Ann Dermatol.
2012 May;24(2):144-150.
A Randomized, Open-Label, Multicenter Trial of Topical Tacrolimus for the Treatment of Pruritis in Patients with Atopic Dermatitis
- Affiliations
-
- 1Department of Dermatology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan. takeuchs@dermatol.med.kyushu-u.ac.jp
- 2Department of Dermatology, Faculty of Medicine, University of Tokyo, Bunkyo-ku, Japan.
- 3Department of Medical Informatics, Kyushu University Hospital, Fukuoka, Japan.
- 4Department of Dermatology, Social Insurance Chuo General Hospital, Shinjuku-ku, Japan.
- 5Department of Dermatology, Saitama Medical University, Iruma-gun, Japan.
- 6Department of Dermatology, St. Marianna University School of Medicine, Kawasaki, Japan.
- 7Department of Dermatology, Hiroshima University, Hiroshima, Japan.
- 8Division of Dermatology, Department of Medicine, National Center for Child Health and Development, Setagaya-ku, Japan.
- 9Division of Allergy, Department of Medicine, National Center for Child Health and Development, Setagaya-ku, Japan.
Abstract
- BACKGROUND
Pruritis caused by atopic dermatitis (AD) is not always well controlled by topical corticosteroid therapy, but use of tacrolimus often helps to soothe such intractable pruritis in clinical settings.
OBJECTIVE
To determine the anti-pruritic efficacy of topical tacrolimus in treating AD in induction and maintenance therapy.
METHODS
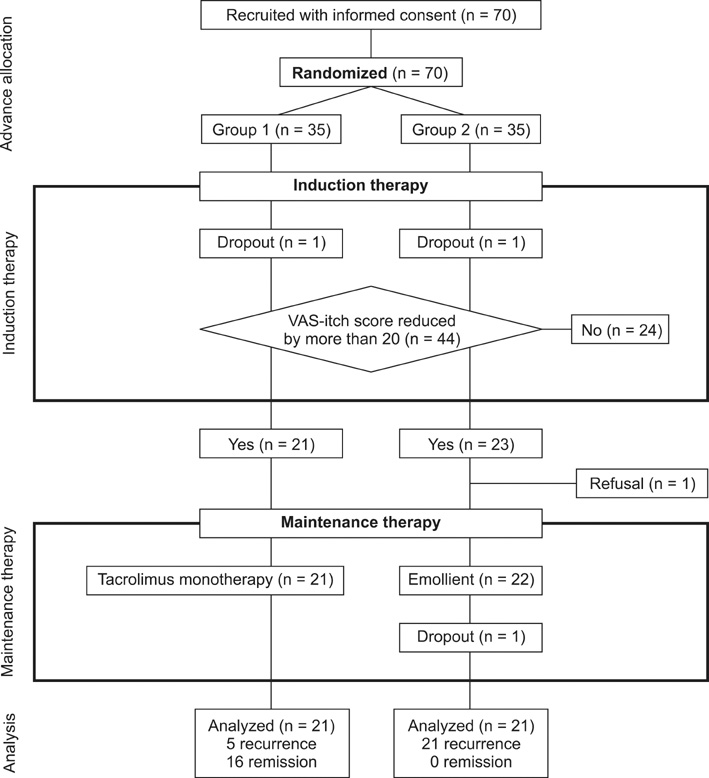
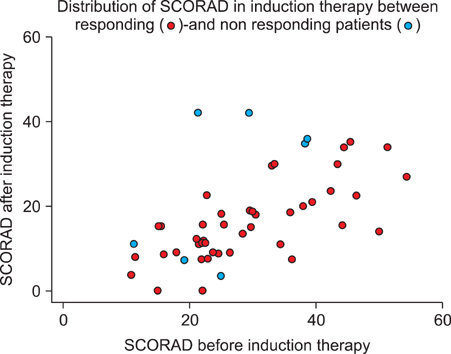
Prior to the study, patients were randomly allocated into two groups, induction therapy followed by tacrolimus monotherapy maintenance, and induction therapy followed by emollient-only maintenance. In the induction therapy, the patients were allowed to use topical tacrolimus and emollients in addition to a low dose (<10 g/week) of topical steroids. Patients showing relief from pruritis were allowed to proceed to maintenance therapy. Recurrence of pruritis in maintenance therapy was examined as a major endpoint.
RESULTS
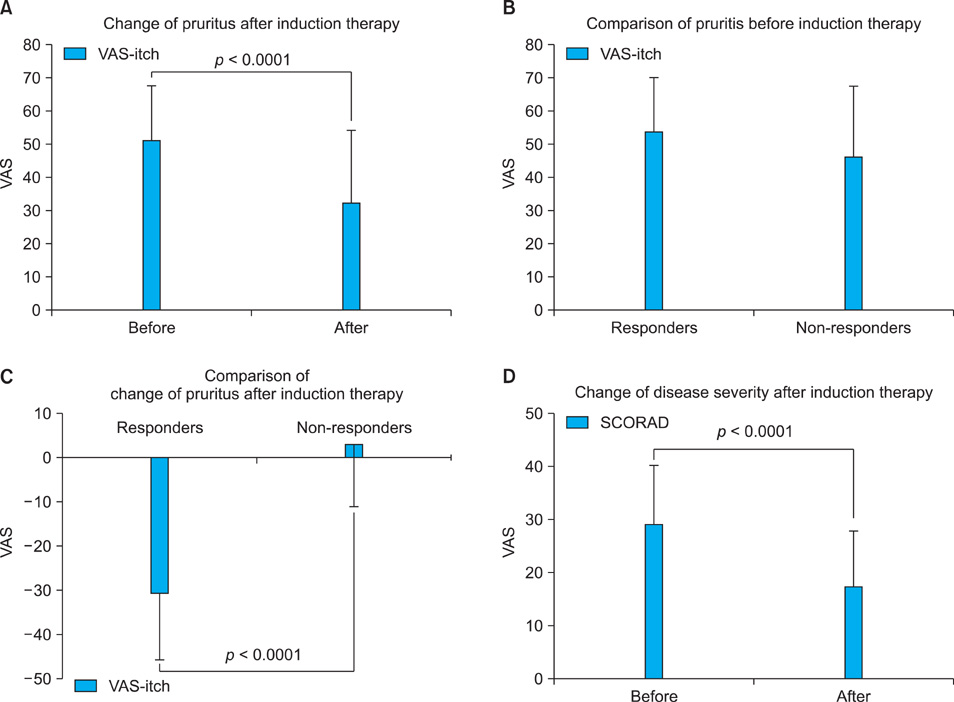
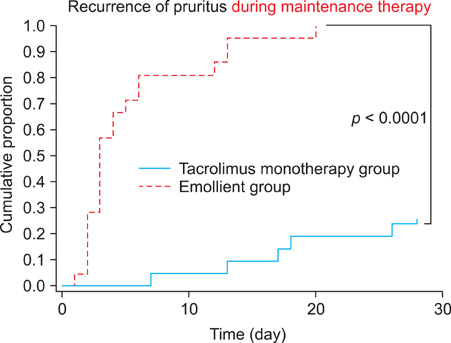
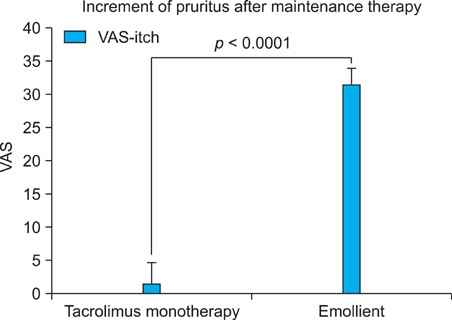
Two-thirds of patients (44/68; 64.7%) showed relief from pruritis after induction therapy. Pruritis recurred in 23.8% (5/21) of the tacrolimus monotherapy group and in 100% (21/21) of the emollient group during maintenance period, a difference that was statistically significant.
CONCLUSION
Use of topical tacrolimus is effective in controlling pruritis of AD compared to emollient.
MeSH Terms
Figure
Reference
-
1. Takeuchi M, Ueda H. Increase of adult atopic dermatitis (AD) in recent Japan. Environ Dermatol. 2000. 7:133–136.2. Yamamoto S. Prevalence and exacerbation factors of atopic dermatitis. Skin Allergy Frontier. 2003. 1:85–90.3. Ikoma A, Steinhoff M, Ständer S, Yosipovitch G, Schmelz M. The neurobiology of itch. Nat Rev Neurosci. 2006. 7:535–547.
Article4. Rossi R, Johansson O. Cutaneous innervation and the role of neuronal peptides in cutaneous inflammation: a minireview. Eur J Dermatol. 1998. 8:299–306.5. Ständer S, Steinhoff M, Schmelz M, Weisshaar E, Metze D, Luger T. Neurophysiology of pruritus: cutaneous elicitation of itch. Arch Dermatol. 2003. 139:1463–1470.6. Furue M, Terao H, Rikihisa W, Urabe K, Kinukawa N, Nose Y, et al. Clinical dose and adverse effects of topical steroids in daily management of atopic dermatitis. Br J Dermatol. 2003. 148:128–133.
Article7. Wahlgren CF. Itch and atopic dermatitis: clinical and experimental studies. Acta Derm Venereol Suppl (Stockh). 1991. 165:1–53.8. Boguniewicz M, Fiedler VC, Raimer S, Lawrence ID, Leung DY, Hanifin JM. Pediatric Tacrolimus Study Group. A randomized, vehicle-controlled trial of tacrolimus ointment for treatment of atopic dermatitis in children. J Allergy Clin Immunol. 1998. 102:637–644.
Article9. Severity scoring of atopic dermatitis: the SCORAD index. Consensus Report of the European Task Force on Atopic Dermatitis. Dermatology. 1993. 186:23–31.10. Furue M, Terao H, Moroi Y, Koga T, Kubota Y, Nakayama J, et al. Dosage and adverse effects of topical tacrolimus and steroids in daily management of atopic dermatitis. J Dermatol. 2004. 31:277–283.
Article11. Fleischer AB Jr, Ling M, Eichenfield L, Satoi Y, Jaracz E, Rico MJ, et al. Tacrolimus ointment for the treatment of atopic dermatitis is not associated with an increase in cutaneous infections. J Am Acad Dermatol. 2002. 47:562–570.
Article12. Rivard J, Lim HW. Ultraviolet phototherapy for pruritus. Dermatol Ther. 2005. 18:344–354.
Article13. Chuang TY, Heinrich LA, Schultz MD, Reizner GT, Kumm RC, Cripps DJ. PUVA and skin cancer. A historical cohort study on 492 patients. J Am Acad Dermatol. 1992. 26:173–177.14. Hon KL, Lam MC, Leung TF, Chow CM, Wong E, Leung AK. Assessing itch in children with atopic dermatitis treated with tacrolimus: objective versus subjective assessment. Adv Ther. 2007. 24:23–28.
Article15. Reitamo S, Rustin M, Ruzicka T, Cambazard F, Kalimo K, Friedmann PS, et al. European Tacrolimus Ointment Study Group. Efficacy and safety of tacrolimus ointment compared with that of hydrocortisone butyrate ointment in adult patients with atopic dermatitis. J Allergy Clin Immunol. 2002. 109:547–555.
Article16. Japanese FK-506 Ointment Study Group. Phase III study of FK-506 (Tacrolimus) ointment in patients with atopic dermatitis -Comparison study with 0.12% betamethasone valerate ointment for trunk and extremities lesions-. Nishinihon J Dermatol. 1997. 59:870–879. (article in Japanese).17. Inagaki N, Shiraishi N, Igeta K, Itoh T, Chikumoto T, Nagao M, et al. Inhibition of scratching behavior associated with allergic dermatitis in mice by tacrolimus, but not by dexamethasone. Eur J Pharmacol. 2006. 546:189–196.
Article18. Inagaki N, Shiraishi N, Igeta K, Nagao M, Kim JF, Chikumoto T, et al. Depletion of substance P, a mechanism for inhibition of mouse scratching behavior by tacrolimus. Eur J Pharmacol. 2010. 626:283–289.
Article19. Inoue T, Katoh N, Kishimoto S. Prolonged topical application of tacrolimus inhibits immediate hypersensitivity reactions by reducing degranulation of mast cells. Acta Derm Venereol. 2006. 86:13–16.
Article20. Kido M, Takeuchi S, Esaki H, Hayashida S, Furue M. Scratching behavior does not necessarily correlate with epidermal nerve fiber sprouting or inflammatory cell infiltration. J Dermatol Sci. 2010. 58:130–135.
Article21. Takeuchi S, Yasukawa F, Furue M, Katz SI. Collared mice: a model to assess the effects of scratching. J Dermatol Sci. 2010. 57:44–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Four Cases of Atopic Dermatitis with Topical Tacrolimus Therapy
- Tacrolimus ointment: An Open study for Effects on Severe Facial Atopic Dermatitis in Korean
- An Open-Label, Single-Arm, Multicenter Trial of Tacrolimus Ointment 0.1% for the Treatment of Atopic Dermatitis in the Head and Neck
- The Efficacy of Tapering Treatment with 0.1% Tacrolimus Ointment in Adult Patients with Atopic Dermatitis in Korea
- Efficacy of 0.1% Tacrolimus Ointment in Korean Patients with Atopic Dermatitis