Efficacy of Percutaneous Epidural Neuroplasty Does Not Correlate with Dural Sac Cross-Sectional Area in Single Level Disc Disease
- Affiliations
-
- 1Department of Neurosurgery, Guro Teun Teun Hospital, Seoul, Korea.
- 2Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea. shindongah@me.com
- 3Spine and Spinal Cord Research Institute, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2450342
- DOI: http://doi.org/10.3349/ymj.2015.56.3.691
Abstract
- PURPOSE
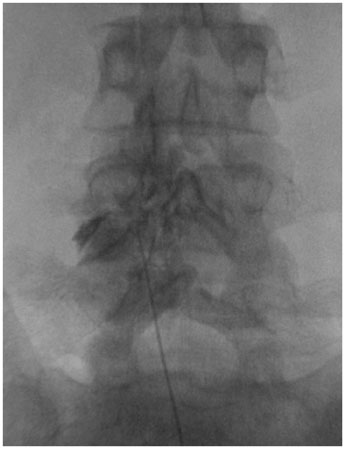
Percutaneous epidural neuroplasty (PEN) is a minimally invasive treatment. The efficacy of PEN has been relatively well investigated; however, the relationship between the clinical effectiveness of PEN and the severity of spinal canal stenosis by disc material has not yet been established. The purpose of this study was to compare clinical outcomes of PEN according to the dural sac cross-sectional area in single level disc disease.
MATERIALS AND METHODS
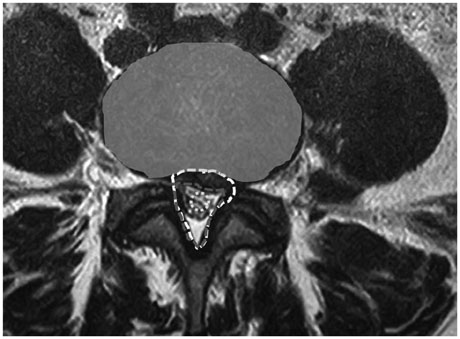
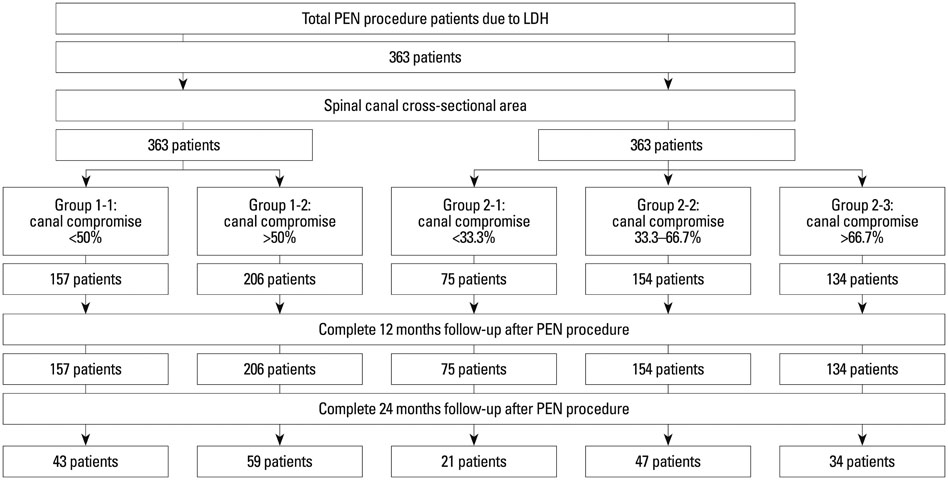
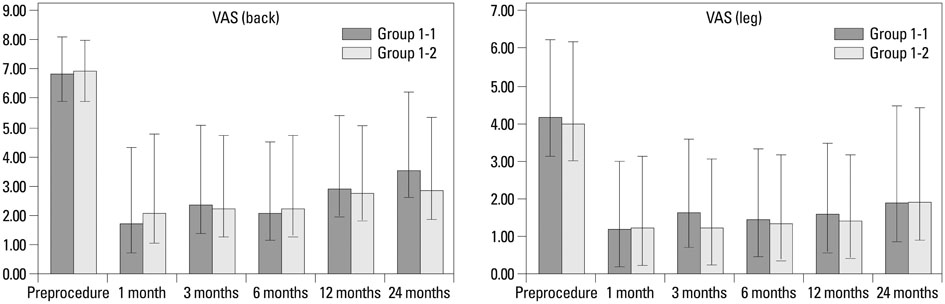
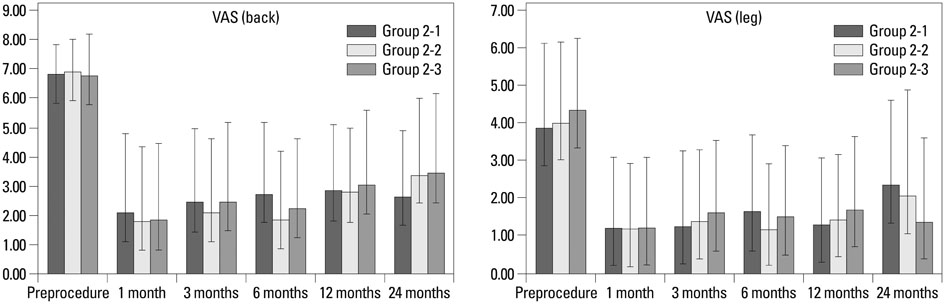
This study included 363 patients with back pain from single level disc disease with and without radiculopathy. Patients were categorized into groups according to spinal canal compromise by disc material: Category 1, less or more than 50%; and Category 2, three subgroups with lesser than a third, between a third and two thirds, and more than two thirds. Clinical outcomes were assessed according to the Visual Analog Scale (VAS) score for back pain and leg pain and Odom's criteria at 1, 3, 6, 12, and 24 months after treatment.
RESULTS
The demographic data showed no difference between groups according to spinal canal compromise by disc material except age (older age correlated with more spinal canal compromise). The dural sac cross-sectional area did not correlate with the VAS scores for back and leg pain after PEN in single level disc disease in Groups 1 and 2. Odom's criteria after PEN were also not different according to dural sac cross-sectional area by disc material.
CONCLUSION
PEN is an effective procedure in treating single level lumbar disc herniation without affecting dural sac cross-sectional area.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
The role of percutaneous neurolysis in lumbar disc herniation: systematic review and meta-analysis
Laxmaiah Manchikanti, Emilija Knezevic, Nebojsa Nick Knezevic, Mahendra R. Sanapati, Alan D. Kaye, Srinivasa Thota, Joshua A. Hirsch
Korean J Pain. 2021;34(3):346-368. doi: 10.3344/kjp.2021.34.3.346.Comments on “The role of percutaneous neurolysis in lumbar disc herniation: systematic review and meta-analysis”
Min Cheol Chang
Korean J Pain. 2022;35(1):124-125. doi: 10.3344/kjp.2022.35.1.124.Clinical Effectiveness of Percutaneous Epidural Neuroplasty According to the Type of Single-Level Lumbar Disc Herniation : A 12-Month Follow-Up Study
Pyung Goo Cho, Gyu Yeul Ji, Young Sul Yoon, Dong Ah Shin
J Korean Neurosurg Soc. 2019;62(6):681-690. doi: 10.3340/jkns.2019.0070.
Reference
-
1. Manchikanti L, Pampati V, Fellows B, Rivera JJ, Damron KS, Beyer C, et al. Effectiveness of percutaneous adhesiolysis with hypertonic saline neurolysis in refractory spinal stenosis. Pain Physician. 2001; 4:366–373.2. Epter RS, Helm S 2nd, Hayek SM, Benyamin RM, Smith HS, Abdi S. Systematic review of percutaneous adhesiolysis and management of chronic low back pain in post lumbar surgery syndrome. Pain Physician. 2009; 12:361–378.3. Viesca CO, Racz GB, Day MR. Special techniques in pain management: lysis of adhesions. Anesthesiol Clin North America. 2003; 21:745–766.
Article4. Veihelmann A, Devens C, Trouillier H, Birkenmaier C, Gerdesmeyer L, Refior HJ. Epidural neuroplasty versus physiotherapy to relieve pain in patients with sciatica: a prospective randomized blinded clinical trial. J Orthop Sci. 2006; 11:365–369.
Article5. Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. A comparative effectiveness evaluation of percutaneous adhesiolysis and epidural steroid injections in managing lumbar post surgery syndrome: a randomized, equivalence controlled trial. Pain Physician. 2009; 12:E355–E368.6. Kim DY, Oh CH, Yoon SH, Park HC, Park CO. Lumbar disc screening using back pain questionnaires: Oswestry Low Back Pain Score, Aberdeen Low Back Pain Scale, and Acute Low Back Pain Screening Questionnaire. Korean J Spine. 2012; 9:153–158.
Article7. Kim TW, Oh CH, Shim YS, Yoon SH, Park HC, Park CO. Psychopathological influence of lumbar disc herniation in male adolescent. Yonsei Med J. 2013; 54:813–818.
Article8. Lee SH, Oh CH, Yoon SH, Park HC, Park CO. Prevalence and geographic distribution of herniated intervertebral disc in Korean 19-year-old male from 2008 to 2009: a study based on Korean conscription-national and geographic prevalence of herniated intervertebral disc in Korean 19YO male-. Yonsei Med J. 2013; 54:1098–1103.
Article9. Ji GY, Oh CH, Lee J, Kim JH, Shin DA. 101 Clinical course after percutaneous epidural neuroplasty according to the type of single level herniated lumbar disc with 12 months follow-up. Neurosurgery. 2013; 60:153.
Article10. Park CH, Lee SH, Jung JY. Dural sac cross-sectional area does not correlate with efficacy of percutaneous adhesiolysis in single level lumbar spinal stenosis. Pain Physician. 2011; 14:377–382.11. Sirvanci M, Bhatia M, Ganiyusufoglu KA, Duran C, Tezer M, Ozturk C, et al. Degenerative lumbar spinal stenosis: correlation with Oswestry Disability Index and MR imaging. Eur Spine J. 2008; 17:679–685.
Article12. Athiviraham A, Yen D, Scott C, Soboleski D. Clinical correlation of radiological spinal stenosis after standardization for vertebral body size. Clin Radiol. 2007; 62:776–780.
Article13. Campbell MJ, Carreon LY, Glassman SD, McGinnis MD, Elmlinger BS. Correlation of spinal canal dimensions to efficacy of epidural steroid injection in spinal stenosis. J Spinal Disord Tech. 2007; 20:168–171.
Article14. Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 2004; 230:583–588.
Article15. Manchikanti L, Cash KA, McManus CD, Pampati V, Singh V, Benyamin R. The preliminary results of a comparative effectiveness evaluation of adhesiolysis and caudal epidural injections in managing chronic low back pain secondary to spinal stenosis: a randomized, equivalence controlled trial. Pain Physician. 2009; 12:E341–E354.16. Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, Abdi S, et al. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009; 12:699–802.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Epidural Neuroplasty
- Functional myelography
- Massive Epidural Hematoma Caused by Percutaneous Epidural Neuroplasty: A Case Report
- Inadvertent Intrathecal Contrast Injection during Percutaneous Epidural Neuroplasty: Two Autopsy Cases
- Acute Motor Weakness of Opposite Lower Extremity after Percutaneous Epidural Neuroplasty