Clin Exp Otorhinolaryngol.
2019 Feb;12(1):72-78. 10.21053/ceo.2018.00388.
Prediction of Obstructive Sleep Apnea Based on Respiratory Sounds Recorded Between Sleep Onset and Sleep Offset
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. iamsungu@gmail.com
- 2Music and Audio Research Group, Graduate School of Convergence Science and Technology, Seoul National University, Seoul, Korea. kglee@snu.ac.kr
- KMID: 2437494
- DOI: http://doi.org/10.21053/ceo.2018.00388
Abstract
OBJECTIVES
To develop a simple algorithm for prescreening of obstructive sleep apnea (OSA) on the basis of respiratorysounds recorded during polysomnography during all sleep stages between sleep onset and offset.
METHODS
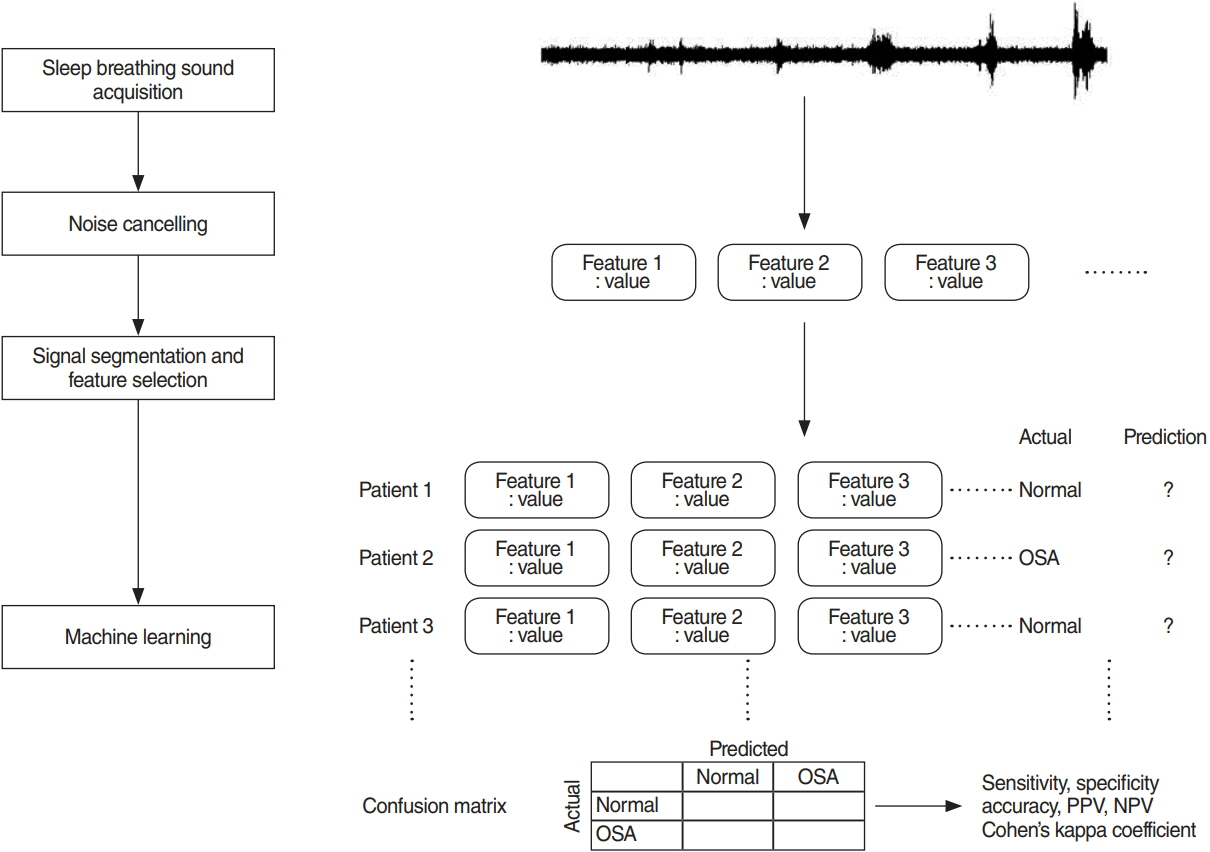
Patients who underwent attended, in-laboratory, full-night polysomnography were included. For all patients, audiorecordings were performed with an air-conduction microphone during polysomnography. Analyses included allsleep stages (i.e., N1, N2, N3, rapid eye movement, and waking). After noise reduction preprocessing, data were segmentedinto 5-s windows and sound features were extracted. Prediction models were established and validated with10-fold cross-validation by using simple logistic regression. Binary classifications were separately conducted for threedifferent threshold criteria at apnea hypopnea index (AHI) of 5, 15, or 30. Prediction model characteristics, includingaccuracy, sensitivity, specificity, positive predictive value (precision), negative predictive value, and area under thecurve (AUC) of the receiver operating characteristic were computed.
RESULTS
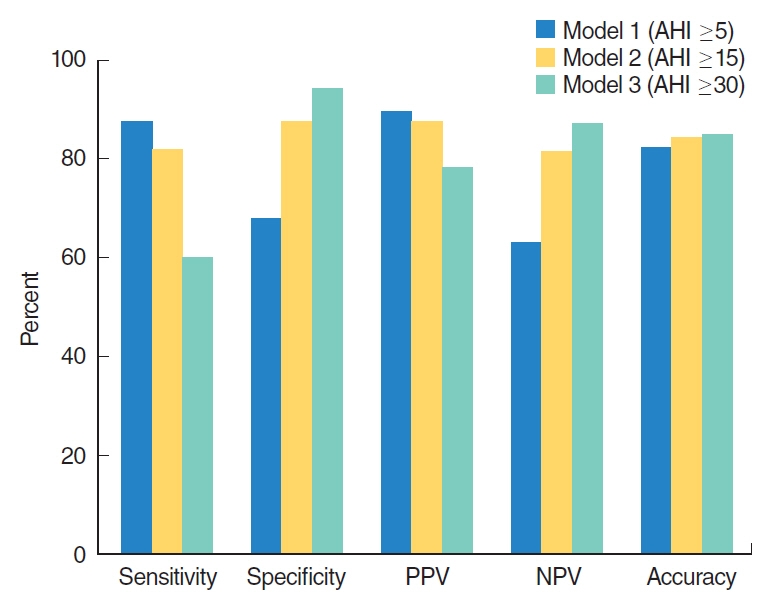
A total of 116 subjects were included; their mean age, body mass index, and AHI were 50.4 years, 25.5 kg/m2, and23.0/hr, respectively. A total of 508 sound features were extracted from respiratory sounds recorded throughoutsleep. Accuracies of binary classifiers at AHIs of 5, 15, and 30 were 82.7%, 84.4%, and 85.3%, respectively. Predictionperformances for the classifiers at AHIs of 5, 15, and 30 were AUC, 0.83, 0.901, and 0.91; sensitivity, 87.5%,81.6%, and 60%; and specificity, 67.8%, 87.5%, and 94.1%. Respective precision values of the classifiers were89.5%, 87.5%, and 78.2% for AHIs of 5, 15, and 30.
CONCLUSION
This study showed that our binary classifier predicted patients with AHI of ≥15 with sensitivity and specificityof >80% by using respiratory sounds during sleep. Since our prediction model included all sleep stage data, algorithmsbased on respiratory sounds may have a high value for prescreening OSA with mobile devices.
MeSH Terms
Figure
Reference
-
1. Xie C, Zhu R, Tian Y, Wang K. Association of obstructive sleep apnoea with the risk of vascular outcomes and all-cause mortality: a meta-analysis. BMJ Open. 2017; Dec. 7(12):e013983.
Article2. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013; May. 177(9):1006–14.
Article3. Ahmed M, Patel NP, Rosen I. Portable monitors in the diagnosis of obstructive sleep apnea. Chest. 2007; Nov. 132(5):1672–7.
Article4. Ong AA, Gillespie MB. Overview of smartphone applications for sleep analysis. World J Otorhinolaryngol Head Neck Surg. 2016; Mar. 2(1):45–9.
Article5. Camacho M, Robertson M, Abdullatif J, Certal V, Kram YA, Ruoff CM, et al. Smartphone apps for snoring. J Laryngol Otol. 2015; Oct. 129(10):974–9.
Article6. Jung HJ, Wee JH, Rhee CS, Kim JW. Full-night measurement of level of obstruction in sleep apnea utilizing continuous manometry. Laryngoscope. 2017; Dec. 127(12):2897–902.
Article7. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999; Aug. 22(5):667–89.8. Kim J, Kim T, Lee D, Kim JW, Lee K. Exploiting temporal and non-stationary features in breathing sound analysis for multiple obstructive sleep apnea severity classification. Biomed Eng Online. 2017; Jan. 16(1):6.
Article9. Frank E, Hall MA, Witten IH. The Weka Workbench. Online appendix for “data mining: practical machine learning tools and techniques". 4th ed. Burlington (NJ): Morgan Kaufmann;2016.10. Emoto T, Kashihara M, Abeyratne UR, Kawata I, Jinnouchi O, Aku-tagawa M, et al. Signal shape feature for automatic snore and breathing sounds classification. Physiol Meas. 2014; Dec. 35(12):2489–99.
Article11. Sun X, Kim JY, Won Y, Kim JJ, Kim KA. Efficient snoring and breathing detection based on sub-band spectral statistics. Biomed Mater Eng. 2015; 26 Suppl 1:S787–93.
Article12. Nguyen TL, Won Y. Sleep snoring detection using multi-layer neural networks. Biomed Mater Eng. 2015; 26 Suppl 1:S1749–55.
Article13. Janott C, Schuller B, Heiser C. Acoustic information in snoring noises. HNO. 2017; Feb. 65(2):107–16.14. Samuelsson LB, Rangarajan AA, Shimada K, Krafty RT, Buysse DJ, Strollo PJ, et al. Support vector machines for automated snoring detection: proof-of-concept. Sleep Breath. 2017; Mar. 21(1):119–33.
Article15. Koo SK, Kwon SB, Kim YJ, Moon JI, Kim YJ, Jung SH. Acoustic analysis of snoring sounds recorded with a smartphone according to obstruction site in OSAS patients. Eur Arch Otorhinolaryngol. 2017; Mar. 274(3):1735–40.
Article16. Qian K, Janott C, Pandit V, Zhang Z, Heiser C, Hohenhorst W, et al. Classification of the excitation location of snore sounds in the upper airway by acoustic multifeature analysis. IEEE Trans Biomed Eng. 2017; Aug. 64(8):1731–41.
Article17. Janott C, Schmitt M, Zhang Y, Qian K, Pandit V, Zhang Z, et al. Snoring classified: The Munich-Passau Snore Sound Corpus. Comput Biol Med. 2018; Mar. 94:106–18.
Article18. Shokrollahi M, Saha S, Hadi P, Rudzicz F, Yadollahi A. Snoring sound classification from respiratory signal. Conf Proc IEEE Eng Med Biol Soc. 2016; Aug. 2016:3215–8.
Article19. Elwali A, Moussavi Z. Obstructive sleep apnea screening and airway structure characterization during wakefulness using tracheal breathing sounds. Ann Biomed Eng. 2017; Mar. 45(3):839–50.
Article20. Halevi M, Dafna E, Tarasiuk A, Zigel Y. Can we discriminate between apnea and hypopnea using audio signals? Conf Proc IEEE Eng Med Biol Soc. 2016; Aug. 2016:3211–4.
Article21. Kim T, Kim JW, Lee K. Detection of sleep disordered breathing severity using acoustic biomarker and machine learning techniques. Biomed Eng Online. 2018; Feb. 17(1):16.
Article22. Erdenebayar U, Park JU, Jeong P, Lee KJ. Obstructive sleep apnea screening using a piezo-electric sensor. J Korean Med Sci. 2017; Jun. 32(6):893–9.
Article23. Saeb S, Cybulski TR, Schueller SM, Kording KP, Mohr DC. Scalable passive sleep monitoring using mobile phones: opportunities and obstacles. J Med Internet Res. 2017; Apr. 19(4):e118.
Article24. White LH, Lyons OD, Yadollahi A, Ryan CM, Bradley TD. Night-to-night variability in obstructive sleep apnea severity: relationship to overnight rostral fluid shift. J Clin Sleep Med. 2015; Jan. 11(2):149–56.
Article25. Deacon NL, Jen R, Li Y, Malhotra A. Treatment of obstructive sleep apnea: prospects for personalized combined modality therapy. Ann Am Thorac Soc. 2016; Jan. 13(1):101–8.
Article