Comparison of surgical outcomes of intracorporeal hepaticojejunostomy in the excision of choledochal cysts using laparoscopic versus robot techniques
- Affiliations
-
- 1Department of Surgery and Cancer Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. jangjy4@snu.ac.kr
- KMID: 2407748
- DOI: http://doi.org/10.4174/astr.2018.94.4.190
Abstract
- PURPOSE
Increasing surgical expertise in minimally invasive surgery has allowed laparoscopic surgery to be performed in many abdominal surgeries. Laparoscopic choledochal cyst excision and Roux-en-Y hepaticojejunostomy are challenging and sophisticated surgeries because of the difficult anastomosis. Recent advances in robotic surgery have enabled more delicate and precise movements, and Endowrist instruments allow for securing sutures during anastomosis. This study aimed to compare surgical outcomes of laparoscopic and robotic hepaticojejunostomy in choledochal cyst excision.
METHODS
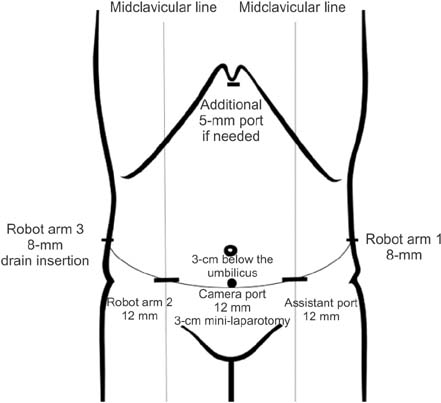
Sixty-seven patients who underwent laparoscopic or robotic-hybrid choledochal cyst excision from 2004 to 2016 were retrospectively analyzed and compared. In robotic surgery, dissection was performed laparoscopically, and hepaticojejunostomy was performed using a robotic platform.
RESULTS
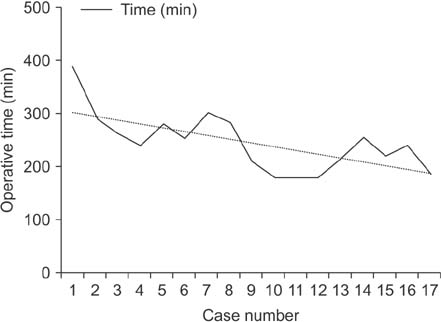
The mean operative time was significantly longer in robotic surgery than in laparoscopic surgery (247.94 ± 54.14 minutes vs. 181.31 ± 43.06 minutes, P < 0.05). The mean estimated blood loss (108.71 ± 15.53 mL vs. 172.78 ± 117.46 mL, respectively, P = 0.097) and postoperative hospital stay (7.33 ± 2.96 days vs. 6.22 ± 1.06 days, P = 0.128) were comparable between procedures. Compared to the laparoscopic approaches, robotic surgery had significantly less short-term complications (22.4% vs. 0%, P = 0.029). There were more biliary leakage (n = 7, 14.3%) observed during the first 30 days after surgery in laparoscopy while none were observed in the robotic method.
CONCLUSION
Robotic surgery allow for more precise and secure sutures during anastomosis thereby reducing biliary complications. With expanding knowledge and expertise, robotic surgery may offer more advantages over laparoscopy in the era of minimally invasive surgery.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Minimally invasive surgery for choledochal cysts: Laparoscopic versus robotic approaches
Jong Hwi Yoon, Ho Kyoung Hwang, Woo Jung Lee, Chang Moo Kang
Ann Hepatobiliary Pancreat Surg. 2021;25(1):71-77. doi: 10.14701/ahbps.2021.25.1.71.Clinical characteristics of patients with malignancy and long-term outcomes of surgical treatment of patients with choledochal cyst
Wung Sun Han, Hongbeom Kim, Hee Ju Sohn, Mirang Lee, Yoon Hyung Kang, Hyeong Seok Kim, Youngmin Han, Jae-Seung Kang, Wooil Kwon, Jin-Young Jang
Ann Surg Treat Res. 2021;101(6):332-339. doi: 10.4174/astr.2021.101.6.332.A case of laparoscopic excision of choledochal cyst, hepaticojejunostomy, and Roux-en-Y anastomosis using Artisential®
Younghoon Shim, Chang Moo Kang
Ann Hepatobiliary Pancreat Surg. 2024;28(2):266-269. doi: 10.14701/ahbps.23-114.
Reference
-
1. Wiseman K, Buczkowski AK, Chung SW, Francoeur J, Schaeffer D, Scudamore CH. Epidemiology, presentation, diagnosis, and outcomes of choledochal cysts in adults in an urban environment. Am J Surg. 2005; 189:527–531.
Article2. Lee SE, Jang JY, Lee YJ, Choi DW, Lee WJ, Cho BH, et al. Choledochal cyst and associated malignant tumors in adults: a multicenter survey in South Korea. Arch Surg. 2011; 146:1178–1184.3. Sastry AV, Abbadessa B, Wayne MG, Steele JG, Cooperman AM. What is the incidence of biliary carcinoma in choledochal cysts, when do they develop, and how should it affect management. World J Surg. 2015; 39:487–492.
Article4. Urushihara N, Fukuzawa H, Fukumoto K, Sugiyama A, Nagae H, Watanabe K, et al. Totally laparoscopic management of choledochal cyst: Roux-en-Y Jejunojejunostomy and wide hepaticojejunostomy with hilar ductoplasty. J Laparoendosc Adv Surg Tech A. 2011; 21:361–366.
Article5. Jang JY, Kim SW, Han HS, Yoon YS, Han SS, Park YH. Totally laparoscopic management of choledochal cysts using a four-hole method. Surg Endosc. 2006; 20:1762–1765.
Article6. Tang ST, Yang Y, Wang Y, Mao YZ, Li SW, Tong QS, et al. Laparoscopic choledochal cyst excision, hepaticojejunostomy, and extracorporeal Roux-en-Y anastomosis: a technical skill and intermediate-term report in 62 cases. Surg Endosc. 2011; 25:416–422.
Article7. Jang JY, Yoon YS, Kang MJ, Kwon W, Park JW, Chang YR, et al. Laparoscopic excision of a choledochal cyst in 82 consecutive patients. Surg Endosc. 2013; 27:1648–1652.
Article8. Tanaka M, Shimizu S, Mizumoto K, Yokohata K, Chijiiwa K, Yamaguchi K, et al. Laparoscopically assisted resection of choledochal cyst and Roux-en-Y reconstruction. Surg Endosc. 2001; 15:545–552.
Article9. Senthilnathan P, Patel ND, Nair AS, Nalankilli VP, Vijay A, Palanivelu C. Laparoscopic management of choledochal cysttechnical modifications and outcome analysis. World J Surg. 2015; 39:2550–2556.
Article10. Hwang DW, Lee JH, Lee SY, Song DK, Hwang JW, Park KM, et al. Early experience of laparoscopic complete en bloc excision for choledochal cysts in adults. Surg Endosc. 2012; 26:3324–3329.
Article11. Palanivelu C, Rangarajan M, Parthasarathi R, Amar V, Senthilnathan P. Laparoscopic management of choledochal cysts: technique and utcomes: a retrospective study of 35 patients from a tertiary center. J Am Coll Surg. 2008; 207:839–846.12. Margonis GA, Spolverato G, Kim Y, Marques H, Poultsides G, Maithel S, et al. Minimally invasive resection of choledochal cyst: a feasible and safe surgical option. J Gastrointest Surg. 2015; 19:858–865.
Article13. Akaraviputh T, Trakarnsanga A, Suksamanapun N. Robot-assisted completeexcision of choledochal cyst type I, hepaticojejunostomy and extracorporealRoux-en-y anastomosis: a case report and review literature. World J Surg Oncol. 2010; 8:87.
Article14. Kang CM, Chi HS, Kim JY, Choi GH, Kim KS, Choi JS, et al. A case of robot-assisted excision of choledochal cyst, hepaticojejunostomy, andextracorporeal Roux-en-y anastomosis using the da Vinci surgical system. Surg Laparosc Endosc Percutan Tech. 2007; 17:538–541.15. Choi SB, Choi SY. Current status and future perspective of laparoscopic surgery in hepatobiliary disease. Kaohsiung J Med Sci. 2016; 32:281–291.
Article16. Farello GA, Cerofolini A, Rebonato M, Bergamaschi G, Ferrari C, Chiappetta A. Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc. 1995; 5:354–358.17. Stefanidis D, Wang F, Korndorffer JR Jr, Dunne JB, Scott DJ. Roboticassistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg Endosc. 2010; 24:377–382.18. Moorthy K, Munz Y, Dosis A, Hernandez J, Martin S, Bello F, et al. Dexterity enhancement with robotic surgery. Surg Endosc. 2004; 18:790–795.
Article19. Heemskerk J, van Gemert WG, de Vries J, Greve J, Bouvy ND. Learning curves of robot-assisted laparoscopic surgery compared with conventional laparoscopic surgery: an experimental study evaluating skill acquisition of robotassisted laparoscopic tasks compared with conventional laparoscopic tasks in inexperienced users. Surg Laparosc Endosc Percutan Tech. 2007; 17:171–174.20. Jung M, Morel P, Buehler L, Buchs NC, Hagen ME. Robotic general surgery: current practice, evidence, and perspective. Langenbecks Arch Surg. 2015; 400:283–292.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of laparoscopic excision of choledochal cyst, hepaticojejunostomy, and Roux-en-Y anastomosis using Artisential®
- Robot-assisted Excision of a Huge Choledochal Cyst and Roux-en-Y Hepaticojejunostomy using the da Vinci(TM) Surgical System
- Initial Experience of Robot-assisted Resection of Choledochal Cyst in Children
- Comparison of long-term biliary complications between open and laparoscopic choledochal cyst excision in children
- Early Experience of Laparoscopic Management of Choledochal Cyst