evaluation of scar scale and greater satisfaction with wound. No patient in either group experienced any critical complications. Three patients in the open excision group required readmission for cholangitis and 2 patients had ileus. No patient in the laparoscopic excision group experienced any postoperative complications during follow-up.
CONCLUSION
Despite difficulties performing laparoscopic surgery in neonates, LEC was safe and feasible when intraperitoneal peak pressure was maintained under 10 mmHg and PaCOâ‚‚ was closely monitored by a pediatric anesthesiologist. Compared with open excision, LEC provided improved cosmetic outcomes without severe complications. Prospective randomized studies with large numbers of patients are warranted.
MeSH Terms
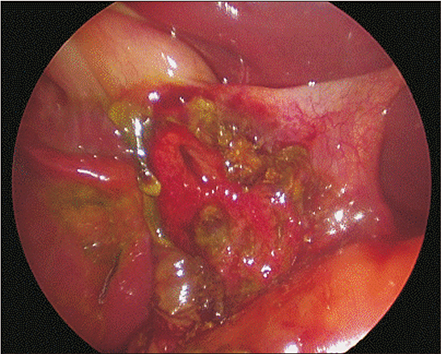
Figure
Cited by 1 articles
-
Clinical comparison between the presence and absence of protein plugs in pediatric choledochal cysts: experience in 390 patients over 30 years in a single center
Chaeyoun Oh, Jong-Ho Cheun, Hyun-Young Kim
Ann Surg Treat Res. 2021;101(5):306-313. doi: 10.4174/astr.2021.101.5.306.
Reference
-
1. Miyano T, Yamataka A, Kato Y, Segawa O, Lane G, Takamizawa S, et al. Hepaticoenterostomy after excision of choledochal cyst in children: a 30-year experience with 180 cases. J Pediatr Surg. 1996; 31:1417–1421.
Article2. Miyano T, Yamataka A, Li L. Congenital biliary dilatation. Semin Pediatr Surg. 2000; 9:187–195.
Article3. Ohi R, Yaoita S, Kamiyama T, Ibrahim M, Hayashi Y, Chiba T. Surgical treatment of congenital dilatation of the bile duct with special reference to late complications after total excisional operation. J Pediatr Surg. 1990; 25:613–617.
Article4. Farello GA, Cerofolini A, Rebonato M, Bergamaschi G, Ferrari C, Chiappetta A. Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc. 1995; 5:354–358.5. Li L, Feng W, Jing-Bo F, Qi-Zhi Y, Gang L, Liu-Ming H, et al. Laparoscopic-assisted total cyst excision of choledochal cyst and Roux-en-Y hepatoenterostomy. J Pediatr Surg. 2004; 39:1663–1666.
Article6. Li L, Liu SL, Hou WY, Cui L, Liu XL, Jun Z, et al. Laparoscopic correction of biliary duct stenosis in choledochal cyst. J Pediatr Surg. 2008; 43:644–646.
Article7. Lima M, Gargano T, Ruggeri G, Destro F, Maffi M. Laparoscopic treatment of congenital choledochal cyst and hepaticojejunostomy with extracorporeal Roux-en-Y anastomosis: technical aspects and early experience with three cases. Pediatr Med Chir. 2016; 38:125.
Article8. Diao M, Li L, Cheng W. Laparoscopic versus Open Roux-en-Y hepatojejunostomy for children with choledochal cysts: intermediate-term follow-up results. Surg Endosc. 2011; 25:1567–1573.
Article9. Liuming H, Hongwu Z, Gang L, Jun J, Wenying H, Wong KK, et al. The effect of laparoscopic excision vs open excision in children with choledochal cyst: a midterm follow-up study. J Pediatr Surg. 2011; 46:662–665.
Article10. Qiao G, Li L, Li S, Tang S, Wang B, Xi H, et al. Laparoscopic cyst excision and Roux-Y hepaticojejunostomy for children with choledochal cysts in China: a multicenter study. Surg Endosc. 2015; 29:140–144.
Article11. Fujimoto T, Segawa O, Lane GJ, Esaki S, Miyano T. Laparoscopic surgery in newborn infants. Surg Endosc. 1999; 13:773–777.
Article12. Gueugniaud PY, Abisseror M, Moussa M, Godard J, Foussat C, Petit P, et al. The hemodynamic effects of pneumoperitoneum during laparoscopic surgery in healthy infants: assessment by continuous esophageal aortic blood flow echo-Doppler. Anesth Analg. 1998; 86:290–293.13. O'Neill JA Jr. Choledochal cyst. Curr Probl Surg. 1992; 29:361–410.14. Chen CJ. Clinical and operative findings of choledochal cysts in neonates and infants differ from those in older children. Asian J Surg. 2003; 26:213–217.
Article15. Liu SL, Li L, Hou WY, Zhang J, Huang LM, Li X, et al. Laparoscopic excision of choledochal cyst and Roux-en-Y hepaticojejunostomy in symptomatic neonates. J Pediatr Surg. 2009; 44:508–511.
Article16. Saito T, Terui K, Mitsunaga T, Nakata M, Kuriyama Y, Higashimoto Y, et al. Role of pediatric endoscopic retrograde cholangiopancreatography in an era stressing less-invasive imaging modalities. J Pediatr Gastroenterol Nutr. 2014; 59:204–209.
Article17. Lee H, Hirose S, Bratton B, Farmer D. Initial experience with complex laparoscopic biliary surgery in children: biliary atresia and choledochal cyst. J Pediatr Surg. 2004; 39:804–807.
Article18. Ure BM, Schier F, Schmidt AI, Nustede R, Petersen C, Jesch NK. Laparoscopic resection of congenital choledochal cyst, choledochojejunostomy, and extraabdominal Roux-en-Y anastomosis. Surg Endosc. 2005; 19:1055–1057.
Article19. Thome UH, Ambalavanan N. Permissive hypercapnia to decrease lung injury in ventilated preterm neonates. Semin Fetal Neonatal Med. 2009; 14:21–27.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally invasive surgery for choledochal cysts: Laparoscopic versus robotic approaches
- A case of laparoscopic excision of choledochal cyst, hepaticojejunostomy, and Roux-en-Y anastomosis using Artisential®
- Comparison of surgical outcomes of intracorporeal hepaticojejunostomy in the excision of choledochal cysts using laparoscopic versus robot techniques
- Laparoscopic Choledochal Cyst Excision and Hepaticojejunostomy: A Case Series
- Robot-assisted Excision of a Huge Choledochal Cyst and Roux-en-Y Hepaticojejunostomy using the da Vinci(TM) Surgical System