Yonsei Med J.
2019 Jul;60(7):694-699. 10.3349/ymj.2019.60.7.694.
Current Status of Patient Education in the Management of Atopic Dermatitis in Korea
- Affiliations
-
- 1Department of Dermatology, Severance Hospital, Cutaneous Biology Research Institute, Yonsei University College of Medicine, Seoul, Korea. copark@yuhs.ac
- 2Department of Pediatrics, Dankook University Hospital, Cheonan, Korea.
- 3Department of Dermatology, Atopy Clinic, Seoul Medical Center, Seoul, Korea.
- 4Department of Dermatology, School of Medicine, Kyungpook National University, Daegu, Korea.
- 5Department of Internal Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea.
- 6Department of Pediatrics, Atopy Clinic, Seoul Medical Center, Seoul, Korea.
- 7Department of Pediatrics, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea.
- 8Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea.
- 9Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 10Department of Pediatrics, School of Medicine, Kyung Hee University, Seoul, Korea.
- 11Department of Pediatrics, College of Medicine, the Catholic University of Korea, Seoul, Korea.
- 12Department of Dermatology, Soonchunhyang University College of Medicine, Seoul, Korea.
- 13Department of Dermatology, Chung-Ang University Hospital, Seoul, Korea.
- KMID: 2450410
- DOI: http://doi.org/10.3349/ymj.2019.60.7.694
Abstract
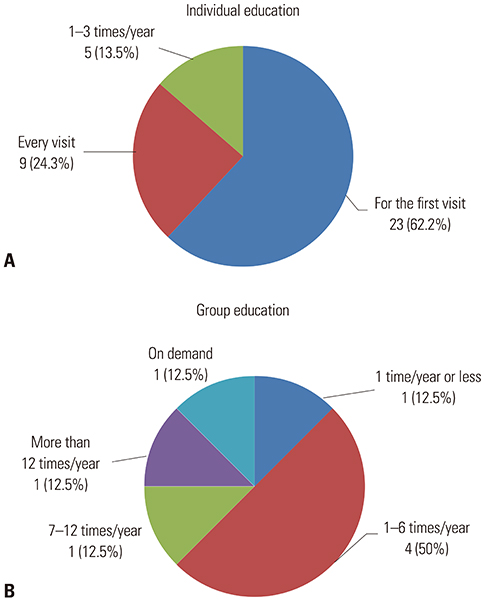
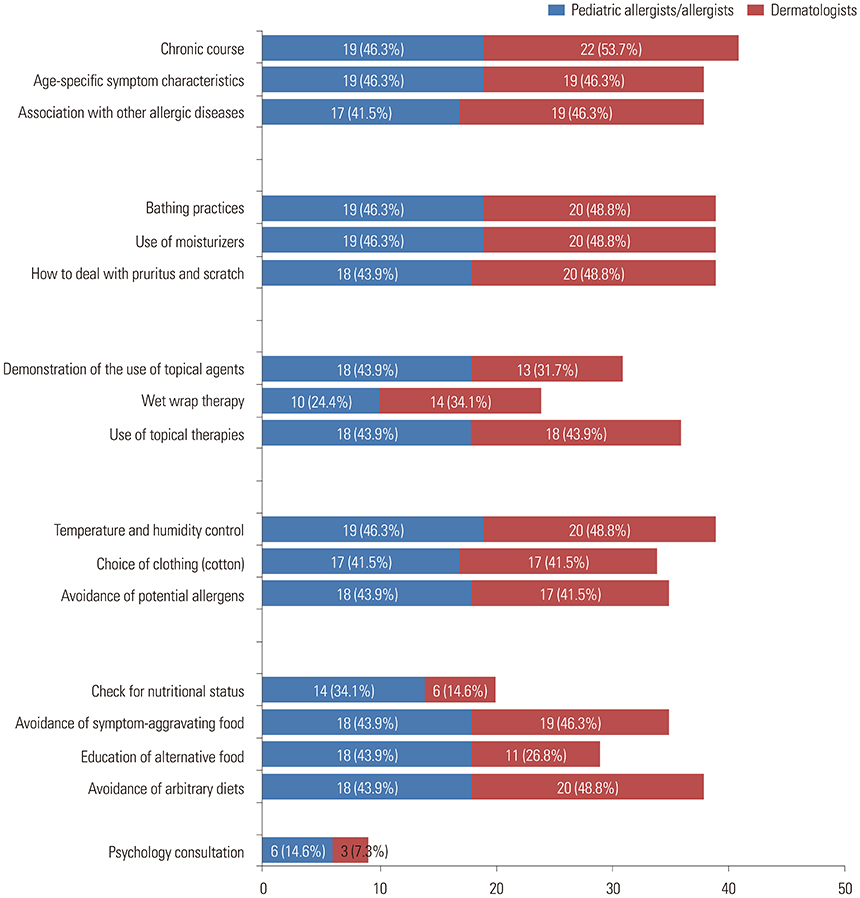
- Patient education is important for successful management of atopic dermatitis; however, due to limited time and resources, patient education remains insufficient. This study aimed to investigate the current state of education provided by Korean dermatologists, pediatric allergists, and allergists to patients with atopic dermatitis. A questionnaire survey consisting of items regarding educational programs for patients with atopic dermatitis was conducted via e-mail. In total, 153 participants responded to the questionnaires, and 26.8% indicated that they have had separate educational programs. The workforce involved in the educational program included nurses, residents or fellows, dieticians, pharmacists, and clinical psychologists. Most education protocols addressed the characteristics and natural course of atopic dermatitis and environmental management. Overall, 96.7% of the participants replied that an additional charge is needed for education; moreover, additional assistance from an academic society or association, in the form of medical staff, organized data, and advertisement, is required to develop and provide a well-structured educational program. A standardized education protocol will effectively provide appropriate education for patients with atopic dermatitis. Arrangement of education fees, covered by the National Health Insurance Service, will lead to the establishment of a structured educational program and participation of an additional medical workforce.
Keyword
MeSH Terms
Figure
Reference
-
1. Spergel JM. Epidemiology of atopic dermatitis and atopic march in children. Immunol Allergy Clin North Am. 2010; 30:269–280.
Article2. Morren MA, Przybilla B, Bamelis M, Heykants B, Reynaers A, Degreef H. Atopic dermatitis: triggering factors. J Am Acad Dermatol. 1994; 31(3 Pt 1):467–473.
Article3. Kim JE, Kim HJ, Lew BL, Lee KH, Hong SP, Jang YH, et al. Consensus guidelines for the treatment of atopic dermatitis in Korea (Part I): general management and topical treatment. Ann Dermatol. 2015; 27:563–577.
Article4. Chin HW, Jang HS, Jang BS, Jo JH, Kim MB, Oh CK, et al. A study on utilization of alternative medicine for patients with atopic dermatitis. Korean J Dermatol. 2005; 43:903–911.5. Kim JK, Kim JH, Lim DH, Son BK. Qualitative assessment of atopic dermatitis-related websites. Pediatr Allergy Respir Dis. 2007; 17:282–288.6. Li AW, Yin ES, Antaya RJ. Topical corticosteroid phobia in atopic dermatitis: a systematic review. JAMA Dermatol. 2017; 153:1036–1042.7. Shin JY, Kim DW, Park CW, Seo SJ, Park YL, Lee JR, et al. An educational program that contributes to improved patient and parental understanding of atopic dermatitis. Ann Dermatol. 2014; 26:66–72.
Article8. Sidbury R, Tom WL, Bergman JN, Cooper KD, Silverman RA, Berger TG, et al. Guidelines of care for the management of atopic dermatitis: section 4. Prevention of disease flares and use of adjunctive therapies and approaches. J Am Acad Dermatol. 2014; 71:1218–1233.9. Pustišek N, Šitum M, Vurnek Živković M, Ljubojević Hadžavdić S, Vurnek M, Niseteo T. The significance of structured parental educational intervention on childhood atopic dermatitis: a randomized controlled trial. J Eur Acad Dermatol Venereol. 2016; 30:806–812.
Article10. Jang YH, Lee JS, Kim SL, Song CH, Jung HD, Shin DH, et al. A family-engaged educational program for atopic dermatitis: a seven-year, multicenter experience in Daegu-Gyeongbuk, South Korea. Ann Dermatol. 2015; 27:383–388.
Article11. Yum HY, Han KO, Park J, Kang MY, Chang SI, Cho SH, et al. Improvement in disease knowledge through an education program of atopic dermatitis. Korean J Asthma Allergy Clin Immunol. 2012; 32:21–25.12. Heratizadeh A, Werfel T, Wollenberg A, Abraham S, Plank-Habibi S, Schnopp C, et al. Effects of structured patient education in adults with atopic dermatitis: multicenter randomized controlled trial. J Allergy Clin Immunol. 2017; 140:845–853.
Article13. Staab D, Diepgen TL, Fartasch M, Kupfer J, Lob-Corzilius T, Ring J, et al. Age related, structured educational programmes for the management of atopic dermatitis in children and adolescents: multicentre, randomised controlled trial. BMJ. 2006; 332:933–938.
Article14. Barbarot S, Gagnayre R, Bernier C, Chavigny JM, Chiaverini C, Lacour JP, et al. [A guide for education programs in atopic dermatitis]. Ann Dermatol Venereol. 2007; 134:121–127.15. Agner T. Compliance among patients with atopic eczema. Acta Derm Venereol Suppl (Stockh). 2005; (215):33–35.16. Niebel G, Kallweit C, Lange I, Fölster-Holst R. [Direct versus video-aided parent education in atopic eczema in childhood as a supplement to specialty physician treatment. A controlled pilot study]. Hautarzt. 2000; 51:401–411.17. Lee JB, Rha YH, Choi SH. A questionnaire survey of care-givers' understanding of atopic dermatitis. Korean J Asthma Allergy Clin Immunol. 2009; 29:179–185.18. Muraro A, Halken S, Arshad SH, Beyer K, Dubois AE, Du Toit G, et al. EAACI food allergy and anaphylaxis guidelines. Primary prevention of food allergy. Allergy. 2014; 69:590–601.
Article19. Nicol NH, Ersser SJ. The role of the nurse educator in managing atopic dermatitis. Immunol Allergy Clin North Am. 2010; 30:369–383.
Article20. Chung SW, Chang EY, Lee HC, Shin MY, Kim BE, Ahn KM, et al. The relationships among severity score, behavioral problem, parental stress, maternal depression, and social support in children with atopic dermatitis. Korean J Asthma Allergy Clin Immunol. 2005; 25:39–44.21. Finlay AY. Measures of the effect of adult severe atopic eczema on quality of life. J Eur Acad Dermatol Venereol. 1996; 7:149–154.
Article22. Senra MS, Wollenberg A. Psychodermatological aspects of atopic dermatitis. Br J Dermatol. 2014; 170:Suppl 1. 38–43.
Article23. Ehlers A, Stangier U, Gieler U. Treatment of atopic dermatitis: a comparison of psychological and dermatological approaches to relapse prevention. J Consult Clin Psychol. 1995; 63:624–635.
Article24. Norén P, Melin L. The effect of combined topical steroids and habit-reversal treatment in patients with atopic dermatitis. Br J Dermatol. 1989; 121:359–366.
Article25. Boguniewicz M, Nicol N, Kelsay K, Leung DY. A multidisciplinary approach to evaluation and treatment of atopic dermatitis. Semin Cutan Med Surg. 2008; 27:115–127.
Article26. de Bes J, Legierse CM, Prinsen CA, de Korte J. Patient education in chronic skin diseases: a systematic review. Acta Derm Venereol. 2011; 91:12–17.
Article27. Ring J, Alomar A, Bieber T, Deleuran M, Fink-Wagner A, Gelmetti C, et al. Guidelines for treatment of atopic eczema (atopic dermatitis) Part II. J Eur Acad Dermatol Venereol. 2012; 26:1176–1193.
Article28. Lim MS, Lee CH, Sim S, Hong SK, Choi HG. Physical activity, sedentary habits, sleep, and obesity are associated with asthma, allergic rhinitis, and atopic dermatitis in Korean Adolescents. Yonsei Med J. 2017; 58:1040–1046.
Article29. Lee J, Lee H, Noh S, Bae BG, Shin JU, Park CO, et al. Retrospective analysis on the effects of house dust mite specific immunotherapy for more than 3 years in atopic dermatitis. Yonsei Med J. 2016; 57:393–398.
Article30. Sy W, Lamb AJ. Atopic dermatitis disease education. Adv Exp Med Biol. 2017; 1027:179–184.
Article31. Stalder JF, Bernier C, Ball A, De Raeve L, Gieler U, Deleuran M, et al. Therapeutic patient education in atopic dermatitis: worldwide experiences. Pediatr Dermatol. 2013; 30:329–334.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status in Management of Children with Atopic Dermatitis and Knowledge and Practice of Preschool Teachers
- Measurement of Atopic Dermatitis Disability
- Current status and characteristics of atopic dermatitis in Korea
- Therapeutic approach to atopic dermatitis in children
- Status of clinical practice on diagnosis and management of atopic dermatitis in Korea: a questionnaire survey of physicians