Infect Chemother.
2019 Jun;51(2):177-182. 10.3947/ic.2019.51.2.177.
Nosocomial Outbreak Caused by NDM-5 and OXA-181 Carbapenemase Co-producing Escherichia coli
- Affiliations
-
- 1Department of Laboratory Medicine, Yonsei University Wonju College of Medicine, Wonju Severance Christian Hospital, Wonju, Korea. u931018@yonsei.ac.kr
- 2Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju Severance Christian Hospital, Wonju, Korea. hyksos@yonsei.ac.kr
- 3Infection Control Department, Yonsei University Wonju College of Medicine, Wonju Severance Christian Hospital, Wonju, Korea.
- 4Department of Laboratory Medicine and Research Institute of Antimicrobial Resistance, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2450874
- DOI: http://doi.org/10.3947/ic.2019.51.2.177
Abstract
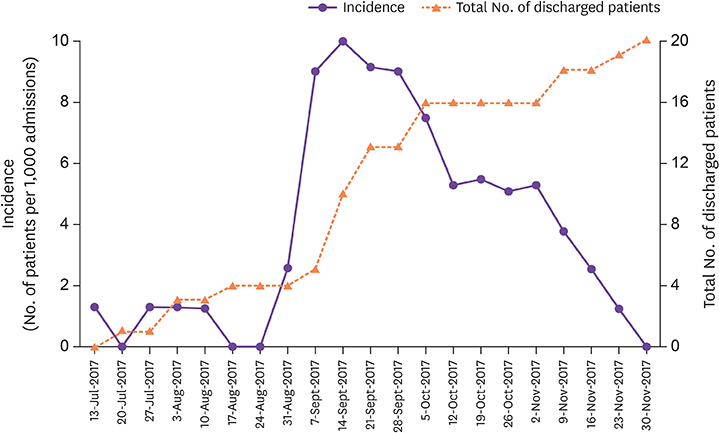
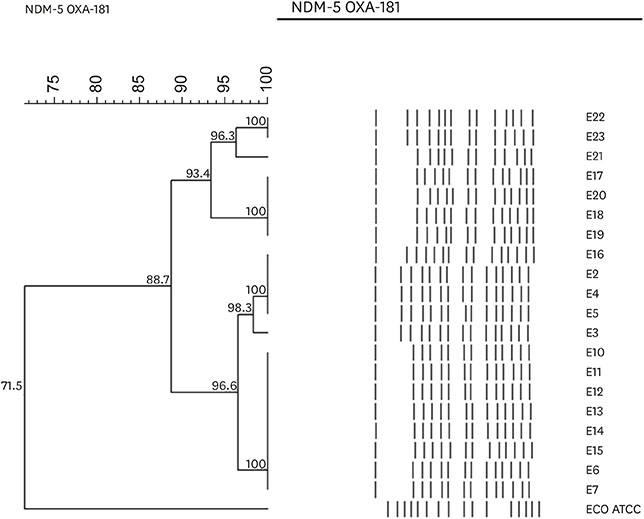
- Carbapenemase-producing Enterobacteriaceae (CPE) is an important and increasing threat to global health. From July to September 2017, 20 inpatients at a tertiary care hospital in Korea were either colonized or infected with carbapenem-resistant Escherichia coli strains. All of E. coli isolates co-produced bla(NDM-5) and bla(OXA-181) carbapenemase genes and shared ≥88% clonal relatedness on the basis of a cladistic calculation of the distribution of pulsed-field gel electrophoresis patterns. Rapid detection of CPE is one of the most important factors to prevent CPE dissemination because it takes long time for CPE to become negative.
Keyword
MeSH Terms
Figure
Reference
-
1. Dortet L, Poirel L, Al Yaqoubi F, Nordmann P. NDM-1, OXA-48 and OXA-181 carbapenemase-producing Enterobacteriaceae in Sultanate of Oman. Clin Microbiol Infect. 2012; 18:E144–E148.2. Aung MS, San N, Maw WW, San T, Urushibara N, Kawaguchiya M, Sumi A, Kobayashi N. Prevalence of extended-spectrum beta-lactamase and carbapenemase genes in clinical isolates of Escherichia coli in Myanmar: Dominance of blaNDM-5 and emergence of blaOXA-181. Microb Drug Resist. 2018; 24:1333–1344.
Article3. Khajuria A, Praharaj AK, Kumar M, Grover N. Emergence of Escherichia coli, co-producing NDM-1 and OXA-48 carbapenemases, in urinary isolates, at a tertiary care centre at Central India. J Clin Diagn Res. 2014; 8:DC01–DC04.4. Cho SY, Huh HJ, Baek JY, Chung NY, Ryu JG, Ki CS, Chung DR, Lee NY, Song JH. Klebsiella pneumoniae co-producing NDM-5 and OXA-181 carbapenemases, South Korea. Emerg Infect Dis. 2015; 21:1088–1089.
Article5. Jhang J, Wang HY, Yoo G, Hwang GY, Uh Y, Yoon KJ. NDM-5 and OXA-48 co-producing uropathogenic Escherichia coli isolate: First case in Korea. Ann Lab Med. 2018; 38:277–279.
Article6. Song W, Yoo G, Hwang GY, Uh Y. Evaluation of diagnostic performance of RAPIDEC CARBA NP test for carbapenemase-producing Enterobacteriaceae . Ann Clin Microbiol. 2016; 19:59–64.
Article7. Kim J, Bae IK, Jeong SH, Chang CL, Lee CH, Lee K. Characterization of IncF plasmids carrying the bla CTX-M-14 gene in clinical isolates of Escherichia coli from Korea. J Antimicrob Chemother. 2011; 66:1263–1268.
Article8. Centers for Disease Control and Prevention (CDC). Laboratory protocol for detection of carbapenem-resistant or carbapenemase-producing, Klebsiella spp. and E. coli from rectal swabs. Accessed 1 July, 2011. Available at: https://pdfs.semanticscholar.org/19e7/0fac8709331116cef737b962b976849ac5ac.pdf.9. Centers for Disease Control and Prevention (CDC). Facility guidance for control of carbapenem-resistant Enterobacteriaceae (CRE)-November 2015 update CRE Toolkit. Accessed 24 August, 2016. Available at: https://www.cdc.gov/hai/pdfs/cre/CRE-guidance-508.pdf.10. French CE, Coope C, Conway L, Higgins JP, McCulloch J, Okoli G, Patel BC, Oliver I. Control of carbapenemase-producing Enterobacteriaceae outbreaks in acute settings: an evidence review. J Hosp Infect. 2017; 95:3–45.
Article11. Wendorf KA, Kay M, Baliga C, Weissman SJ, Gluck M, Verma P, D'Angeli M, Swoveland J, Kang MG, Eckmann K, Ross AS, Duchin J. Endoscopic retrograde cholangiopancreatography-associated AmpC Escherichia coli outbreak. Infect Control Hosp Epidemiol. 2015; 36:634–642.
Article12. Epstein L, Hunter JC, Arwady MA, Tsai V, Stein L, Gribogiannis M, Frias M, Guh AY, Laufer AS, Black S, Pacilli M, Moulton-Meissner H, Rasheed JK, Avillan JJ, Kitchel B, Limbago BM, MacCannell D, Lonsway D, Noble-Wang J, Conway J, Conover C, Vernon M, Kallen AJ. New Delhi metallo-β-lactamase-producing carbapenem-resistant Escherichia coli associated with exposure to duodenoscopes. JAMA. 2014; 312:1447–1455.
Article13. Lai KK, Fontecchio SA, Kelley AL, Melvin ZS, Baker S. The epidemiology of fecal carriage of vancomycin-resistant enterococci. Infect Control Hosp Epidemiol. 1997; 18:762–765.
Article14. Karki S, Land G, Aitchison S, Kennon J, Johnson PD, Ballard SA, Leder K, Cheng AC. Long-term carriage of vancomycin-resistant enterococci in patients discharged from hospitals: a 12-year retrospective cohort study. J Clin Microbiol. 2013; 51:3374–3379.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rapid Identification of OXA-48-like, KPC, NDM, and VIM Carbapenemase-Producing Enterobacteriaceae From Culture: Evaluation of the RESIST-4 O.K.N.V. Multiplex Lateral Flow Assay
- Emergence and Spread of OXA-48-Like Carbapenemase-Producing Enterobacteriaceae
- Disk Carbapenemase Test for the Rapid Detection of KPC-, NDM-, and Other Metallo-β-Lactamase-Producing Gram-Negative Bacilli
- NDM-5 and OXA-48 Co-producing Uropathogenic Escherichia coli Isolate: First Case in Korea
- Evaluation of Six Phenotypic Methods for the Detection of Carbapenemases in Gram-Negative Bacteria With Characterized Resistance Mechanisms