Clin Exp Otorhinolaryngol.
2023 Nov;16(4):317-325. 10.21053/ceo.2022.01634.
Endoscope-Assisted Hairline Approach for Head and Neck Masses: A Review
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Dankook University College of Medicine, Cheonan, Korea
- KMID: 2548360
- DOI: http://doi.org/10.21053/ceo.2022.01634
Abstract
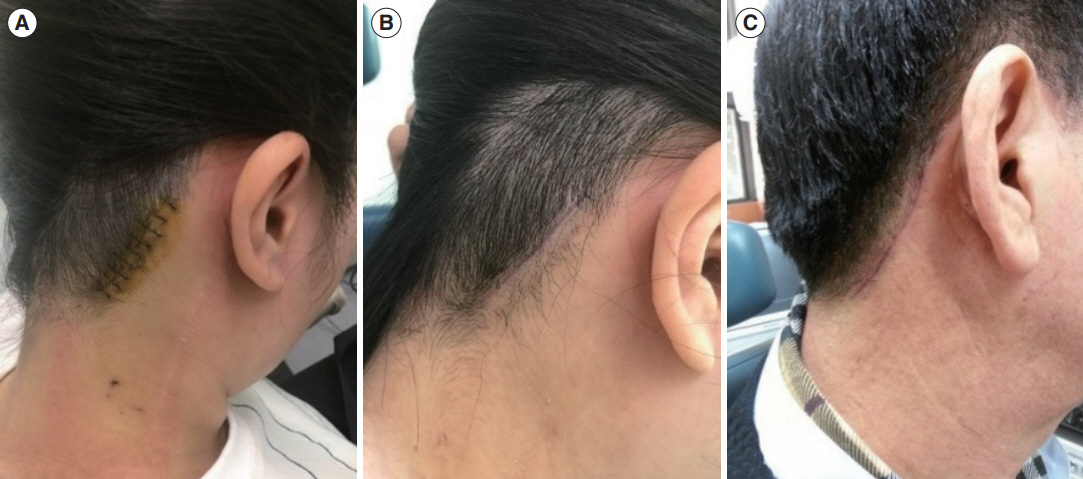
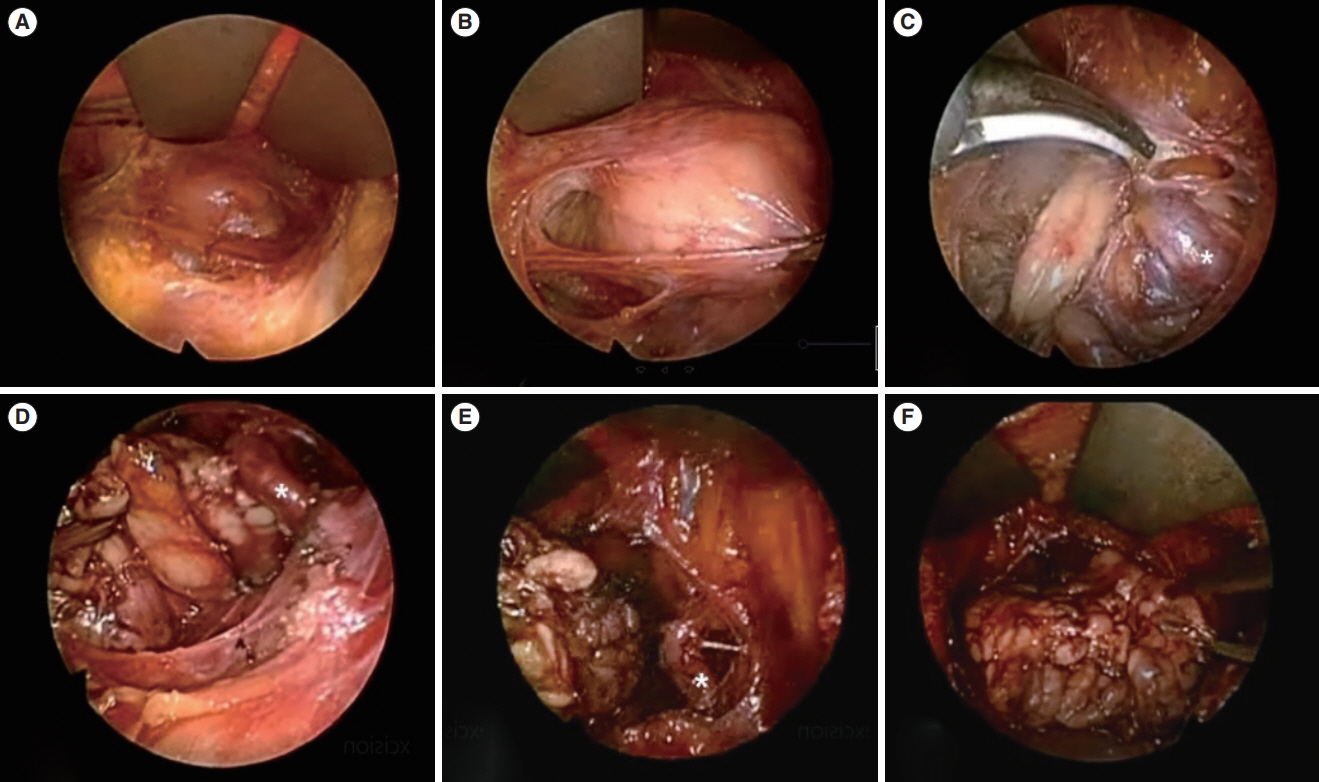
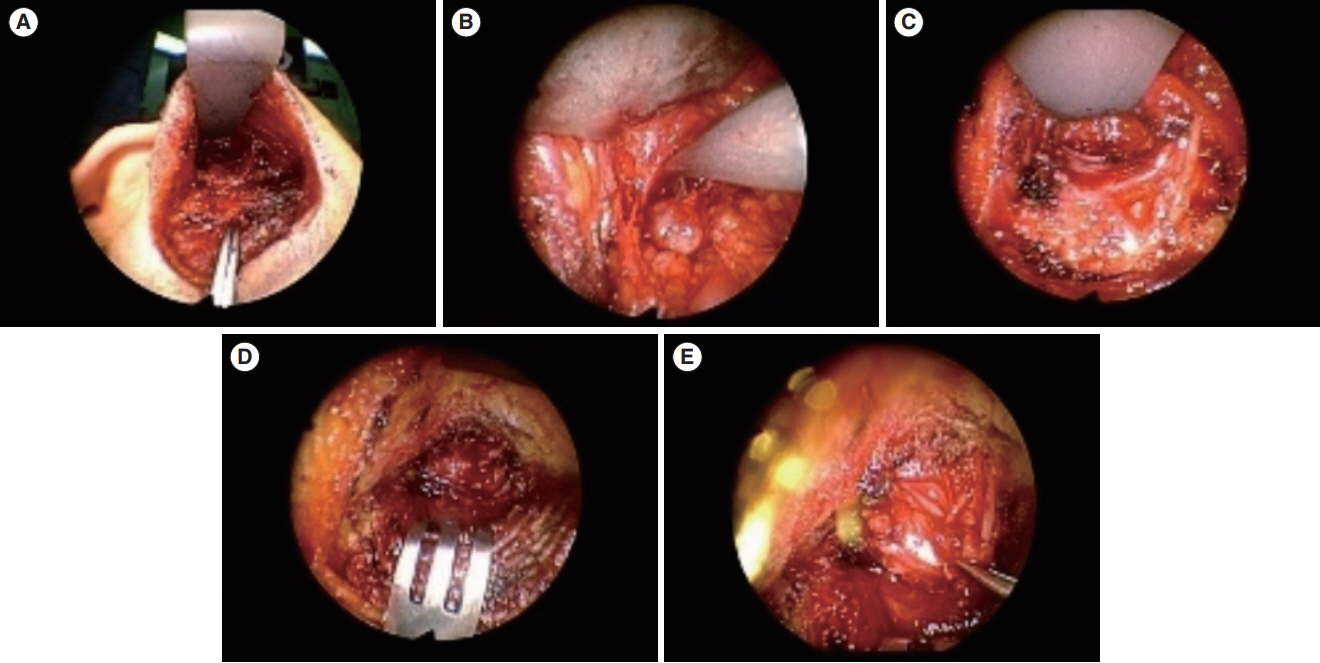
- Conventional surgery through a transcervical incision is indicated for the treatment of certain tumors in the head and neck. However, this method can cause multiple problems, including scarring and cosmetic concerns. The endoscope-assisted hairline approach, which serves as an alternative to conventional surgical procedures, is gaining popularity due to its excellent cosmetic and functional outcomes. However, given the anatomical complexity involved, the endoscope-assisted hairline technique is not frequently employed in head and neck surgery. The evolution of the hairline surgical approach has been influenced by changes in disease conditions and recent advances in surgical tools. This review article discusses the use of endoscope-assisted hairline approaches in the resection of head and neck masses, focusing on the surgical procedure and postoperative clinical outcomes.
Keyword
Figure
Reference
-
1. Rumsey N, Clarke A, White P. Exploring the psychosocial concerns of outpatients with disfiguring conditions. J Wound Care. 2003; Jul. 12(7):247–52.2. Lee HS, Lee D, Koo YC, Shin HA, Koh YW, Choi EC. Endoscopic resection of upper neck masses via retroauricular approach is feasible with excellent cosmetic outcomes. J Oral Maxillofac Surg. 2013; Mar. 71(3):520–7.3. Kim J, Lee YI, Lee JH, Oh SH, Lee SE, Kim YK. Successful treatment of post-operative keloid with combined cryotherapy and ablative fractional CO2 laser. Med Laser. 2020; Jun. 9(1):58–61.4. Gagner M, Inabnet WB. Endoscopic thyroidectomy for solitary thyroid nodules. Thyroid. 2001; Feb. 11(2):161–3.5. Ikeda Y, Takami H, Sasaki Y, Kan S, Niimi M. Endoscopic neck surgery by the axillary approach. J Am Coll Surg. 2000; Sep. 191(3):336–40.6. Ikeda Y, Takami H, Sasaki Y, Takayama J, Niimi M, Kan S. Comparative study of thyroidectomies: endoscopic surgery versus conventional open surgery. Surg Endosc. 2002; Dec. 16(12):1741–5.7. Gagner M. Endoscopic subtotal parathyroidectomy in patients with primary hyperparathyroidism. Br J Surg. 1996; Jun. 83(6):875.8. Choi WJ, Park ES, Tak MS, Kang SG. Combination treatment of Nd: YAG picosecond-domain laser and fractional CO2 laser for contracted neck scar with hyperpigmentation. Med Lasers. 2021; Feb. 10(1):52–4.9. Kim YH, Kim BK. Scar treatment using 585-nam pulsed dye laser. Med Lasers. 2016; Jun. 5(1):17–21.10. Miccoli P, Bendinelli C, Berti P, Vignali E, Pinchera A, Marcocci C. Video-assisted versus conventional parathyroidectomy in primary hyperparathyroidism: a prospective randomized study. Surgery. 1999; Dec. 126(6):1117–21.11. Ohgami M, Ishii S, Arisawa Y, Ohmori T, Noga K, Furukawa T, et al. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech. 2000; Feb. 10(1):1–4.12. Park KN, Cho SH, Lee SW. Nationwide multicenter survey for current status of endoscopic thyroidectomy in Korea. Clin Exp Otorhinolaryngol. 2015; Jun. 8(2):149–54.13. Woo SH, Park JJ, Kwon M, Kim JP. “Hidden scar” submandibular gland excision using an endoscope-assisted hairline approach. Oral Oncol. 2017; Feb. 65:83–8.14. Woo SH. Endoscope-assisted intraoral removal of the thyroid isthmus mass using a frenotomy incision. J Laparoendosc Adv Surg Tech A. 2013; Sep. 23(9):787–90.15. Woo SH. Endoscopic-assisted total thyroidectomy via lateral keloid scar incision. Clin Exp Otorhinolaryngol. 2014; Dec. 7(4):338–41.16. Woo SH, Jeong HS, Kim JP, Park JJ, Baek CH. Endoscope-assisted intraoral removal of ectopic thyroid tissue using a frenotomy incision. Thyroid. 2013; May. 23(5):605–8.17. Woo SH, Kim JP, Baek CH. Endoscope-assisted extracapsular dissection of benign parotid tumors using hairline incision. Head Neck. 2016; Mar. 38(3):375–9.18. Kim JP, Park JJ, Woo SH. Endoscope-assisted hairline approach for resecting maxillofacial masses. Int J Oral Maxillofac Surg. 2020; Mar. 49(3):310–6.19. Tae K, Ji YB, Song CM, Ryu J. Robotic and endoscopic thyroid surgery: evolution and advances. Clin Exp Otorhinolaryngol. 2019; Feb. 12(1):1–11.20. Eneroth CM. Salivary gland tumors in the parotid gland, submandibular gland, and the palate region. Cancer. 1971; Jun. 27(6):1415–8.21. Aro K, Tarkkanen J, Saat R, Saarilahti K, Makitie A, Atula T. Submandibular gland cancer: specific features and treatment considerations. Head Neck. 2018; Jan. 40(1):154–62.22. Weber RS, Byers RM, Petit B, Wolf P, Ang K, Luna M. Submandibular gland tumors. Adverse histologic factors and therapeutic implications. Arch Otolaryngol Head Neck Surg. 1990; Sep. 116(9):1055–60.23. Preuss SF, Klussmann JP, Wittekindt C, Drebber U, Beutner D, Guntinas-Lichius O. Submandibular gland excision: 15 years of experience. J Oral Maxillofac Surg. 2007; May. 65(5):953–7.24. Singer DP, Sullivan PK. Submandibular gland I: an anatomic evaluation and surgical approach to submandibular gland resection for facial rejuvenation. Plast Reconstr Surg. 2003; Sep. 112(4):1150–4.25. Laskawi R, Ellies M, Arglebe C, Schott A. Surgical management of benign tumors of the submandibular gland: a follow-up study. J Oral Maxillofac Surg. 1995; May. 53(5):506–8.26. Conley J, Myers E, Cole R. Analysis of 115 patients with tumors of the submandibular gland. Ann Otol Rhinol Laryngol. 1972; Jun. 81(3):323–30.27. Munir N, Bradley PJ. Diagnosis and management of neoplastic lesions of the submandibular triangle. Oral Oncol. 2008; Mar. 44(3):251–60.28. Chen MK, Su CC, Tsai YL, Chang CC. Minimally invasive endoscopic resection of the submandibular gland: a new approach. Head Neck. 2006; Nov. 28(11):1014–7.29. Roh JL. Removal of the submandibular gland by a retroauricular approach. Arch Otolaryngol Head Neck Surg. 2006; Jul. 132(7):783–7.30. Quer M, Vander Poorten V, Takes RP, Silver CE, Boedeker CC, de Bree R, et al. Surgical options in benign parotid tumors: a proposal for classification. Eur Arch Otorhinolaryngol. 2017; Nov. 274(11):3825–36.31. Eveson JW, Cawson RA. Salivary gland tumours: a review of 2410 cases with particular reference to histological types, site, age and sex distribution. J Pathol. 1985; May. 146(1):51–8.32. Albergotti WG, Nguyen SA, Zenk J, Gillespie MB. Extracapsular dissection for benign parotid tumors: a meta-analysis. Laryngoscope. 2012; Sep. 122(9):1954–60.33. O’Brien CJ. Current management of benign parotid tumors: the role of limited superficial parotidectomy. Head Neck. 2003; Nov. 25(11):946–52.34. Zhi K, Ren W, Gao L, Zhao L, Huang S, Li J, et al. Face-lift incision combined with sternomastoid muscular flap in parotidectomy. Aesthetic Plast Surg. 2011; Aug. 35(4):558–62.35. Roh JL. Extracapsular dissection of benign parotid tumors using a retroauricular hairline incision approach. Am J Surg. 2009; May. 197(5):e53–6.36. Lin SD, Tsai CC, Lai CS, Lee SS, Chang KP. Endoscope-assisted parotidectomy for benign parotid tumors. Ann Plast Surg. 2000; Sep. 45(3):269–73.37. Li Y, Xue R, Lai Q, Xu B, Yuan K, Tang X, et al. Endoscope-assisted resection of nonneoplastic space-occupying lesion in oral and maxillofacial areas. Sci Rep. 2017; Dec. 7(1):16920.38. Zhong LP, Zhao SF, Chen GF, Ping FY. Ultrasonographic appearance of lipoma in the oral and maxillofacial region. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; Dec. 98(6):738–40.39. Miyakubo M, Oriuchi N, Tsushima Y, Higuchi T, Koyama K, Arai K, et al. Diagnosis of maxillofacial tumor with L-3-[18f]-fluoro-alpha-methyltyrosine (FMT) PET: a comparative study with FDG-PET. Ann Nucl Med. 2007; Feb. 21(2):129–35.40. Glosser JW, Pires CA, Feinberg SE. Branchial cleft or cervical lymphoepithelial cysts: etiology and management. J Am Dent Assoc. 2003; Jan. 134(1):81–6.41. Tanaka N, Murata A, Yamaguchi A, Kohama G. Clinical features and management of oral and maxillofacial tumors in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; Jul. 88(1):11–5.42. Mitroi M, Dumitrescu D, Simionescu C, Popescu C, Mogoanta C, Cioroianu L, et al. Management of second branchial cleft anomalies. Rom J Morphol Embryol. 2008; 49(1):69–74.43. Ahn Y, Lee SH. Laser-assisted transforaminal endoscopic lumbar discectomy: technical pearls for prevention of complications. Med Lasers. 2013; Dec. 2(2):43–8.44. Padalhin AR. Lasers and robots: recent developments in transoral laser and transoral robotic surgery. Med Lasers. 2020; Dec. 9(2):103–9.45. Song CM, Jung YH, Sung MW, Kim KH. Endoscopic resection of the submandibular gland via a hairline incision: a new surgical approach. Laryngoscope. 2010; May. 120(5):970–4.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopically-Assisted Scar-Free Midline Neck Mass Excision
- Hairline lowering surgery: how we do it
- Endoscope-Assisted Trichophytic Anterior Hairline Brow Lift
- Transoral Endoscopic Diverticulostomy of Zenker’s Diverticulum With Energy Device
- Book Review: Multidisciplinary Head & Neck Reconstruction. A Defect-Oriented Approach