Clin Endosc.
2013 Jul;46(4):373-378.
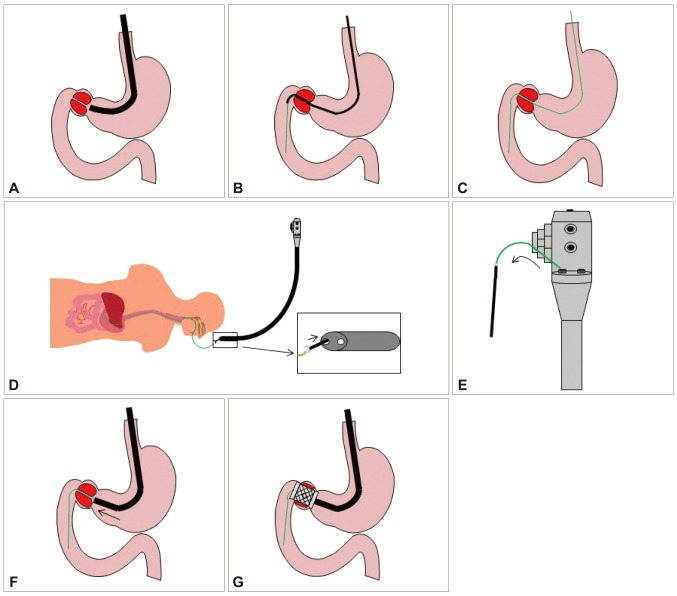
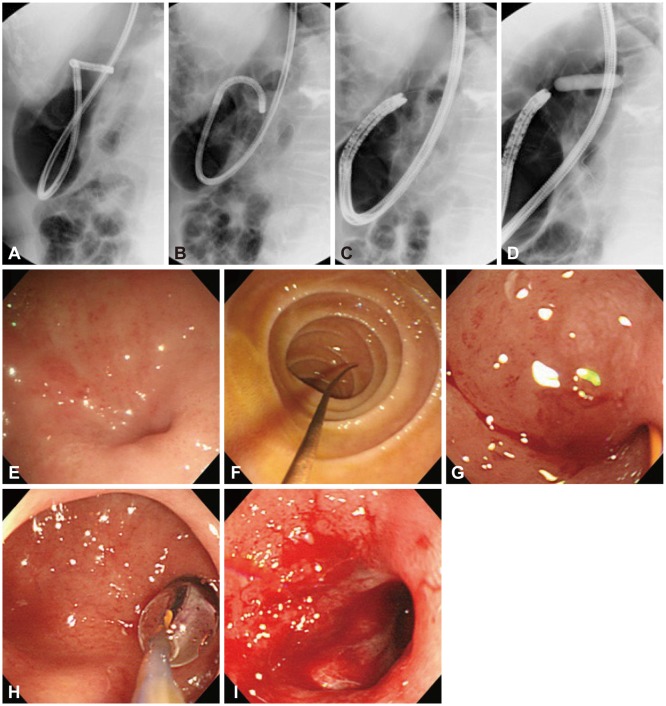
Ultrathin Endoscope-Assisted Method for the Management of Upper Gastrointestinal Obstruction to Avoid Technical Failure
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea. gastro@catholic.ac.kr
Abstract
- BACKGROUND/AIMS
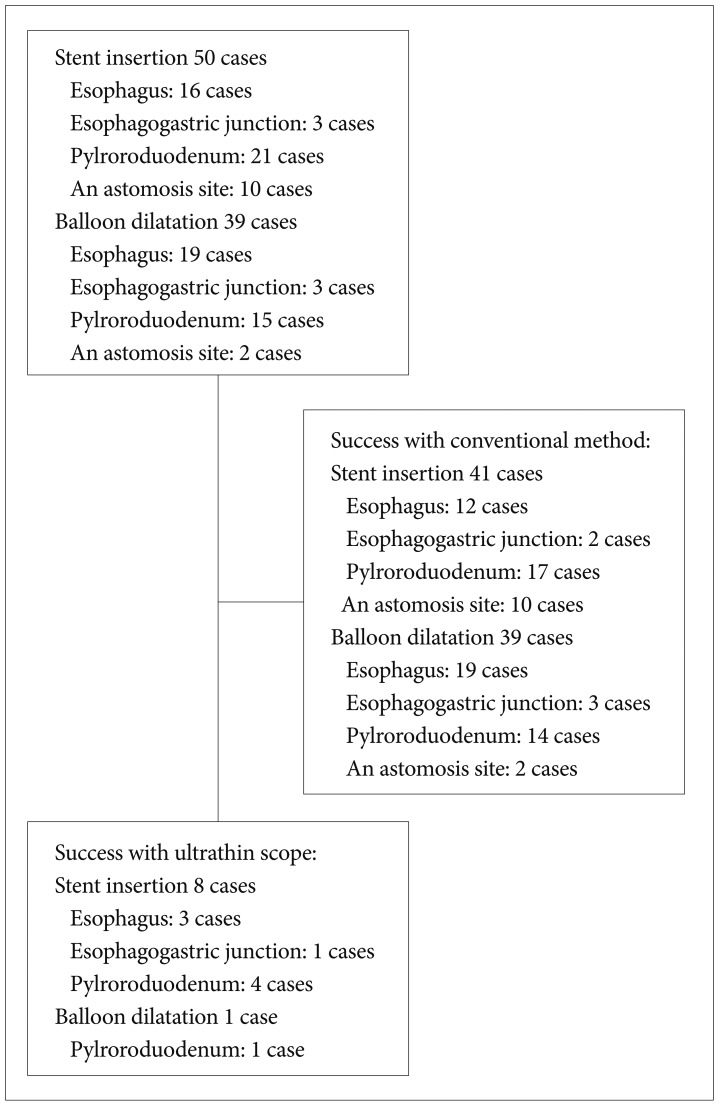
Endoscopic management of upper gastrointestinal obstruction is safe and feasible. However, its technical and clinical success rate is about 90%, which is primarily due to inability to pass a guide-wire through the stricture. The aim of this study was to evaluate the usefulness of an ultrathin endoscope for correct placement of guide wire to avoid technical failure in upper gastrointestinal obstruction.
METHODS
Retrospective assessment of ultrathin endoscope to traverse the stenosis of the upper gastrointestinal tract in technically difficult cases was performed. Technical and clinical success rates and immediate complications were analyzed.
RESULTS
Nine cases were included in this study (eight cases of stent insertion and one case of balloon dilatation). Technical success was achieved in all of the patients (100%) and oral feeding was feasible in all of the cases (100%). Immediate complications, such as migration, perforation, and hemorrhage, did not develop in any of the cases.
CONCLUSIONS
Ultrathin endoscope-assisted method for upper gastrointestinal obstruction is potentially safe and useful to avoid technical failure.
MeSH Terms
Figure
Reference
-
1. Dormann A, Meisner S, Verin N, Wenk Lang A. Self-expanding metal stents for gastroduodenal malignancies: systematic review of their clinical effectiveness. Endoscopy. 2004; 36:543–550. PMID: 15202052.
Article2. Dumortier J, Ponchon T, Scoazec JY, et al. Prospective evaluation of transnasal esophagogastroduodenoscopy: feasibility and study on performance and tolerance. Gastrointest Endosc. 1999; 49(3 Pt 1):285–291. PMID: 10049409.
Article3. Lustberg AM, Darwin PE. A pilot study of transnasal percutaneous endoscopic gastrostomy. Am J Gastroenterol. 2002; 97:1273–1274. PMID: 12014751.
Article4. García-Cano J. Use of an ultrathin gastroscope to allow endoscopic insertion of enteral wallstents without fluoroscopic monitoring. Dig Dis Sci. 2006; 51:1231–1235. PMID: 16944017.
Article5. Vlavianos P, Zabron A. Clinical outcomes, quality of life, advantages and disadvantages of metal stent placement in the upper gastrointestinal tract. Curr Opin Support Palliat Care. 2012; 6:27–32. PMID: 22228029.
Article6. Cennamo V, Fuccio L, Laterza L, et al. Side-viewing endoscope for colonic self-expandable metal stenting in patients with malignant colonic obstruction. Eur J Gastroenterol Hepatol. 2009; 21:585–586. PMID: 19282771.
Article7. Vázquez-Iglesias JL, Gonzalez-Conde B, Vázquez-Millán MA, Estévez-Prieto E, Alonso-Aguirre P. Self-expandable stents in malignant colonic obstruction: insertion assisted with a sphincterotome in technically difficult cases. Gastrointest Endosc. 2005; 62:436–437. PMID: 16111965.
Article8. Mulcahy HE, Fairclough PD. Ultrathin endoscopy in the assessment and treatment of upper and lower gastrointestinal tract strictures. Gastrointest Endosc. 1998; 48:618–620. PMID: 9852453.
Article9. Itoi T, Ishii K, Sofuni A, et al. Ultrathin endoscope-assisted ERCP for inaccessible peridiverticular papilla by a single-balloon enteroscope in a patient with Roux-en-Y anastomosis. Dig Endosc. 2010; 22:334–336. PMID: 21175491.
Article10. Krishna SG, McElreath DP, Rego RF. Direct pancreatoscopy with an ultrathin forward-viewing endoscope in intraductal papillary mucinous neoplasm of the pancreas. Clin Gastroenterol Hepatol. 2009; 7:e75–e76. PMID: 19683071.
Article11. Yan SL, Chen CH, Yeh YH, Yueh SK. Successful biliary stenting and sphincterotomy using an ultrathin forward-viewing endoscope. Endoscopy. 2009; 41(Suppl 2):E59–E60. PMID: 19319781.
Article12. Aydinli M, Koruk I, Dag MS, Savas MC, Kadayifci A. Ultrathin endoscopy for gastrointestinal strictures. Dig Endosc. 2012; 24:150–153. PMID: 22507087.
Article13. García-Cano J, González Martín JA, Redondo-Cerezo E, et al. Treatment of malignant colorectal obstruction by means of endoscopic insertion of self-expandable metallic stents. An Med Interna. 2003; 20:515–520. PMID: 14585037.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Placement of a Self-Expanding Metal Stent to Treat Esophagogastric Benign Anastomotic Stricture via Retroflexed Ultrathin Endoscopy: A Case Report with a Video
- Endoscope-Assisted Hairline Approach for Head and Neck Masses: A Review
- Real-Time Video-Assisted Retrieval of Airway Foreign Body in Very Young Pediatric Patients
- Clinical Practice Guidelines for Endoscope Reprocessing
- Palliation of Malignant Upper Gastrointestinal Obstruction with Self-Expandable Metal Stent