J Korean Soc Radiol.
2018 Dec;79(6):323-331. 10.3348/jksr.2018.79.6.323.
The Effectiveness of Ultrasound-Guided Thoracic Paravertebral Block for Percutaneous Radiofrequency Ablation of Hepatic Tumors: A Pilot Study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 2Department of Radiology, Presbyterian Medical Center, Jeonju, Korea. turtle28@naver.com
- 3Department of Anesthesiology and Pain Medicine, Presbyterian Medical Center, Jeonju, Korea.
- 4Department of Preventive Medicine, Chonbuk National University Medical School, Jeonju, Korea.
- KMID: 2427380
- DOI: http://doi.org/10.3348/jksr.2018.79.6.323
Abstract
- PURPOSE
The purpose of this study was to evaluate the effectiveness of thoracic paravertebral block (TPVB) for management of pain during and after percutaneous radiofrequency ablation (RFA) of hepatic tumor.
MATERIALS AND METHODS
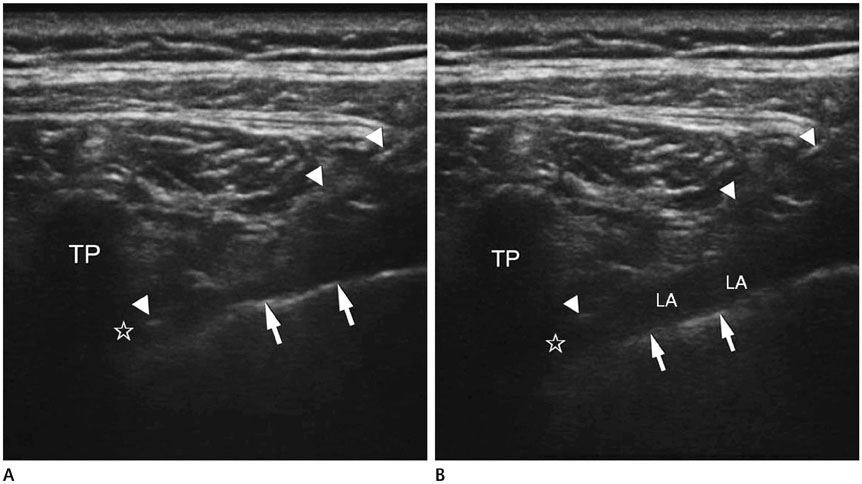
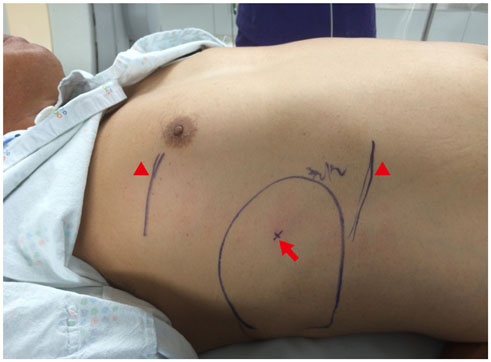
All patients were divided into non-TPVB (4 patients, 4 sessions of RFA for 4 tumors) and TPVB group (5 patients, 7 sessions of RFAs for 7 tumors). Ultrasound (US)-guided TPVB was performed at T7 level. The 15 mL of 0.375% ropivacaine was injected into right paravertebral space before RFA. If patients complained pain and asked analgesics or experienced pain with verbal numerical rating scale (VNRS) of more than 4, fentanyl 25 µg (up to 100 µg), pethidine 25 mg, and midazolam 0.05 mg/kg (up to 5 mg) were sequentially given intravenously during RFA.
RESULTS
Total intravenous morphine equivalence of analgesics before, during, and after RFA was 129.1 mg and 0.0 mg in non-TPVB and TPVB group, respectively.
CONCLUSION
US-guided TPVB may be an effective and safe anesthetic method for decreasing or eliminating pain during and after RFA for hepatic tumor and helpful in decreasing the usage of opioids.
MeSH Terms
Figure
Reference
-
1. Salhab M, Canelo R. An overview of evidence-based management of hepatocellular carcinoma: a meta-analysis. J Cancer Res Ther. 2011; 7:463–475.
Article2. Wu YZ, Li B, Wang T, Wang SJ, Zhou YM. Radiofrequency ablation vs hepatic resection for solitary colorectal liver metastasis: a meta-analysis. World J Gastroenterol. 2011; 17:4143–4148.
Article3. Carrafiello G, Laganà D, Cotta E, Mangini M, Fontana F, Bandiera F, et al. Radiofrequency ablation of intrahepatic cholangiocarcinoma: preliminary experience. Cardiovasc Intervent Radiol. 2010; 33:835–839.4. Yang W, Chen MH, Yin SS, Yan K, Gao W, Wang YB, et al. Radiofrequency ablation of recurrent hepatocellular carcinoma after hepatectomy: therapeutic efficacy on early and late phase recurrence. AJR Am J Roentgenol. 2006; 186:5 Suppl. S275–S283.5. Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD, Dupuy DE, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. Radiology. 2005; 235:728–739.
Article6. Lee S, Rhim H, Kim YS, Choi D, Lee WJ, Lim HK, et al. Percutaneous radiofrequency ablation of hepatocellular carcinomas: factors related to intraprocedural and postprocedural pain. AJR Am J Roentgenol. 2009; 192:1064–1070.
Article7. Park YR, Kim YS, Rhim H, Lim HK, Choi D, Lee WJ. Arterial enhancement of hepatocellular carcinoma before radiofrequency ablation as a predictor of postablation local tumor progression. AJR Am J Roentgenol. 2009; 193:757–763.
Article8. Takaki H, Yamakado K, Sakurai H, Nakatsuka A, Shiraki K, Iasaji S, et al. Radiofrequency ablation combined with chemoembolization: treatment of recurrent hepatocellular carcinomas after hepatectomy. AJR Am J Roentgenol. 2011; 197:488–494.
Article9. Kim YK, Kim CS, Chung GH, Han YM, Lee SY, Jin GY, et al. Radiofrequency ablation of hepatocellular carcinoma in patients with decompensated cirrhosis: evaluation of therapeutic efficacy and safety. AJR Am J Roentgenol. 2006; 186:5 Suppl. S261–S268.
Article10. Shibata T, Shibata T, Maetani Y, Isoda H, Hiraoka M. Radiofrequency ablation for small hepatocellular carcinoma: prosepctive comparison of internally cooled electrode and expandable electrode. Radiology. 2006; 238:346–353.
Article11. Minami Y, Kudo M. Radiofrequency ablation of hepatocellular carcinoma: a literature review. Int J Hepatol. 2011; 2011:104685.
Article12. Chen MH, Yang W, Yan K, Gao W, Dai Y, Wang YB, et al. Treatment efficacy of radiofrequency ablation of 338 patients with hepatic malignant tumor and the relevant complications. World J Gastroenterol. 2005; 11:6395–6401.
Article13. Richardson J, Lönnqvist PA. Thoracic paravertebral block. Br J Anaesth. 1998; 81:230–238.14. Korean Liver Cancer Study Group (KLCSG). National Cancer Center, Korea (NCC). 2014 KLCSG-NCC Korea practice guideline for the management of hepatocellular carcinoma. Gut Liver. 2015; 9:267–231.15. Ripamonti C, Groff L, Brunelli C, Polastri D, Stavrakis A, De Conno F. Switching from morphine to oral methadone in treating cancer pain: what is the equianalgesic dose ratio. J Clin Oncol. 1998; 16:3216–3221.
Article16. Mercadante S, Casuccio A, Fulfaro F, Groff L, Boffi R, Villari P, et al. Switching from morphine to methadone to improve analgesia and tolerability in cancer patients: a prospective study. J Clin Oncol. 2001; 19:2898–2904.
Article17. Karmakar MK. Thoracic paravertebral block. Anesthesiology. 2001; 95:771–780.
Article18. Cheema SP, Ilsley D, Richardson J, Sabanathan S. A thermographic study of paravertebral analgesia. Anaesthesia. 1995; 50:118–121.
Article19. Lönnqvist PA, MacKenzie J, Soni AK, Conacher ID. Paravertebral blockade. Failure rate and complications. Anaesthesia. 1995; 50:813–881.
Article20. Cheung Ning M, Karmakar MK. Right thoracic paravertebral anaesthesia for percutaneous radiofrequency ablation of liver tumours. Br J Radiol. 2011; 84:785–789.
Article21. Gazzera C, Fonio P, Faletti R, Dotto MC, Gobbi F, Donadio P, et al. Role of paravertebral block anaesthesia during percutaneous transhepatic thermoablation. Radiol Med. 2014; 119:549–557.
Article22. Piccioni F, Fumagalli L, Garbagnati F, Di Tolla G, Mazzaferro V, Langer M. Thoracic paravertebral anesthesia for percutaneous radiofrequency ablation of hepatic tumors. J Clin Anesth. 2014; 26:271–275.
Article23. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006; 367:1618–1625.
Article24. Macrae WA. Chronic post-surgical pain: 10 years on. Br J Anaesth. 2008; 101:77–86.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasound-guided Aspiration of the Iatrogenic Pneumothorax Caused by Paravertebral Block: A Case Report
- Ultrasound Guided Thoracic Paravertebral Space Block for Chronic Intractable Upper Back Pain
- Recent developments in endoscopic ultrasound-guided ablation treatment
- Ultrasound (US)-Guided Ablation of Thyroid Nodules
- Percutaneous Adrenal Radiofrequency Ablation: A Short Review for Endocrinologists