Brain Tumor Res Treat.
2018 Oct;6(2):92-96. 10.14791/btrt.2018.6.e16.
Brain Abscess Showing a Lack of Restricted Diffusion and Successfully Treated with Linezolid
- Affiliations
-
- 1Department of Neurosurgery, Eulji University, Nowon Eulji Medical Center, Seoul, Korea. drkdr@hanmail.net
- KMID: 2423981
- DOI: http://doi.org/10.14791/btrt.2018.6.e16
Abstract
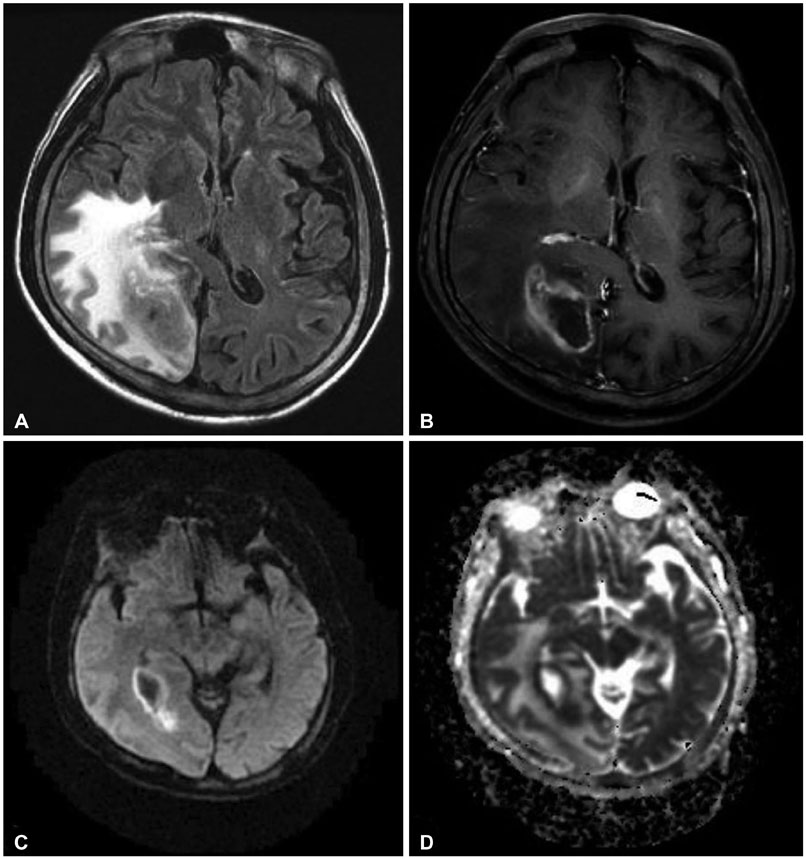
- A 59-year-old patient with a history of hepatocellular carcinoma presented with decreased consciousness and left hemiparesis. A rim-enhanced mass lesion without diffusion restriction was observed in contrast-enhanced MRI including diffusion-weighted imaging. Based on these findings, metastatic brain tumor was suspected. However, brain abscess (BA) was diagnosed after multiple bacterial colonies were observed in aspiration biopsy. Initial conventional antibiotic treatment including vancomycin had failed, so linezolid was used as second-line therapy. As a result, infection signs and clinical symptoms were resolved. We report a case with atypical imaging features and antibiotic susceptibility of a BA in an immunocompromised patient undergoing chemotherapy.
MeSH Terms
Figure
Reference
-
1. Brouwer MC, Tunkel AR, van de Beek D. Brain abscess. N Engl J Med. 2014; 371:1758.
Article2. Nathoo N, Nadvi SS, Narotam PK, van Dellen JR. Brain abscess: management and outcome analysis of a computed tomography era experience with 973 patients. World Neurosurg. 2011; 75:716–726. discussion 612-7.
Article3. Britt RH, Enzmann DR, Yeager AS. Neuropathological and computerized tomographic findings in experimental brain abscess. J Neurosurg. 1981; 55:590–603.
Article4. Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess: systematic review and meta-analysis. Neurology. 2014; 82:806–813.
Article5. Xu XX, Li B, Yang HF, et al. Can diffusion-weighted imaging be used to differentiate brain abscess from other ring-enhancing brain lesions? A meta-analysis. Clin Radiol. 2014; 69:909–915.
Article6. Birmingham MC, Rayner CR, Meagher AK, Flavin SM, Batts DH, Schentag JJ. Linezolid for the treatment of multidrug-resistant, grampositive infections: experience from a compassionate-use program. Clin Infect Dis. 2003; 36:159–168.
Article7. Helweg-Larsen J, Astradsson A, Richhall H, Erdal J, Laursen A, Brennum J. Pyogenic brain abscess, a 15 year survey. BMC Infect Dis. 2012; 12:332.
Article8. Muzumdar D, Jhawar S, Goel A. Brain abscess: an overview. Int J Surg. 2011; 9:136–144.
Article9. Xiao F, Tseng MY, Teng LJ, Tseng HM, Tsai JC. Brain abscess: clinical experience and analysis of prognostic factors. Surg Neurol. 2005; 63:442–449. discussion 449-50.
Article10. Erdoğan E, Cansever T. Pyogenic brain abscess. Neurosurg Focus. 2008; 24:E2.
Article11. Goodkin HP, Harper MB, Pomeroy SL. Intracerebral abscess in children: historical trends at Children's Hospital Boston. Pediatrics. 2004; 113:1765–1770.
Article12. Yuh WT, Nguyen HD, Gao F, et al. Brain parenchymal infection in bone marrow transplantation patients: CT and MR findings. AJR Am J Roentgenol. 1994; 162:425–430.
Article13. Ozbayrak M, Ulus OS, Berkman MZ, Kocagoz S, Karaarslan E. Atypical pyogenic brain abscess evaluation by diffusion-weighted imaging: diagnosis with multimodality MR imaging. Jpn J Radiol. 2015; 33:668–671.
Article14. Reddy JS, Mishra AM, Behari S, et al. The role of diffusion-weighted imaging in the differential diagnosis of intracranial cystic mass lesions: a report of 147 lesions. Surg Neurol. 2006; 66:246–250. discussion 250-1.
Article15. Nath K, Agarwal M, Ramola M, et al. Role of diffusion tensor imaging metrics and in vivo proton magnetic resonance spectroscopy in the differential diagnosis of cystic intracranial mass lesions. Magn Reson Imaging. 2009; 27:198–206.
Article16. Toh CH, Wei KC, Chang CN, et al. Differentiation of pyogenic brain abscesses from necrotic glioblastomas with use of susceptibility-weighted imaging. AJNR Am J Neuroradiol. 2012; 33:1534–1538.
Article17. Pal D, Bhattacharyya A, Husain M, Prasad KN, Pandey CM, Gupta RK. In vivo proton MR spectroscopy evaluation of pyogenic brain abscesses: a report of 194 cases. AJNR Am J Neuroradiol. 2010; 31:360–366.
Article18. Livermore DM. Linezolid in vitro: mechanism and antibacterial spectrum. J Antimicrob Chemother. 2003; 51:Suppl 2. ii9–ii16.
Article19. Vinh DC, Rubinstein E. Linezolid: a review of safety and tolerability. J Infect. 2009; 59:Suppl 1. S59–S74.
Article20. French G. Safety and tolerability of linezolid. J Antimicrob Chemother. 2003; 51:Suppl 2. ii45–ii53.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bright Intracranial Lesions on Diffusion-weighted Images: A Pictorial Review
- Diffusion-weighted Imaging and Proton Magnetic Resonance Spectroscopy of Tuberculous Brain Abscess with a Fluid-fluid Level
- A Case of Multiloculated Infantile Brain Abscess Treated by Repeated Needle Aspiration
- Preoperative Assessment of Cystic Brain Lesion: Significance of Diffusion-Weighted Image and ADC (Apparent Diffusion Coefficiency) Values
- High-Altitude Cerebral Edema Evaluated with MRI: A Case Report