Allergy Asthma Immunol Res.
2019 Mar;11(2):280-290. 10.4168/aair.2019.11.2.280.
Prescription Patterns and Burden of Pediatric Asthma in Korea
- Affiliations
-
- 1Department of Pediatrics, Severance Hospital, Institute of Allergy, Brain Korea 21 PLUS Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea. mhsohn@yuhs.ac
- 2Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea.
- 3Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2431859
- DOI: http://doi.org/10.4168/aair.2019.11.2.280
Abstract
- PURPOSE
This study aimed to estimate the prevalence, prescription pattern and burden of pediatric asthma in Korea by analyzing the National Health Insurance (NHI) claims data.
METHODS
We retrospectively analyzed the insurance claim records from the Korean NHI claims database from January 2010 to December 2014. Asthmatic patients were defined as children younger than 18 years, with appropriate 10th Revision of the International Classification of Diseases codes (J45 or J46) and a prescription for 1 or more asthma maintenance medications at the same date. Hospitalization and emergency department visits for asthma were defined as use of short-acting beta2-agonists during hospital visits among asthmatic patients.
RESULTS
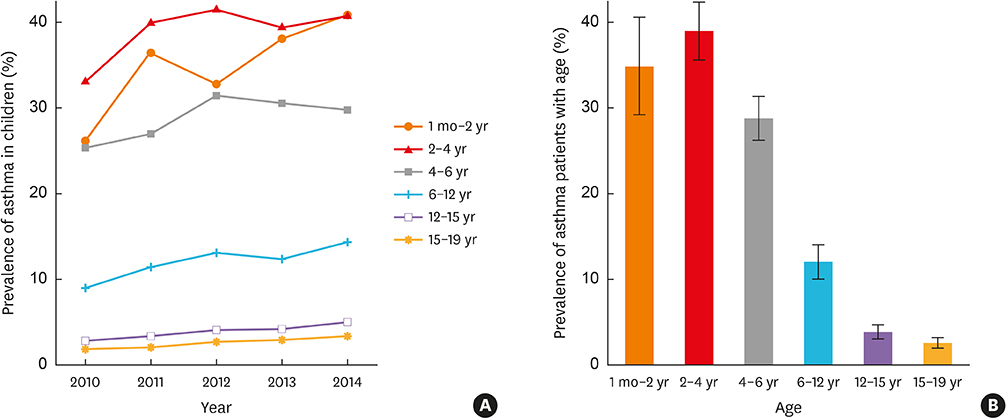
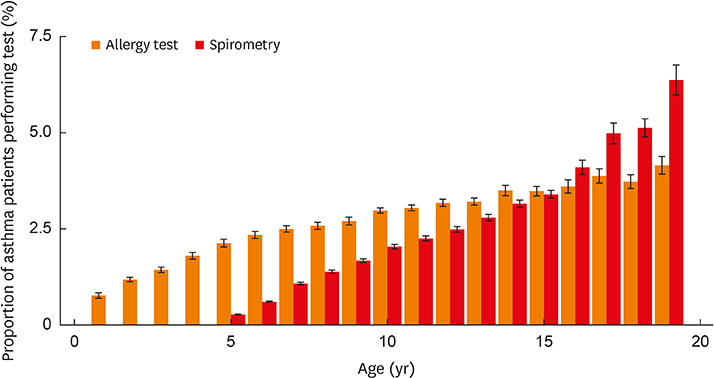
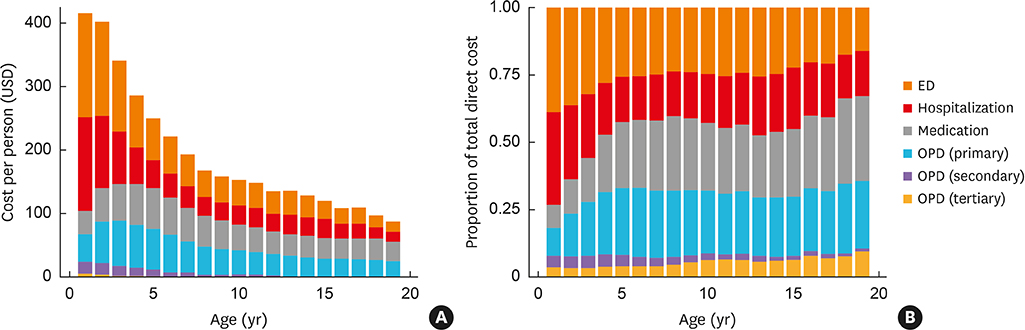
There were 1,172,807 asthmatic children in 2010, which increased steadily to 1,590,228 in 2014 in Korea. The prevalence showed an increasing trend annually for all ages. The mean prevalence by age in those older than 2 years decreased during the study period (from 39.4% in the 2-3 year age group to 2.6% in the 15-18 year age group). In an outpatient prescription, leukotriene receptor antagonists were the most commonly prescribed medication for all ages. Patients older than 6 years for whom inhaled corticosteroids were prescribed comprised less than 15% of asthmatic patients. The total direct medical cost for asthma between 2010 and 2014 ranged from $376 to $483 million. Asthma-related medical cost per person reached its peak in $366 in 2011 and decreased to $275 in 2014.
CONCLUSIONS
The prevalence of pediatric asthma increased annually and decreased with age. Individual cost of asthma showed a decreasing trend in Korean children.
Keyword
MeSH Terms
-
Adrenal Cortex Hormones
Asthma*
Child
Cost of Illness
Emergency Service, Hospital
Hospitalization
Humans
Insurance
International Classification of Diseases
Korea*
Leukotriene Antagonists
National Health Programs
Outpatients
Prescriptions*
Prevalence
Retrospective Studies
Adrenal Cortex Hormones
Leukotriene Antagonists
Figure
Cited by 2 articles
-
Associated Factors for Asthma Severity in Korean Children: A Korean Childhood Asthma Study
Eun Lee, Dae Jin Song, Woo Kyung Kim, Dong In Suh, Hey-Sung Baek, Meeyong Shin, Young Yoo, Jin Tack Kim, Ji-Won Kwon, Gwang Cheon Jang, Dae Hyun Lim, Hyeon-Jong Yang, Hwan Soo Kim, Ju-Hee Seo, Sung-Il Woo, Hyung Young Kim, Youn Ho Shin, Ju Suk Lee, Jisun Yoon, Sungsu Jung, Minkyu Han, Eunjin Eom, Jinho Yu
Allergy Asthma Immunol Res. 2020;12(1):86-98. doi: 10.4168/aair.2020.12.1.86.Usefulness of bronchodilator response as an index of asthma control in children
Jong Deok Kim, Soo Yeon Kim, Yoon Hee Kim, Kyung Won Kim, Myung Hyun Sohn, In Suk Sol
Allergy Asthma Respir Dis. 2019;7(2):92-98. doi: 10.4168/aard.2019.7.2.92.
Reference
-
1. Lee-Sarwar KA, Bacharier LB, Litonjua AA. Strategies to alter the natural history of childhood asthma. Curr Opin Allergy Clin Immunol. 2017; 17:139–145.
Article2. Bahadori K, Doyle-Waters MM, Marra C, Lynd L, Alasaly K, Swiston J, et al. Economic burden of asthma: a systematic review. BMC Pulm Med. 2009; 9:24.
Article3. Nunes C, Pereira AM, Morais-Almeida M. Asthma costs and social impact. Asthma Res Pract. 2017; 3:1.
Article4. Chung F, Barnes N, Allen M, Angus R, Corris P, Knox A, et al. Assessing the burden of respiratory disease in the UK. Respir Med. 2002; 96:963–975.
Article5. Pearce N, Aït-Khaled N, Beasley R, Mallol J, Keil U, Mitchell E, et al. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2007; 62:758–766.
Article6. Kälvesten L, Bråbäck L. Time trend for the prevalence of asthma among school children in a Swedish district in 1985–2005. Acta Paediatr. 2008; 97:454–458.
Article7. Lee YL, Hwang BF, Lin YC, Guo YL. Taiwan Childhood Allergy Survey Group. Time trend of asthma prevalence among school children in Taiwan. Pediatr Allergy Immunol. 2007; 18:188–195.8. Schröder PC, Li J, Wong GW, Schaub B. The rural-urban enigma of allergy: what can we learn from studies around the world? Pediatr Allergy Immunol. 2015; 26:95–102.
Article9. Park SY, Kim JH, Kim HJ, Seo B, Kwon OY, Chang HS, et al. High prevalence of asthma in elderly women: findings from a Korean national health database and adult asthma cohort. Allergy Asthma Immunol Res. 2018; 10:387–396.
Article10. Lee SI. Prevalence of childhood asthma in Korea: International Study of Asthma and Allergies in childhood. Allergy Asthma Immunol Res. 2010; 2:61–64.
Article11. Kwon S. Payment system reform for health care providers in Korea. Health Policy Plan. 2003; 18:84–92.
Article12. Koo BK, Lee JH, Kim J, Jang EJ, Lee CH. Prevalence of gestational diabetes mellitus in Korea: a National Health Insurance database study. PLoS One. 2016; 11:e0153107.
Article13. Song SO, Jung CH, Song YD, Park CY, Kwon HS, Cha BS, et al. Background and data configuration process of a nationwide population-based study using the Korean national health insurance system. Diabetes Metab J. 2014; 38:395–403.
Article14. Gergen PJ. Understanding the economic burden of asthma. J Allergy Clin Immunol. 2001; 107:Suppl. S445–S448.
Article15. Saha S, Gerdtham UG. Cost of illness studies on reproductive, maternal, newborn, and child health: a systematic literature review. Health Econ Rev. 2013; 3:24.
Article16. Jang Y, Shin A. Sex-based differences in asthma among preschool and school-aged children in Korea. PLoS One. 2015; 10:e0140057.
Article17. Kim BK, Kim JY, Kang MK, Yang MS, Park HW, Min KU, et al. Allergies are still on the rise? A 6-year nationwide population-based study in Korea. Allergol Int. 2016; 65:186–191.
Article18. Rabe KF, Adachi M, Lai CK, Soriano JB, Vermeire PA, Weiss KB, et al. Worldwide severity and control of asthma in children and adults: the global asthma insights and reality surveys. J Allergy Clin Immunol. 2004; 114:40–47.
Article19. Global Initiative for Asthma (GINA). Diagnosis and management of asthma in children 5 years and younger 2015 [Internet]. place unknown: Global Initiative for Asthma;2015. cited 2017 Jan 30. Available from: http://ginasthma.org.20. Engelkes M, Janssens HM, de Jongste JC, Sturkenboom MC, Verhamme KM. Prescription patterns, adherence and characteristics of non-adherence in children with asthma in primary care. Pediatr Allergy Immunol. 2016; 27:201–208.
Article21. Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United States, 2001–2010. Vital Health Stat 3. 2012; 1–58.22. Klok T, Kaptein AA, Duiverman EJ, Brand PL. High inhaled corticosteroids adherence in childhood asthma: the role of medication beliefs. Eur Respir J. 2012; 40:1149–1155.
Article23. Yang CL, Simons E, Foty RG, Subbarao P, To T, Dell SD. Misdiagnosis of asthma in schoolchildren. Pediatr Pulmonol. 2017; 52:293–302.
Article24. Looijmans-van den Akker I, van Luijn K, Verheij T. Overdiagnosis of asthma in children in primary care: a retrospective analysis. Br J Gen Pract. 2016; 66:e152–e157.
Article25. Yang JH, Kim M, Park YT, Lee EK, Jung CY, Kim S. The effect of the introduction of a nationwide DUR system where local DUR systems are operating--the Korean experience. Int J Med Inform. 2015; 84:912–919.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Global burden of asthma among children and adolescents with projections to 2050: a comprehensive review and forecasted modeling study
- A Survey of Awareness and Application of the Guideline for Diagnosis and Management of Childhood Asthma
- Studies and proposals of childhood asthma in Korea
- Asthma and Rhinitis in South America: How Different They are From Other Parts of the World
- A Survey of the Prescription Patterns of Allergen Immunotherapy in Korea