Korean J Pain.
2015 Apr;28(2):144-147. 10.3344/kjp.2015.28.2.144.
Acute Motor Weakness of Opposite Lower Extremity after Percutaneous Epidural Neuroplasty
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kwangju Christian Hospital, Gwangju, Korea.
- 2Department of Anesthesiology and Pain Medicine, Chosun University Hospital, Gwangju, Korea. mdmole@chosun.ac.kr
- 3Department of Anesthesiology and Pain Medicine, Gwangju Saewoori Spine Hospital, Gwangju, Korea.
- KMID: 2278279
- DOI: http://doi.org/10.3344/kjp.2015.28.2.144
Abstract
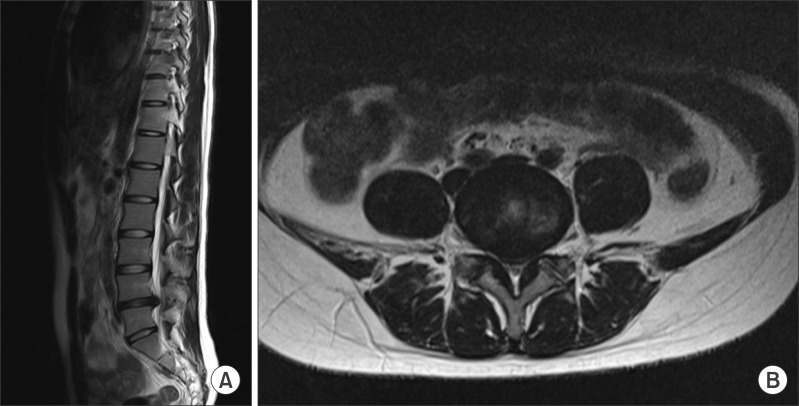
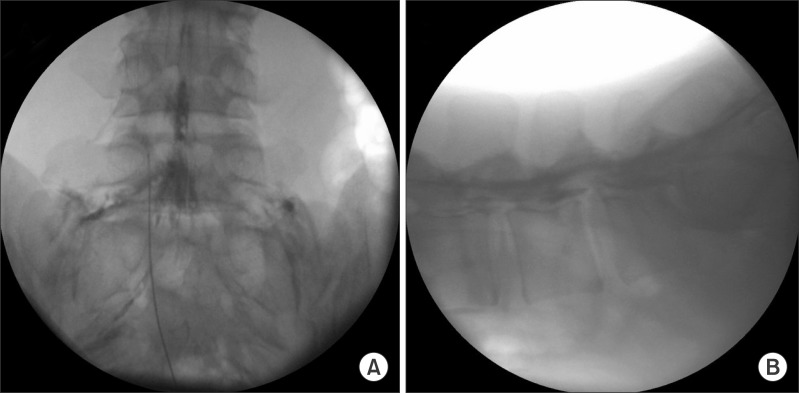
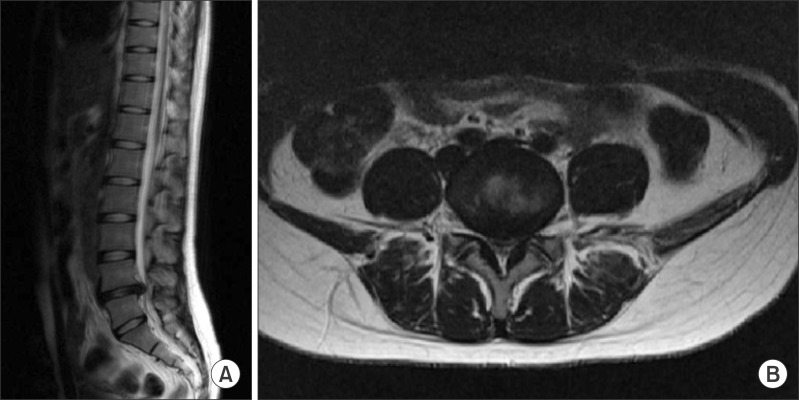
- Recently, percutaneous epidural neuroplasty has become widely used to treat radicular pain caused by spinal stenosis or a herniated intervertebral disc. A 19-year-old female patient suffering from left radicular pain caused by an L4-L5 intervertebral disc herniation underwent percutaneous epidural neuroplasty of the left L5 nerve root using a Racz catheter. After the procedure, the patient complained of acute motor weakness in the right lower leg, on the opposite site to where the neuroplasty was conducted. Emergency surgery was performed, and swelling of the right L5 nerve root was discovered. The patient recovered her motor and sensory functions immediately after the surgery. Theoretically, the injection of a large volume of fluid in a patient with severe spinal stenosis during epidural neuroplasty can increase the pressure on the opposite side of the epidural space, which may cause injury of the opposite nerve by barotrauma from a closed compartment. Practitioners should be aware of this potential complication.
Keyword
MeSH Terms
Figure
Reference
-
1. Racz GB, Holubec JT. Racz GB, editor. Lysis of adhesions in the epidural space. In: Techniques of neurolysis. Boston (MA): Kluwer Academic Publishers;1989. p. 57–72.2. Epter RS, Helm S 2nd, Hayek SM, Benyamin RM, Smith HS, Abdi S. Systematic review of percutaneous adhesiolysis and management of chronic low back pain in post lumbar surgery syndrome. Pain Physician. 2009; 12:361–378. PMID: 19305485.3. Belozer M, Wang G. Epidural adhesiolysis for the treatment of back pain. Health Technol Assess. 2004; 5:1–19.4. Helm Ii S, Benyamin RM, Chopra P, Deer TR, Justiz R. Percutaneous adhesiolysis in the management of chronic low back pain in post lumbar surgery syndrome and spinal stenosis: a systematic review. Pain Physician. 2012; 15:E435–E462. PMID: 22828693.5. Lee F, Jamison DE, Hurley RW, Cohen SP. Epidural lysis of adhesions. Korean J Pain. 2014; 27:3–15. PMID: 24478895.
Article6. Manchikanti L, Malla Y, Wargo BW, Cash KA, Pampati V, Fellows B. A prospective evaluation of complications of 10,000 fluoroscopically directed epidural injections. Pain Physician. 2012; 15:131–140. PMID: 22430650.7. Ho KY, Manghnani P. Acute monoplegia after lysis of epidural adhesions: a case report. Pain Pract. 2008; 8:404–407. PMID: 18721177.
Article8. Bromage PR. Subarachnoid catheters and the cauda equina syndrome: hypotheses in need of trial. Anesthesiology. 1994; 80:711–712. PMID: 8141477.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebellar Infarction Following Epidural Abscess after Epidural Neuroplasty
- Unintended Complication of Intracranial Subdural Hematoma after Percutaneous Epidural Neuroplasty
- Percutaneous Epidural Neuroplasty
- Motor Weakness on Lower Extremities after the Combined Spinal-epidural Anesthesia and Analgesia: A case report
- Massive Epidural Hematoma Caused by Percutaneous Epidural Neuroplasty: A Case Report