J Korean Soc Spine Surg.
2018 Sep;25(3):128-132. 10.4184/jkss.2018.25.3.128.
Diagnosis of C2 Spondylotic Radiculopathy by Physical Examination and Imaging Studies and Treatment by Microscopic Posterior Foraminotomy: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Bundang Jesaeng General Hospital, Seongnam, Korea. yslee2808@gmail.com
- KMID: 2421605
- DOI: http://doi.org/10.4184/jkss.2018.25.3.128
Abstract
- STUDY DESIGN: Case report.
OBJECTIVES
We report the case of a patient with C2 spondylotic radiculopathy who was treated by microscopic posterior foraminotomy. SUMMARY OF LITERATURE REVIEW: C2 spondylotic radiculopathy is rare, but it can occur due to spondylosis, compression by a venous plexus or vertebral artery, or hypertrophy of the atlantoepistrophic ligament.
MATERIALS AND METHODS
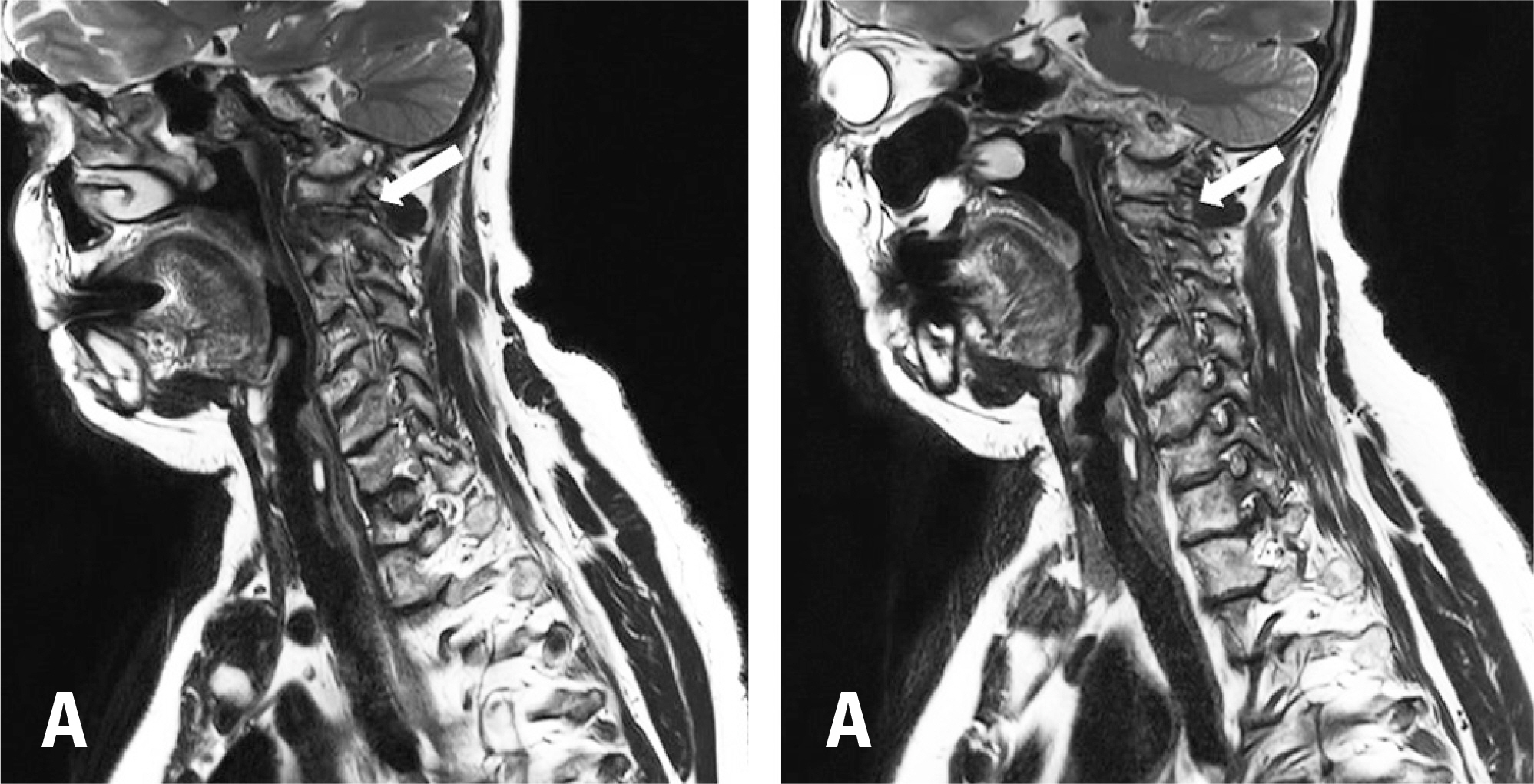
A 64-year-old woman was hospitalized with severe occipital pain radiating toward the left cervical area and posterior to the left ear. It started 3 years previously, and became aggravated 3 months previously. Foraminal stenosis of C1-2 was observed on magnetic resonance imaging (MRI) and degenerative changes of the facet joint of C1-2 and osteophytes originating from the left atlantoaxial joint were shown on computed tomography (CT). Dynamic rotational CT showed narrowing of the left C1-2 neural foramen when it was rotated to the left. Selective C2 root block was done, but the pain was aggravated. Thus, we decompressed the C2 nerve root by microscopic posterior laminotomy of the C1 vertebra. After surgery, the patient's occipitocervical pain mostly resolved. By the 6-month follow up, pain had not recurred, and instability was not observed on plain radiographs.
RESULTS
C2 Spondylotic radiculopathy was diagnosed by physical examination and imaging studies and it was treated by a surgical approach.
CONCLUSIONS
C2 spondylotic radiculopathy should be considered when a patient complains of occipitocervical pain triggered by cervical rotation and C1-2 foraminal stenosis is observed on MRI and CT.
Keyword
MeSH Terms
Figure
Reference
-
1. Spurling RG, Scoville WB. Lateral rupture of cervical intervertebral disc. A common cause of shoulder and arm pain. Surg Gynecol Obstet. 1944; 78:350–8.2. Ehni G, Benner B. Occipital neuralgia and the C1-2 arthrosis syndrome. J Neurosurg. 1984 Nov; 61(5):961–5. DOI: 10.3171/jns.1984.61.5.0961.
Article3. Star MJ, Curd JG, Thorne RP. Atlantoaxial lateral mass osteoarthritis. A frequently overlooked cause of severe occipitocervical pain. Spine (Phila Pa 1976). 1992 Jun; 17(6 Suppl):71–6.4. Clavel M, Clavel P. Occipital neuralgia secondary to exuberant callus formation. Case report. J Neurosurg. 1996 Dec; 85(6):1170–1. DOI: 10.3171/jns.1996.85.6.1170.5. Pakzaban P. Transarticular screw fixation of C1-2 for the treatment of arthropathy-associated occipital neuralgia. 2011 Feb; 14(2):209–14. DOI: 10.3171/2010.10. SPINE09815.6. Pikus HJ, Phillips JM. Outcome of surgical decompression of the second cervical root for cervicogenic headache. Neurosurgery. 1996 Jul; 39(1):63–70. discussion 70-1. DOI: 10.1097/00006123-199607000-00014.
Article7. Lu J, Ebraheim NA. Anatomic considerations of C2 nerve root ganglion. Spine (Phila Pa 1976). 1998 Mar; 23(6):64952. DOI: 10.1097/00007632-199803150-00001.
Article8. Cesmebasi A, Muhleman MA, Hulsberg P, et al. Occipital neuralgia: anatomic considerations. Clin Anat. 2015 Jan; 28(1):101–8. DOI: 10.1002/ca.22468.
Article9. Sjaastad O, Saunte C, Hovdahl H et al “Cervicogenic” headache. An hypothesis. Cephalalgia. 1983 Dec; 3(4):24956. DOI: 10.1046/j.1468-2982.1983.0304249.x.10. Kim CH, Kim K-T, Chung CK, et al. Minimally invasive cervical foraminotomy and diskectomy for laterally located soft disk herniation. Eur Spine J. 2015 Dec; 24(12):300512. DOI: 10.1007/s00586-015-4198-1.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Cervical Inclinatory Foraminotomy for Spondylotic Radiculopathy Preliminary
- Posterior Cervical Microscopic Foraminotomy and Discectomy with Laser for Unilateral Radiculopathy
- Early Surgical Results of Minimally Invasive Posterior Foraminotomy using Tubular Retractor for Cervical Radiculopathy
- Long-Term Outcome of Posterior Cervical Inclinatory Foraminotomy
- Endoscope Assisted Anterior Cervical Foraminotomy