J Korean Ophthalmol Soc.
2019 Apr;60(4):374-379. 10.3341/jkos.2019.60.4.374.
A Case of Corneal Chemical Injury by High-dose Ethanol during Orbital Wall Fracture Repair
- Affiliations
-
- 1Department of Ophthalmology, Jeju National University School of Medicine, Jeju, Korea. dr.jinho.jeong@gmail.com
- KMID: 2443155
- DOI: http://doi.org/10.3341/jkos.2019.60.4.374
Abstract
- PURPOSE
To report a case of chemical injury of the cornea caused by high-dose ethanol during orbital wall fracture repair.
CASE SUMMARY
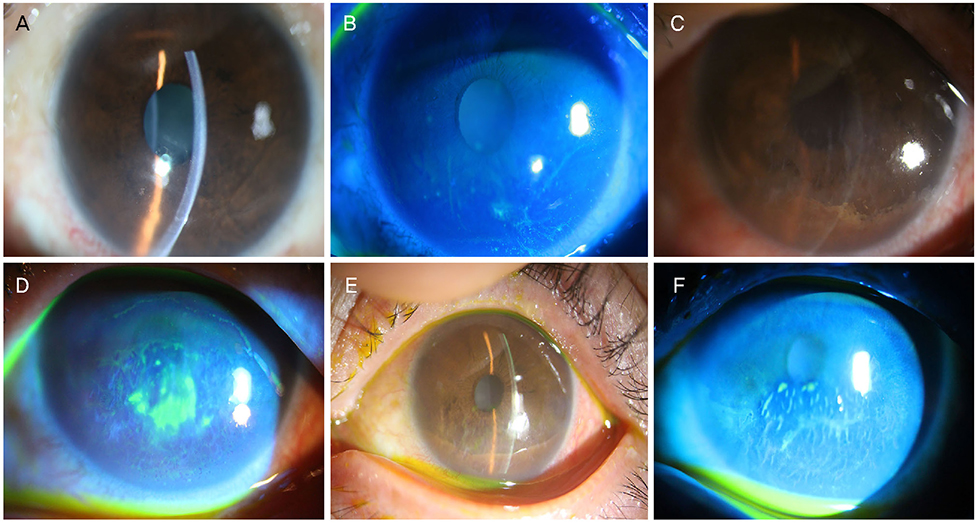
A 56-year-old male presented with pain after blowout fracture repair surgery. During the surgery, 2% hexethanol solution (2% chlorhexidine and 72% ethanol mixture), which was used for disinfection of the face, flowed into the left eye. Conjunctival injection in the left limbus, a large corneal epithelial defect, and severe stromal edema were subsequently observed. The patient was treated with topical antibiotics, steroids, and autologous serum eye drops. After 1 week, the corneal epithelial defect was improved, but at the second month of therapy, recurrent corneal erosion with deterioration of the endothelial cell function occurred. Anterior stromal puncture and laser keratectomy were performed. The corneal epithelial defect and erosion improved, but the endothelial cell density was severely decreased.
CONCLUSIONS
The 2% hexethanol solution is usually used for preoperative skin disinfection, but it contains a high concentration of ethanol. The surgeon should be aware that high concentrations of ethanol may result in severe corneal damage, including corneal endothelial dysfunction and limbal cell deficiency.
MeSH Terms
Figure
Reference
-
1. Roth S, Thisted RA, Erickson JP, et al. Eye injuries after nonocular surgery. a study of 60,965 anesthetics from 1988 to 1992. Anesthesiology. 1996; 85:1020–1027.2. Yu HD, Chou AH, Yang MW, Chang CJ. An analysis of perioperative eye injuries after nonocular surgery. Acta Anaesthesiol Taiwan. 2010; 48:122–129.
Article3. Liu HY, Yeh PT, Kuo KT, et al. Toxic keratopathy following the use of alcohol-containing antiseptics in nonocular surgery. JAMA Ophthalmol. 2016; 134:449–452.
Article4. Mac Rae SM, Brown B, Edelhauser HF. The corneal toxicity of presurgical skin antiseptics. Am J Ophthalmol. 1984; 97:221–232.
Article5. Oh JY, Yu JM, KO JH. Analysis of ethanol effects on corneal epithelium. Invest Ophthalmol Vis Sci. 2013; 54:3852–3856.
Article6. Chang SW, Chou SF, Wang YH. Ethanol treatment induces significant cell death in porcine corneal fibroblasts. Cornea. 2006; 25:1072–1079.
Article7. Eslani M, Baradaran-Rafii A, Movahedan A, Djalilian AR. The ocular surface chemical burns. J Ophthalmol. 2014; 2014:196827.
Article8. Baradaran-Rafii A, Eslani M, Haq Z, et al. Current and upcoming therapies for ocular surface chemical injuries. Ocul Surf. 2017; 15:48–64.
Article9. Perkins TW, Kumar A, Kiland JA. Corneal decompensation following bleb revision with absolute alcohol: clinical pathological correlation. Arch Ophthalmol. 2006; 124:738–741.
Article10. Fish R, Davidson RS. Management of ocular thermal and chemical injuries, including amniotic membrane therapy. Curr Opin Ophthalmol. 2010; 21:317–321.
Article11. Avni Zauberman N, Artornsombudh P, Elbaz U, et al. Anterior stromal puncture for the treatment of recurrent corneal erosion syndrome: patient clinical features and outcomes. Am J Ophthalmol. 2014; 157:273–279.e1.
Article12. Ko BY, Lee GW. Clinical results of phototherapeutic keratectomy for refractory recurrent corneal erosion. J Korean Ophthalmol Soc. 2011; 52:392–400.
Article13. Joyce NC. Proliferative capacity of the corneal endothelium. Prog Retin Eye Res. 2003; 22:359–389.
Article14. Tamori Y, Deng WM. Compensatory cellular hypertrophy: the other strategy for tissue homeostasis. Trends Cell Biol. 2014; 24:230–237.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Repair of Orbital Wall Fracture Using Transcaruncular Approach
- Retrobulbar hematoma following the repair of an orbital wall fracture: a case series
- Transcaruncular Approach to Blowout Fractures of the Medial Orbital Wall
- Repair of Medial Orbital Wall Fracture
- Two Cases of Mucocele After Orbital Fracture Repair