Ann Hepatobiliary Pancreat Surg.
2019 May;23(2):128-132. 10.14701/ahbps.2019.23.2.128.
Assessment of patient safety and the efficiency of facility utilization following simplified ultra-rapid intravenous infusion of hepatitis B immunoglobulin in a high-volume liver transplantation center
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- 2Organ Transplantation Center, Asan Medical Center, Seoul, Korea.
- KMID: 2448765
- DOI: http://doi.org/10.14701/ahbps.2019.23.2.128
Abstract
- BACKGROUNDS/AIMS
This study intended to evaluate patient safety and efficiency of facility utilization following simplified ultra-rapid intravenous infusion of hepatitis B immunoglobulin (HBIG) in recipients of hepatitis B virus-associated adult liver transplantation (LT), who visited our outpatient clinic.
METHODS
Our simplified ultra-rapid infusion protocol was to directly infuse 50 ml volume of 10,000 IU HBIG for 20-25 minutes on an ambulatory basis. The incidence of adverse side-effects and the efficiency of facility utilization were assessed retrospectively.
RESULTS
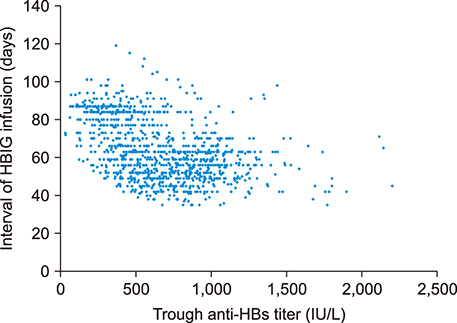
A total of 1,513 patients received 12,472 sessions of HBIG infusion according to simplified ultra-rapid infusion method. Of these, 1,172 patients were converted from conventional ultra-rapid infusion method, and received 8,352 sessions of HBIG infusion for 18 months (mean 7.1 times; 4.8 times per year). The remaining 341 de novo patients received 4,120 sessions of HBIG infusion for 18 months (mean 12.1 times; 8.1 times per year). None of these patients experienced any adverse side-effects following the simplified ultra-rapid infusion. The maximal capacity of HBIG infusion sessions at the injection facility of our outpatient clinic was increased from 65-70 sessions to 80 sessions, after introduction of simplified ultra-rapid infusion method. Mean trough anti-HBs titer was lower, and mean interval of HBIG infusion was longer in the combination therapy group compared with HBIG monotherapy group.
CONCLUSIONS
Our high-volume study indicates that in nearly all LT recipients, rapid infusion of highly purified HBIG within 30 minutes was well-tolerated. This suggests that it would be reasonable to perform simplified ultra-rapid infusion protocol widely for patient convenience.
MeSH Terms
Figure
Reference
-
1. Hwang S, Lee SG, Ahn CS, Kim KH, Moon DB, Ha TY, et al. Prevention of hepatitis B recurrence after living donor liver transplantation: primary high-dose hepatitis B immunoglobulin monotherapy and rescue antiviral therapy. Liver Transpl. 2008; 14:770–778.
Article2. Mohanty SR, Cotler SJ. Management of hepatitis B in liver transplant patients. J Clin Gastroenterol. 2005; 39:58–63.3. Terrault N, Roche B, Samuel D. Management of the hepatitis B virus in the liver transplantation setting: a European and an American perspective. Liver Transpl. 2005; 11:716–732.
Article4. Roche B, Samuel D. Evolving strategies to prevent HBV recurrence. Liver Transpl. 2004; 10:10 Suppl 2. S74–S85.
Article5. Ghany MG, Ayola B, Villamil FG, Gish RG, Rojter S, Vierling JM, et al. Hepatitis B virus S mutants in liver transplant recipients who were reinfected despite hepatitis B immune globulin prophylaxis. Hepatology. 1998; 27:213–222.
Article6. Hwang S, Yu YD, Park GC, Choi YI, Park PJ, Jung SW, et al. Safety of ultra-rapid intravenous infusion of hepatitis B immunoglobulin in liver transplant recipients. Transplant Proc. 2011; 43:1780–1782.
Article7. Choi HJ, Kim DG, Kim SI, Wang HJ, Joh JW, Suh KS, et al. A multicenter phase III study to evaluate the efficacy and safety of hepabulin, a new hepatitis B immunoglobulin, in liver transplantation recipients with hepatitis B. Ann Transplant. 2017; 22:740–748.
Article8. Korean Association for the Study of the Liver. KASL clinical practice guidelines: management of chronic hepatitis B. Clin Mol Hepatol. 2016; 22:18–75.9. Roche B, Roque-Afonso AM, Nevens F, Samuel D. Rational basis for optimizing short and long-term hepatitis B virus prophylaxis post liver transplantation: role of hepatitis B immune globulin. Transplantation. 2015; 99:1321–1334.10. Gane EJ, Angus PW, Strasser S, Crawford DH, Ring J, Jeffrey GP, et al. Lamivudine plus low-dose hepatitis B immunoglobulin to prevent recurrent hepatitis B following liver transplantation. Gastroenterology. 2007; 132:931–937.
Article11. Jiang L, Yan L, Li B, Wen T, Zhao J, Jiang L, et al. Prophylaxis against hepatitis B recurrence posttransplantation using lamivudine and individualized low-dose hepatitis B immunoglobulin. Am J Transplant. 2010; 10:1861–1869.
Article12. Akyildiz M, Karasu Z, Zeytunlu M, Aydin U, Ozacar T, Kilic M. Adefovir dipivoxil therapy in liver transplant recipients for recurrence of hepatitis B virus infection despite lamivudine plus hepatitis B immunoglobulin prophylaxis. J Gastroenterol Hepatol. 2007; 22:2130–2134.
Article13. Wang P, Tam N, Wang H, Zheng H, Chen P, Wu L, et al. Is hepatitis B immunoglobulin necessary in prophylaxis of hepatitis B recurrence after liver transplantation? A meta-analysis. PLoS One. 2014; 9:e104480.
Article14. Moon DB, Lee SG, Hwang S, Kim KH, Ahn CS, Ha TY, et al. Toward more than 400 liver transplantations a year at a single center. Transplant Proc. 2013; 45:1937–1941.
Article15. Hwang S, Ahn CS, Kim KH, Moon DB, Ha TY, Song GW, et al. A cross-sectional analysis of long-term immunosuppressive regimens after liver transplantation at Asan Medical Center: increased preference for mycophenolate mofetil. Ann Hepatobiliary Pancreat Surg. 2018; 22:19–26.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acute Hepatitis Associated with Intravenous Infusion Amiodarone in Patient with Atrial Fibrillation
- Understanding Acute Liver Failure: A Basic Overview of Definition and Treatment
- Overcoming high pre-transplant isoagglutinin titers using high-dose intravenous immunoglobulin, salvage plasmapheresis, and booster rituximab without splenectomy in ABO-incompatible living donor liver transplantation: a case report
- ABO-incompatible living donor liver transplantation with a simplified desensitization and immunosuppression protocol: a single center retrospective study
- Prophylaxis for Hepatitis B Core Antibody-Positive Donors after Liver Transplantation