J Korean Neurosurg Soc.
2018 Nov;61(6):661-668. 10.3340/jkns.2018.0150.
Spinal Deformity Surgery : It Becomes an Essential Part of Neurosurgery
- Affiliations
-
- 1Department of Neurosurgery, Spine Center, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. beast2625@snu.ac.kr
- KMID: 2428107
- DOI: http://doi.org/10.3340/jkns.2018.0150
Abstract
- Among the spinal disorders, the treatment approach for spinal deformities has been discussed least among department of neurosurgery. But nowadays, more and more neurosurgeons are interested in spinal deformities as well as complex spinal disorders and are doing not a few surgeries for these kinds of disease. Nevertheless, it is mandatory to understand the course of spinal deformity, principles of treatment, and surgical outcomes and complications. Understanding of the biology, biomechanics and metallurgy of the spine and instrumentation are also required for successful spinal deformity surgery. We need senior mentors and good surgical and neurophysiologic monitoring team. Knowledge of spinal deformity may be augmented with spine fellowships and surgical experience. Step by step training such as basic knowledge, orthopedic as well as neurosurgical disciplines and surgical skills would be mandatory. Neurosurgeons can have several advantages for spinal deformity surgeries. By high-level technical ability of the spinal cord handling to preserve neurological function and familiarity with microscopic surgery, better synergistic effect could be expected. A fundamental understanding of pediatric spinal deformity and growing spine should be needed for spinal deformity surgery.
Keyword
MeSH Terms
Figure
Cited by 2 articles
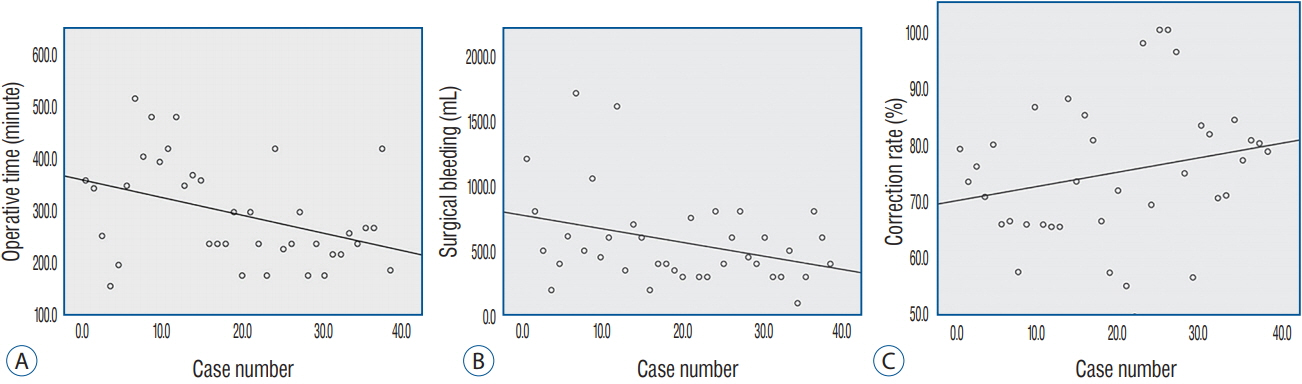
-
Surgical Outcomes and Complications Following All Posterior Approach for Spinal Deformity Associated with Neurofibromatosis Type-1
Byoung-Joo Park, Seung-Jae Hyun, Seong-Hyun Wui, Jong-Myung Jung, Ki-Jeong Kim, Tae-Ahn Jahng
J Korean Neurosurg Soc. 2020;63(6):738-746. doi: 10.3340/jkns.2019.0218.Systematic Review of Reciprocal Changes after Spinal Reconstruction Surgery : Do Not Miss the Forest for the Trees
Chang-Wook Kim, Seung-Jae Hyun, Ki-Jeong Kim
J Korean Neurosurg Soc. 2021;64(6):843-852. doi: 10.3340/jkns.2020.0234.
Reference
-
References
1. Albert TJ, Purtill J, Mesa J, McIntosh T, Balderston RA. Health outcome assessment before and after adult deformity surgery. A prospective study. Spine (Phila Pa 1976). 20:2002–2004. discussion p2005. 1995.2. Benzel EC. The evolving presence of spinal neurosurgery in the spectrum of neurological surgery. Neurosurgery. 60:591–592. 2007.
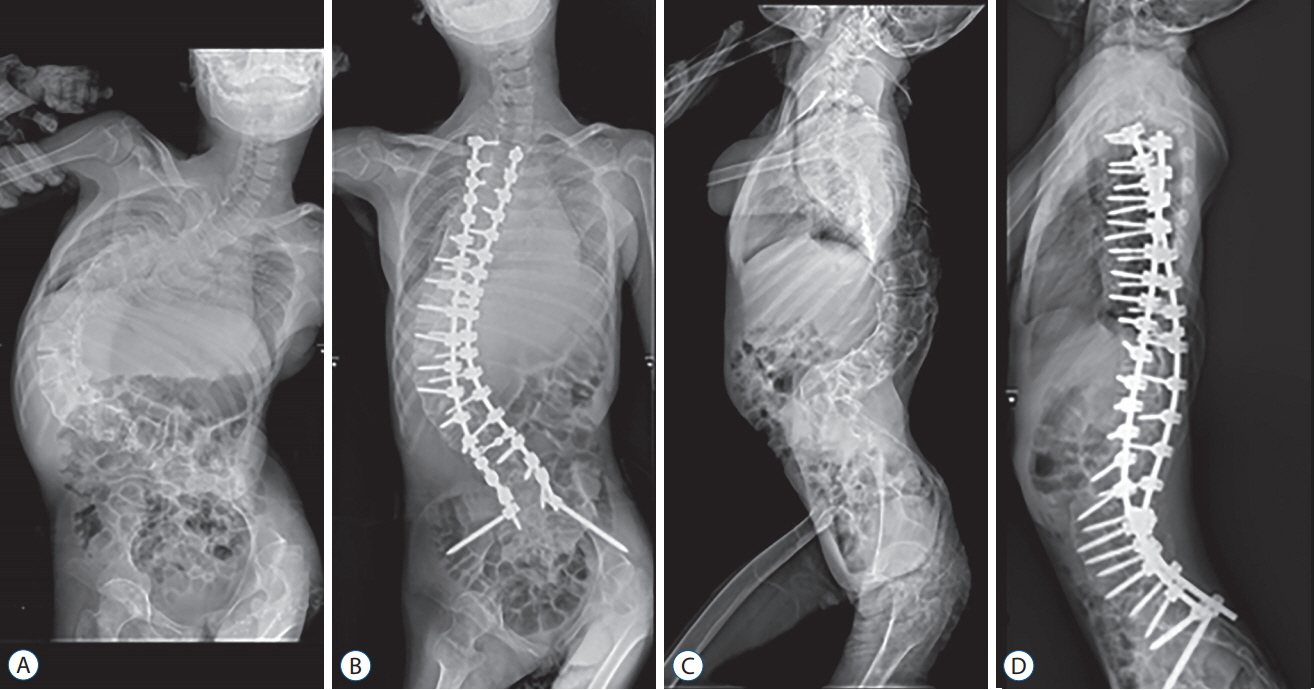
Article3. Bess S, Boachie-Adjei O, Burton D, Cunningham M, Shaffrey C, Shelokov A, et al. Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine (Phila Pa 1976). 34:2186–2190. 2009.
Article4. Bradford DS, Tay BK, Hu SS. Adult scoliosis: surgical indications, operative management, complications, and outcomes. Spine (Phila Pa 1976). 24:2617–2629. 1999.
Article5. Bridwell KH, Lenke LG, Baldus C, Blanke K. Major intraoperative neurologic deficits in pediatric and adult spinal deformity patients. Incidence and etiology at one institution. Spine (Phila Pa 1976). 23:324–331. 1998.
Article6. Buchowski JM, Bridwell KH, Lenke LG, Kuhns CA, Lehman RA Jr, Kim YJ, et al. Neurologic complications of lumbar pedicle subtraction osteotomy: a 10-year assessment. Spine (Phila Pa 1976). 32:2245–2252. 2007.7. Cho SK, Bridwell KH, Lenke LG, Yi JS, Pahys JM, Zebala LP, et al. Major complications in revision adult deformity surgery: risk factors and clinical outcomes with 2- to 7-year follow-up. Spine (Phila Pa 1976). 37:489–500. 2012.8. Choi HY, Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Effectiveness and safety of tranexamic acid in spinal deformity surgery. J Korean Neurosurg Soc. 60:75–81. 2017.
Article9. Choi HY, Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Surgical and radiographic outcomes after pedicle subtraction osteotomy according to surgeon’s experience. Spine (Phila Pa 1976). 42:E795–E801. 2017.
Article10. Clark AJ, Garcia RM, Keefe MK, Koski TR, Rosner MK, Smith JS, et al. Results of the AANS membership survey of adult spinal deformity knowledge: impact of training, practice experience, and assessment of potential areas for improved education: clinical article. J Neurosurg Spine. 21:640–647. 2014.
Article11. Daniels AH, Ames CP, Smith JS, Hart RA. Variability in spine surgery procedures performed during orthopaedic and neurological surgery residency training: an analysis of ACGME case log data. J Bone Joint Surg Am. 96:e196. 2014.12. Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity: luque-galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976). 27:776–786. 2002.
Article13. Han S, Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Comparative study between cobalt chrome and titanium alloy rods for multilevel spinal fusion: proximal junctional kyphosis more frequently occurred in patients having cobalt chrome rods. World Neurosurg. 103:404–409. 2017.
Article14. Hyun SJ, Han S, Kim KJ, Jahng TA, Kim YJ, Rhim SC, et al. Adolescent idiopathic scoliosis surgery by a neurosurgeon: learning curve for neurosurgeons. World neurosurgery. 110:e129–e134. 2018.
Article15. Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ. Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine. 14:126–132. 2017.
Article16. Hyun SJ, Lenke LG, Kim YC, Koester LA, Blanke KM. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976). 39:1899–1904. 2014.
Article17. Hyun SJ, Rhim SC. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients : a long-term follow-up data. J Korean Neurosurg Soc. 47:95–101. 2010.
Article18. Kim HJ, Lenke LG, Shaffrey CI, Van Alstyne EM, Skelly AC. Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery: a systematic review. Spine (Phila Pa 1976). 37(22 Suppl):S144–S164. 2012.19. Kim YJ, Hyun SJ, Cheh G, Cho SK, Rhim SC. Decision making algorithm for adult spinal deformity surgery. J Korean Neurosurg Soc. 59:327–333. 2016.
Article20. Konczalik W, Elsayed S, Boszczyk B. Experience of a fellowship in spinal surgery: a quantitative analysis. Eur Spine J 23 Suppl. 1:S40–S54. 2014.
Article21. Kriss TC, Kriss VM. History of the operating microscope: from magnifying glass to microneurosurgery. Neurosurgery. 42:899–907. discussion 907-908. 1998.
Article22. Kwon JW, Hyun SJ, Han SH, Kim KJ, Jahng TA. Pyogenic vertebral osteomyelitis: clinical features, diagnosis, and treatment. Korean J Spine. 14:27–34. 2017.
Article23. Lapp MA, Bridwell KH, Lenke LG, Daniel Riew K, Linville DA, Eck KR, et al. Long-term complications in adult spinal deformity patients having combined surgery a comparison of primary to revision patients. Spine (Phila Pa 1976). 26:973–983. 2001.
Article24. Lee BH, Hyun SJ, Kim KJ, Jahng TA, Kim YJ, Kim HJ. Clinical and radiological outcomes of posterior vertebral column resection for severe spinal deformities. J Korean Neurosurg Soc. 61:251–257. 2018.
Article25. Lee BH, Hyun SJ, Park JH, Kim KJ. Single stage posterior approach for total resection of presacral giant schwannoma: a technical case report. Korean J Spine. 14:89–92. 2017.
Article26. Lee CH, Chung CK, Jang JS, Kim SM, Chin DK, Lee JK. ‘Lumbar degenerative kyphosis’ is not byword for degenerative sagittal imbalance: time to replace a misconception. J Korean Neurosurg Soc. 60:125–129. 2017.
Article27. Makhni MC, Shillingford JN, Laratta JL, Hyun SJ, Kim YJ. Restoration of sagittal balance in spinal deformity surgery. J Korean Neurosurg Soc. 61:167–179. 2018.
Article28. Park YS, Hyun SJ, Kim KJ, Jahng TA. Multiple intradural disc herniations masquerading as intradural extramedullary tumors: a case report and review of the literature. Korean J Spine. 13:30–32. 2016.
Article29. Park YS, Hyun SJ, Kim KJ, Jahng TA. Plasmacytoma to the axis mimicking metastatic paraganglioma: circumferential reconstruction via posterior approach. Korean J Spine. 12:283–286. 2015.
Article30. Pejrona M, Ristori G, Villafañe JH, Pregliasco FE, Berjano P. Does specialty matter? A survey on 176 Italian neurosurgeons and orthopedic spine surgeons confirms similar competency for common spinal conditions and supports multidisciplinary teams in comprehensive and complex spinal care. Spine J. 18:1498–1503. 2018.
Article31. Potter BK, Lenke LG, Kuklo TR. Prevention and management of iatrogenic flatback deformity. J Bone Joint Surg Am 86-A. 1793–1808. 2004.
Article32. Schlenk RP, Stewart T, Benzel EC. The biomechanics of iatrogenic spinal destabilization and implant failure. Neurosurg Focus. 15:E2. 2003.
Article33. Schwab F, Dubey A, Gamez L, El Fegoun AB, Hwang K, Pagala M, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 30:1082–1085. 2005.
Article34. Schwab F, Lafage V, Farcy JP, Bridwell K, Glassman S, Ondra S, et al. Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis: application of the new adult deformity classification. Spine (Phila Pa 1976). 32:2723–2730. 2007.
Article35. Seicean A, Alan N, Seicean S, Neuhauser D, Benzel EC, Weil RJ. Surgeon specialty and outcomes after elective spine surgery. Spine (Phila Pa 1976). 39:1605–1613. 2014.
Article36. Seyal M, Mull B. Mechanisms of signal change during intraoperative somatosensory evoked potential monitoring of the spinal cord. J Clin Neurophysiol. 19:409–415. 2002.
Article37. Shapiro GS, Taira G, Boachie-Adjei O. Results of surgical treatment of adult idiopathic scoliosis with low back pain and spinal stenosis: a study of long-term clinical radiographic outcomes. Spine (Phila Pa 1976). 28:358–363. 2003.
Article38. Slosar PJ. Indications and outcomes of reconstructive surgery in chronic pain of spinal origin. Spine (Phila Pa 1976). 27:2555–2562. discussion 2563. 2002.
Article39. Takahashi S, Delécrin J, Passuti N. Surgical treatment of idiopathic scoliosis in adults: an age-related analysis of outcome. Spine (Phila Pa 1976). 27:1742–1748. 2002.40. Uluçc K, Kujoth GC, Baskaya MK. Operating microscopes: past, present, and future. Neurosurg Focus. 27:E4. 2009.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- From the Spinopelvic Parameters to Global Alignment and Proportion Scores in Adult Spinal Deformity
- Etiology, diagnosis, and treatment of iatrogenic spinal deformity
- Minimally Invasive Spinal Surgery for Adult Spinal Deformity
- One-Step Ventro-Posterior Fusion via Transpedicular Approach for L1 Burst Fracture by Use of Expandable Cage
- Predicting Proximal Junctional Kyphosis After Adult Spinal Deformity Surgery: A Step Towards True “Precision” Medicine?: Commentary on “Development and Validation of an Online Calculator to Predict Proximal Junctional Kyphosis After Adult Spinal Deformity Surgery Using Machine Learning”