Yonsei Med J.
2016 Nov;57(6):1324-1328. 10.3349/ymj.2016.57.6.1324.
Prognostic Value of Extranodal Extension in Thyroid Cancer: A Meta-Analysis
- Affiliations
-
- 1Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea.
- 2Department of Nuclear Medicine and Biomedical Research Institute, Pusan National University Hospital, Busan, Korea. pnuhnm@gmail.com
- 3Department of Nuclear Medicine, Chung-Ang University College of Medicine, Seoul, Korea. ethmoid@daum.net
- KMID: 2427148
- DOI: http://doi.org/10.3349/ymj.2016.57.6.1324
Abstract
- PURPOSE
Thyroid cancer is the most common endocrine cancer and its incidence has continuously increased in the last three decades all over the world. We aimed to evaluate the prognostic value of extranodal extension (ENE) of thyroid cancer.
MATERIALS AND METHODS
We performed a systematic search of MEDLINE (from inception to June 2014) and EMBASE (from inception to June 2014) for English-language publication. The inclusion criteria were studies of thyroid cancer that reported the prognostic value of ENE in thyroid cancer. Reviews, abstracts, and editorial materials were excluded, and duplicate data were removed. Two authors performed the data extraction independently.
RESULTS
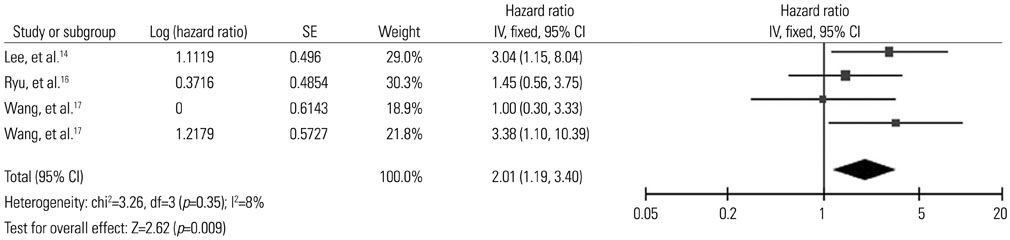
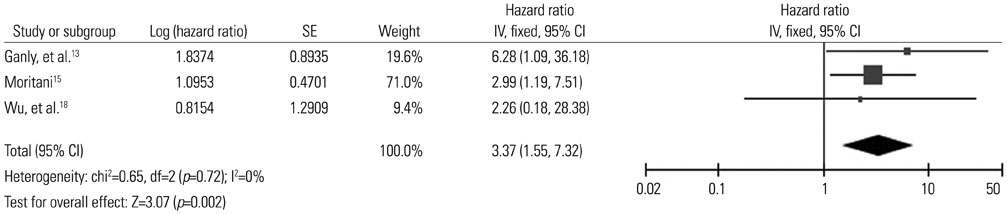
6 studies including 1830 patients were eligible for inclusion in the study. All patients included in the meta-analysis had papillary thyroid cancer (PTC). Recurrence-free survival was analyzed based on 3 studies. The pooled hazard ratio for recurrence was 2.01 [95% confidence interval (CI) 1.19-3.40, p=0.009]. Disease-specific survival was analyzed based on 3 studies with 973 patients. Patients of PTC with ENE showed 3.37-fold higher risk of death from the disease (95% CI 1.55-7.32, p=0.002).
CONCLUSION
ENE should be considered to be a poor prognostic marker in thyroid cancer; such knowledge might improve the management of individual patients. This might facilitate the planning of appropriate ablation therapy and tailored patient follow-up from the beginning of treatment.
Keyword
MeSH Terms
-
Carcinoma/*mortality/*secondary/surgery
Carcinoma, Papillary
Disease-Free Survival
Humans
Lymph Node Excision
Lymph Nodes/*pathology/surgery
Lymphatic Metastasis
Male
Neoplasm Recurrence, Local/mortality/*pathology/surgery
Prognosis
Proportional Hazards Models
Risk
Thyroid Neoplasms/*mortality/*pathology/secondary/surgery
Thyroidectomy
Treatment Outcome
Figure
Cited by 2 articles
-
mRNA Expression of
SLC5A5 andSLC2A Family Genes in Papillary Thyroid Cancer: An Analysis of The Cancer Genome Atlas
Sunghwan Suh, Yun Hak Kim, Tae Sik Goh, Dae Cheon Jeong, Chi-Seung Lee, Jeon Yeob Jang, Wonjae Cha, Myoung-Eun Han, Seong-Jang Kim, In Joo Kim, Kyoungjune Pak
Yonsei Med J. 2018;59(6):746-753. doi: 10.3349/ymj.2018.59.6.746.Prognostic Implications of Extranodal Extension in Relation to Colorectal Cancer Location
Chan Wook Kim, Jihun Kim, Yangsoon Park, Dong-Hyung Cho, Jong Lyul Lee, Yong Sik Yoon, In Ja Park, Seok-Byung Lim, Chang Sik Yu, Jin Cheon Kim
Cancer Res Treat. 2019;51(3):1135-1143. doi: 10.4143/crt.2018.392.
Reference
-
1. Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R. Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol. 2013; 2013:965212.
Article2. Kweon SS, Shin MH, Chung IJ, Kim YJ, Choi JS. Thyroid cancer is the most common cancer in women, based on the data from population-based cancer registries, South Korea. Jpn J Clin Oncol. 2013; 43:1039–1046.
Article3. Lango M, Flieder D, Arrangoiz R, Veloski C, Yu JQ, Li T, et al. Extranodal extension of metastatic papillary thyroid carcinoma: correlation with biochemical endpoints, nodal persistence, and systemic disease progression. Thyroid. 2013; 23:1099–1105.
Article4. Spires JR, Robbins KT, Luna MA, Byers RM. Metastatic papillary carcinoma of the thyroid: the significance of extranodal extension. Head Neck. 1989; 11:242–246.
Article5. Yamashita H, Noguchi S, Murakami N, Kawamoto H, Watanabe S. Extracapsular invasion of lymph node metastasis is an indicator of distant metastasis and poor prognosis in patients with thyroid papillary carcinoma. Cancer. 1997; 80:2268–2272.
Article6. Yamashita H, Noguchi S, Murakami N, Toda M, Uchino S, Watanabe S, et al. Extracapsular invasion of lymph node metastasis. A good indicator of disease recurrence and poor prognosis in patients with thyroid microcarcinoma. Cancer. 1999; 86:842–849.7. Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, et al. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 2012; 22:1144–1152.
Article8. Clain JB, Scherl S, Dos Reis L, Turk A, Wenig BM, Mehra S, et al. Extrathyroidal extension predicts extranodal extension in patients with positive lymph nodes: an important association that may affect clinical management. Thyroid. 2014; 24:951–957.
Article9. Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998; 17:2815–2834.
Article10. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560.
Article11. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634.
Article12. Higgins JP, Altman DG, Gøtzsche PC, Jøni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928.
Article13. Ganly I, Ibrahimpasic T, Rivera M, Nixon I, Palmer F, Patel SG, et al. Prognostic implications of papillary thyroid carcinoma with tall-cell features. Thyroid. 2014; 24:662–670.
Article14. Lee CW, Roh JL, Gong G, Cho KJ, Choi SH, Nam SY, et al. Risk factors for recurrence of papillary thyroid carcinoma with clinically node-positive lateral neck. Ann Surg Oncol. 2015; 22:117–124.
Article15. Moritani S. Impact of invasive extranodal extension on the prognosis of patients with papillary thyroid carcinoma. Thyroid. 2014; 24:1779–1783.
Article16. Ryu IS, Song CI, Choi SH, Roh JL, Nam SY, Kim SY. Lymph node ratio of the central compartment is a significant predictor for locoregional recurrence after prophylactic central neck dissection in patients with thyroid papillary carcinoma. Ann Surg Oncol. 2014; 21:277–283.
Article17. Wang LY, Palmer FL, Nixon IJ, Tuttle RM, Shah JP, Patel SG, et al. Lateral neck lymph node characteristics prognostic of outcome in patients with clinically evident N1b papillary thyroid cancer. Ann Surg Oncol. 2015; 22:3530–3536.
Article18. Wu MH, Shen WT, Gosnell J, Duh QY. Prognostic significance of extranodal extension of regional lymph node metastasis in papillary thyroid cancer. Head Neck. 2015; 37:1336–1343.
Article19. Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med. 1994; 97:418–428.
Article20. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19:1167–1214.
Article21. Noguchi S, Noguchi A, Murakami N. Papillary carcinoma of the thyroid. I. Developing pattern of metastasis. Cancer. 1970; 26:1053–1060.
Article22. Wang LY, Palmer FL, Nixon IJ, Thomas D, Shah JP, Patel SG, et al. Central lymph node characteristics predictive of outcome in patients with differentiated thyroid cancer. Thyroid. 2014; 24:1790–1795.
Article23. Ito Y, Fukushima M, Tomoda C, Inoue H, Kihara M, Higashiyama T, et al. Prognosis of patients with papillary thyroid carcinoma having clinically apparent metastasis to the lateral compartment. Endocr J. 2009; 56:759–766.
Article24. Ricarte-Filho J, Ganly I, Rivera M, Katabi N, Fu W, Shaha A, et al. Papillary thyroid carcinomas with cervical lymph node metastases can be stratified into clinically relevant prognostic categories using oncogenic BRAF, the number of nodal metastases, and extra-nodal extension. Thyroid. 2012; 22:575–584.
Article25. Pak K, Suh S, Kim SJ, Kim IJ. Prognostic value of genetic mutations in thyroid cancer: a meta-analysis. Thyroid. 2015; 25:63–70.
Article26. Lee YS, Lim YS, Lee JC, Wang SG, Kim IJ, Son SM, et al. Nodal status of central lymph nodes as a negative prognostic factor for papillary thyroid carcinoma. J Surg Oncol. 2013; 107:777–782.
Article27. Ito Y, Miyauchi A. Lateral and mediastinal lymph node dissection in differentiated thyroid carcinoma: indications, benefits, and risks. World J Surg. 2007; 31:905–915.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- N Stage: Controversies and Recent Issues
- Significance of Lymphovascular Invasion as a Prognostic Factor in Patients with Papillary Thyroid Cancer: a Systematic Review and Meta-Analysis
- Alcohol Intake and Risk of Thyroid Cancer: A Meta-Analysis of Observational Studies
- Updated guidelines on the preoperative staging of thyroid cancer
- Surgical Management of Difficult Cases with Thyroid Cancer