Cancer Res Treat.
2018 Oct;50(4):1452-1457. 10.4143/crt.2017.414.
Microcystic Stromal Tumor of Testicle: First Case Report and Literature Review
- Affiliations
-
- 1Institute of Pathology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China. 763626334@qq.com, aoqilin@263.net
- 2Department of Pathology, School of Basic Medical Science, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China.
- KMID: 2424815
- DOI: http://doi.org/10.4143/crt.2017.414
Abstract
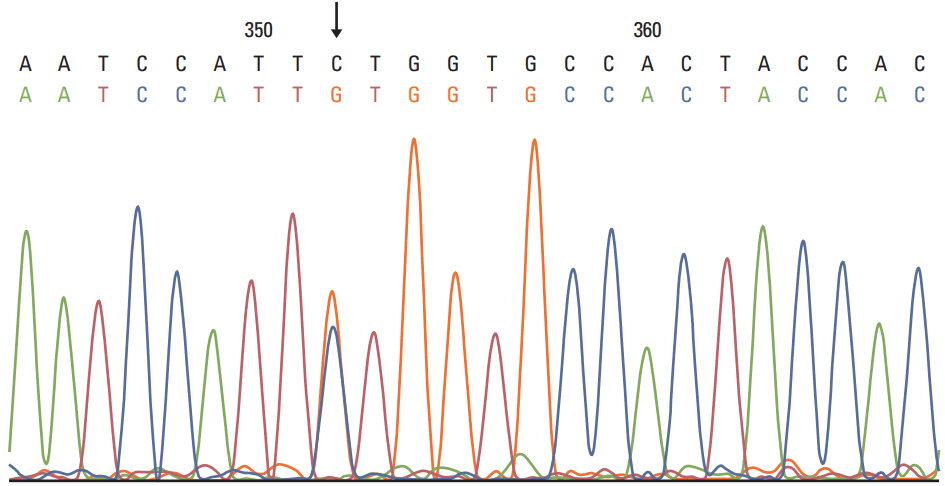
- Microcystic stromal tumor (MCST) is a rare subtype of sex cord-stromal neoplasm. Tumors from all 31 previously reported cases were located in the ovary. Herein, we present a unique case of a right-side testicular tumor in a 33-year-old Chinese male. The tumor is composed of predominantly lobulated cellular nodules separated by hyalinized fibrous stroma and they expressed CD10, β-catenin (nuclear), and cyclin D1. Molecular analysis identified a point mutation (c.110C>G) in exon 3 of CTNNB1. The histopathological features, immunohistochemistry profiles, and molecular analysis of this tumor were consistent with MCST of the ovary. Therefore, a diagnosis of MCST of the right testicle was determined. To the best of our knowledge, this is the first case of MCST occurring in the testicles. The study may provide new insights to the tumor biology of MCST and a better understanding of this rare entity.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Irving JA, Young RH. Microcystic stromal tumor of the ovary: report of 16 cases of a hitherto uncharacterized distinctive ovarian neoplasm. Am J Surg Pathol. 2009; 33:367–75.2. Irving JA, Lee CH, Yip S, Oliva E, McCluggage WG, Young RH. Microcystic stromal tumor: a distinctive ovarian sex cordstromal neoplasm characterized by FOXL2, SF-1, WT-1, cyclin D1, and beta-catenin nuclear expression and CTNNB1 mutations. Am J Surg Pathol. 2015; 39:1420–6.3. Moch H, Cubilla AL, Humphrey PA, Reuter VE, Ulbright TM. The 2016 WHO classification of tumours of the urinary system and male genital organs: part A: renal, penile, and testicular tumours. Eur Urol. 2016; 70:93–105.4. Young RH. Sex cord-stromal tumors of the ovary and testis: their similarities and differences with consideration of selected problems. Mod Pathol. 2005; 18 Suppl 2:S81–98.
Article5. Horta M, Cunha TM. Sex cord-stromal tumors of the ovary: a comprehensive review and update for radiologists. Diagn Interv Radiol. 2015; 21:277–86.
Article6. Roth LM, Cheng L. Mixed germ cell-sex cord stromal tumor of the testis with an intratubular component: a problem in differential diagnosis. Hum Pathol. 2016; 51:51–6.
Article7. Yang M, Bhattacharjee MB. Ovarian microcystic stromal tumor: report of a new entity with immunohistochemical and ultrastructural studies. Ultrastruct Pathol. 2014; 38:261–7.
Article8. Lee SH, Koh YW, Roh HJ, Cha HJ, Kwon YS. Ovarian microcystic stromal tumor: a novel extracolonic tumor in familial adenomatous polyposis. Genes Chromosomes Cancer. 2015; 54:353–60.
Article9. Kang YN, Cho CH, Kwon SY. Microcystic stromal tumor of the ovary with mutation in exon 3 of beta-catenin: a case report. Int J Gynecol Pathol. 2015; 34:121–5.10. Gunes P, Kir G, Yilmaz I, Kucukodaci Z. Coexistence of microcystic stromal tumor of the ovary with mutation of betacatenin and contralateral mucinous cystadenoma. Int J Gynecol Pathol. 2015; 34:546–50.11. Lee JH, Kim HS, Cho NH, Lee JY, Kim S, Kim SW, et al. Genetic analysis of ovarian microcystic stromal tumor. Obstet Gynecol Sci. 2016; 59:157–62.
Article12. Maeda D, Shibahara J, Sakuma T, Isobe M, Teshima S, Mori M, et al. beta-catenin (CTNNB1) S33C mutation in ovarian microcystic stromal tumors. Am J Surg Pathol. 2011; 35:1429–40.13. Liu C, Gallagher RL, Price GR, Bolton E, Joy C, Harraway J, et al. Ovarian microcystic stromal tumor: a rare clinical manifestation of familial adenomatous polyposis. Int J Gynecol Pathol. 2016; 35:561–5.14. Meurgey A, Descotes F, Mery-Lamarche E, Devouassoux-Shisheboran M. Lack of mutation of DICER1 and FOXL2 genes in microcystic stromal tumor of the ovary. Virchows Arch. 2017; 470:225–9.
Article15. Gupta S, Erickson LA. Paratesticular adenomatoid tumor. Mayo Clin Proc. 2016; 91:e167–8.
Article