Anesth Pain Med.
2018 Jan;13(1):53-60. 10.17085/apm.2018.13.1.53.
Combination of nefopam and remifentanil is more effective to reduce rocuronium-induced withdrawal response compared with remifentanil alone: a prospective, double-blinded, randomized control study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chosun University Hospital, Korea. ksh3223@chosun.ac.kr
- 2Department of Anesthesiology and Pain Medicine, School of Medicine, Chosun University, Gwangju, Korea.
- KMID: 2436056
- DOI: http://doi.org/10.17085/apm.2018.13.1.53
Abstract
- BACKGROUND
We investigated the effect of combination of nefopam and remifentanil under the hypothesis that nefopam would effectively prevent rocuronium-induced withdrawal response by blocking serotonin receptors and providing a synergistic or additional effect with remifentanil.
METHODS
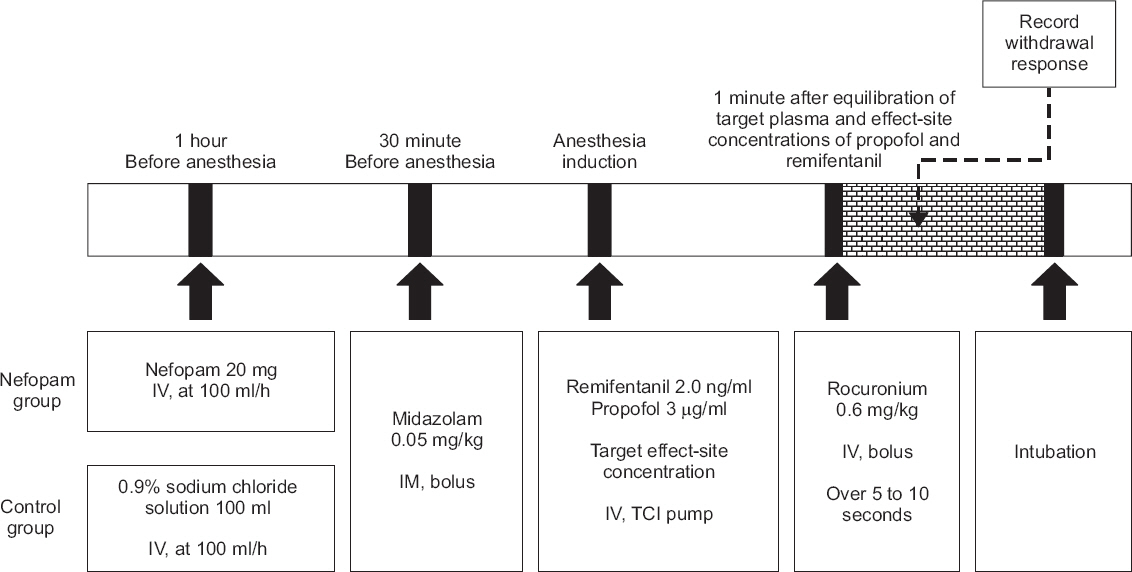
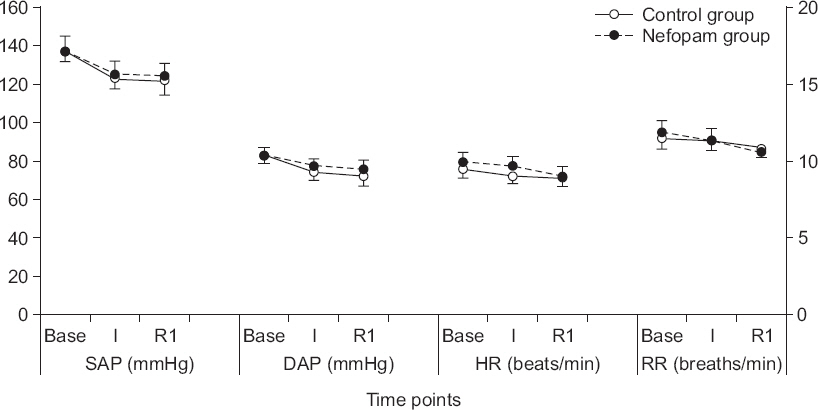
After receiving Institutional Review Board approval, 76 patients aged between 20 and 65 years with American Society of Anesthesiologists physical statuses of I or II were randomly allocated to the control group and nefopam group. In the control group, 102 ml of 0.9% sodium chloride solution was infused one hour before surgery at 100 ml/h. In the nefopam group, 20 mg nefopam (2 ml) in 100 ml of a 0.9% sodium chloride solution was infused one hour before surgery at 100 ml/h. Rocuronium (0.6 mg/kg) was injected after the induction of anesthesia with remifentanil and propofol at target concentrations of 2.0 ng/ml and 3.0 mg/ml, respectively. The grades of rocuronium-induced withdrawal response were evaluated using a four-point scale. The hemodynamics and respiratory rates were recorded upon operating room arrival, after anesthesia induction, and one minute post-injection of rocuronium.
RESULTS
Two patients (nefopam group) were excluded due to incomplete infusion and side effects; thus, 74 patients were finally analyzed. The overall incidence of rocuronium-induced withdrawal response was significantly lower in nefopam group (27.8%, n = 36) than in control group (60.5%, n = 38) (P = 0.005).
CONCLUSIONS
The combination of nefopam (20 mg) and remifentanil is more effective at reducing rocuronium-induced withdrawal response than remifentanil infusion alone with stable hemodynamics.
Keyword
MeSH Terms
Figure
Reference
-
1. Prabhakar H, Singh GP, Ali Z, Kalaivani M, Smith MA. Pharmacological and non-pharmacological interventions for reducing rocuronium bromide induced pain on injection in children and adults. Cochrane Database Syst Rev. 2016; 2:CD009346. DOI: 10.1002/14651858.CD009346.pub2.2. Choi GJ, Lee S, Lee JH, Park SG, Kang H. Pharmacological and non-pharmacological intervention for rocuronium-induced withdrawal movement in the Korean population: a meta-analysis of 41 studies including 4,742 subjects. Korean J Anesthesiol. 2014; 66:419–32. DOI: 10.4097/kjae.2014.66.6.419. PMID: 25006365. PMCID: PMC4085262.3. Kwak HJ, Kim JY, Kim YB, Min SK, Moon BK, Kim JY. Pharmacological prevention of rocuronium-induced injection pain or withdrawal movements: a meta-analysis. J Anesth. 2013; 27:742–9. DOI: 10.1007/s00540-013-1595-7. PMID: 23519582.4. Uzun S, Erden IA, Canbay O, Aypar U. The effect of intravenous paracetamol for the prevention of rocuronium injection pain. Kaohsiung J Med Sci. 2014; 30:566–9. DOI: 10.1016/j.kjms.2014.08.002. PMID: 25458046.5. Cho K, Lee SH, Lee W, Chu BK, Kim MH, Lim SH, et al. Effect of pretreatment with palonosetron on withdrawal movement associated with rocuronium injection. Korean J Anesthesiol. 2014; 66:23–7. DOI: 10.4097/kjae.2014.66.1.23. PMID: 24567809. PMCID: PMC3926996.6. Memiş D, Turan A, Karamanlioğlu B, Süt N, Pamukçu Z. The prevention of pain from injection of rocuronium by ondansetron, lidocaine, tramadol, and fentanyl. Anesth Analg. 2002; 94:1517–20. DOI: 10.1213/00000539-200206000-00026. PMID: 12032018.7. Reddy MS, Chen FG, Ng HP. Effect of ondansetron pretreatment on pain after rocuronium and propofol injection: a randomised, double-blind controlled comparison with lidocaine. Anaesthesia. 2001; 56:902–5. DOI: 10.1046/j.1365-2044.2001.02059-6.x. PMID: 11531681.8. Park KB, Jeon Y, Yi J, Kim JH, Chung SY, Kwak KH. [The effect of palonosetron on rocuronium-induced withdrawal movement]. Rev Bras Anestesiol. 2017; 67:337–41. Portuguese. DOI: 10.1016/j.bjan.2016.04.010. PMID: 28040235.9. Jung KT, Kim HJ, Bae HS, Lee HY, Kim SH, So KY, et al. Effects of lidocaine, ketamine, and remifentanil on withdrawal response of rocuronium. Korean J Anesthesiol. 2014; 67:175–80. DOI: 10.4097/kjae.2014.67.3.175. PMID: 25302093. PMCID: PMC4188762.10. Zhang Y, Xiang Y, Liu J. Prevention of pain on injection of rocuronium: a comparison of lidocaine with different doses of parecoxib. J Clin Anesth. 2012; 24:456–9. DOI: 10.1016/j.jclinane.2011.12.006. PMID: 22762978.11. Kim KH, Abdi S. Rediscovery of nefopam for the treatment of neuropathic pain. Korean J Pain. 2014; 27:103–11. DOI: 10.3344/kjp.2014.27.2.103. PMID: 24748937. PMCID: PMC3990817.12. Chanques G, Sebbane M, Constantin JM, Ramillon N, Jung B, Cissé M, et al. Analgesic efficacy and haemodynamic effects of nefopam in critically ill patients. Br J Anaesth. 2011; 106:336–43. DOI: 10.1093/bja/aeq375. PMID: 21205626.13. Park SJ, Park HJ, Choi JY, Kang HS, Choi HS. The influence of age and gender on remifentanil EC(50) for preventing rocuronium induced withdrawal movements. Korean J Anesthesiol. 2010; 58:244–8. DOI: 10.4097/kjae.2010.58.3.244. PMID: 20498772. PMCID: PMC2872841.14. Na YC, Lee HG, Lee SH, Jang EA, Yoon MH. The efficacy of sevolflurane inhalation alone or its combination with intravenous remifentanil against withdrawal movements on rocuronium injection in children. Korean J Anesthesiol. 2014; 67:373–7. DOI: 10.4097/kjae.2014.67.6.373. PMID: 25558336. PMCID: PMC4280473.15. Choi BI, Choi SH, Shin YS, Lee SJ, Yoon KB, Shin SK, et al. Remifentanil prevents withdrawal movements caused by intravenous injection of rocuronium. Yonsei Med J. 2008; 49:211–6. DOI: 10.3349/ymj.2008.49.2.211. PMID: 18452256. PMCID: PMC2615319.16. Kim JH, Kim JH, Han SH, Hwang JW, Oh AY. Alfentanil is comparable to remifentanil in preventing withdrawal movement following rocuronium injection. J Clin Anesth. 2009; 21:9–12. DOI: 10.1016/j.jclinane.2008.06.016. PMID: 19232934.17. Yoon JY, Kim HK, Kwon JY, Shin SW, Kim KH, Kim WS, et al. EC(50) of remifentanil to prevent withdrawal movement associated with injection of rocuronium. J Anesth. 2010; 24:182–6. DOI: 10.1007/s00540-010-0868-7. PMID: 20127371.18. Girard P, Coppé MC, Verniers D, Pansart Y, Gillardin JM. Role of catecholamines and serotonin receptor subtypes in nefopam-induced antinociception. Pharmacol Res. 2006; 54:195–202. DOI: 10.1016/j.phrs.2006.04.008. PMID: 16750379.19. Rosland JH, Hole K. The effect of nefopam and its enantiomers on the uptake of 5-hydroxytryptamine, noradrenaline and dopamine in crude rat brain synaptosomal preparations. J Pharm Pharmacol. 1990; 42:437–8. DOI: 10.1111/j.2042-7158.1990.tb06587.x.20. Mimoz O, Incagnoli P, Josse C, Gillon MC, Kuhlman L, Mirand A, et al. Analgesic efficacy and safety of nefopam vs. propacetamol following hepatic resection. Anaesthesia. 2001; 56:520–5. DOI: 10.1046/j.1365-2044.2001.01980.x. PMID: 11412156.21. Kapfer B, Alfonsi P, Guignard B, Sessler DI, Chauvin M. Nefopam and ketamine comparably enhance postoperative analgesia. Anesth Analg. 2005; 100:169–74. DOI: 10.1213/01.ANE.0000138037.19757.ED. PMID: 15616073. PMCID: PMC1283103.22. Tirault M, Derrode N, Clevenot D, Rolland D, Fletcher D, Debaene B. The effect of nefopam on morphine overconsumption induced by large-dose remifentanil during propofol anesthesia for major abdominal surgery. Anesth Analg. 2006; 102:110–7. DOI: 10.1213/01.ANE.0000181103.07170.15. PMID: 16368814.23. Yoo JY, Lim BG, Kim H, Kong MH, Lee IO, Kim NS. The analgesic effect of nefopam combined with low dose remifentanil in patients undergoing middle ear surgery under desflurane anesthesia: a randomized controlled trial. Korean J Anesthesiol. 2015; 68:43–9. DOI: 10.4097/kjae.2015.68.1.43. PMID: 25664155. PMCID: PMC4318865.24. Kim K, Kim WJ, Choi DK, Lee YK, Choi IC, Sim JY. The analgesic efficacy and safety of nefopam in patient-controlled analgesia after cardiac surgery: A randomized, double-blind, prospective study. J Int Med Res. 2014; 42:684–92. DOI: 10.1177/0300060514525351. PMID: 24691459.25. Tobin WE, Gold RH. Nefopam hydrochloride: a novel muscle relaxant. J Clin Pharmacol New Drugs. 1972; 12:230–8. DOI: 10.1002/j.1552-4604.1972.tb00167.x.26. Bolt AG, Graham G, Wilson P. Stereoselective demethylation of the enantiomers of nefopam, an experimental antidepressant and skeletal muscle relaxant. Xenobiotica. 1974; 4:355–63. DOI: 10.3109/00498257409052111. PMID: 4842015.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The efficacy of sevolflurane inhalation alone or its combination with intravenous remifentanil against withdrawal movements on rocuronium injection in children
- The influence of age and gender on remifentanil EC(50) for preventing rocuronium induced withdrawal movements
- Prevention of Rocuronium-induced Withdrawal Movement in Children: A Comparison of Remifentanil with Lidocaine
- Nefopam does not influence onset and recovery profiles of rocuronium-induced neuromuscular block: a prospective, double-blinded, randomized, controlled study
- Single pretreatment of remifentanil may reduce pain after propofol and rocuronium injection in rapid sequence induction