J Korean Soc Spine Surg.
2007 Jun;14(2):67-72. 10.4184/jkss.2007.14.2.67.
Early Surgical Results of Minimally Invasive Posterior Foraminotomy using Tubular Retractor for Cervical Radiculopathy
- Affiliations
-
- 1Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University, School of Medicine, Seoul, Korea. neuriac@gmail.com
- KMID: 1941657
- DOI: http://doi.org/10.4184/jkss.2007.14.2.67
Abstract
-
STUDY DESIGN: A retrospective review of the clinical and surgical outcomes in 13 patients in which minimally invasive posterior cervical foraminotomy was performed.
OBJECTIVES
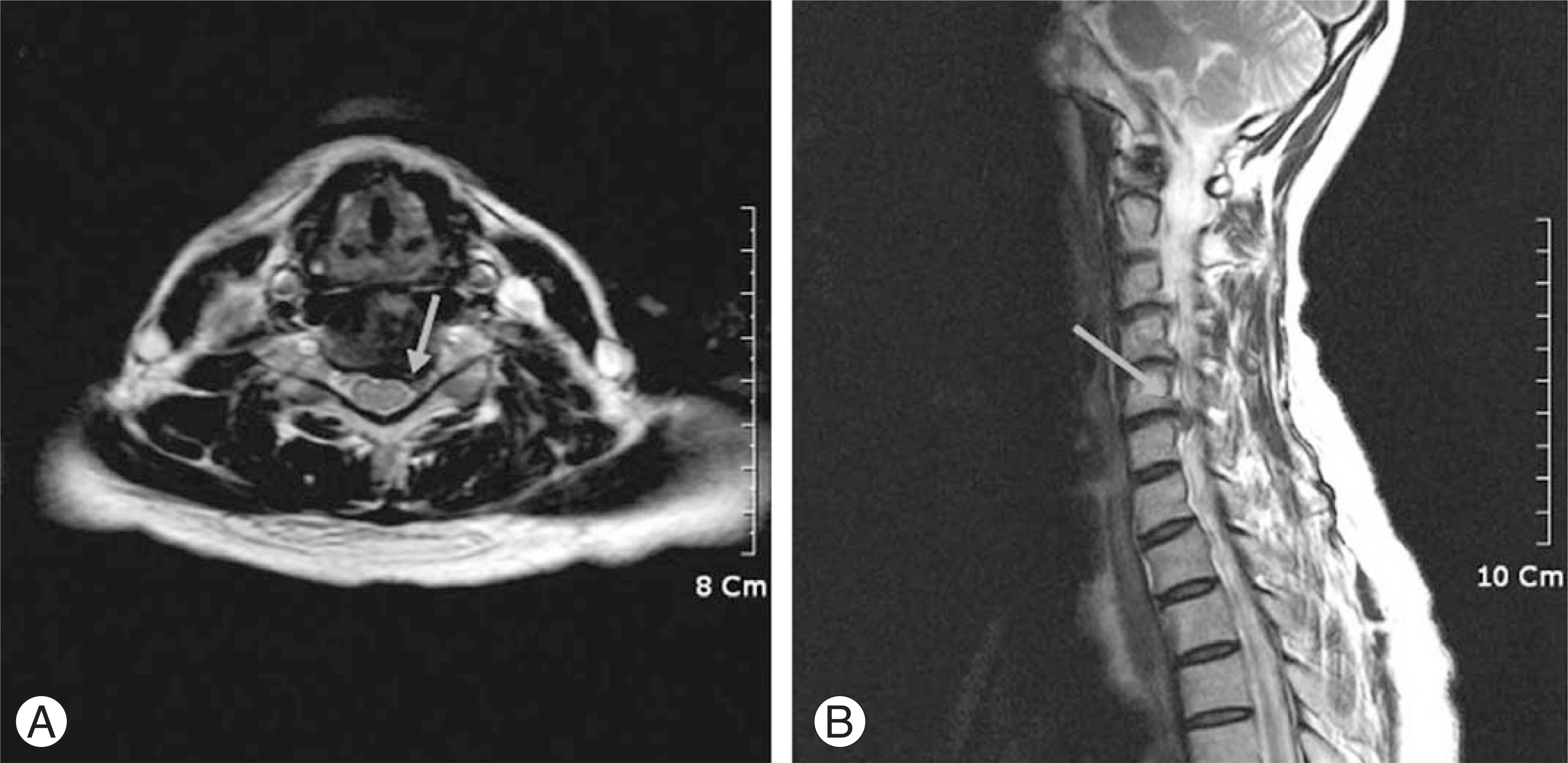
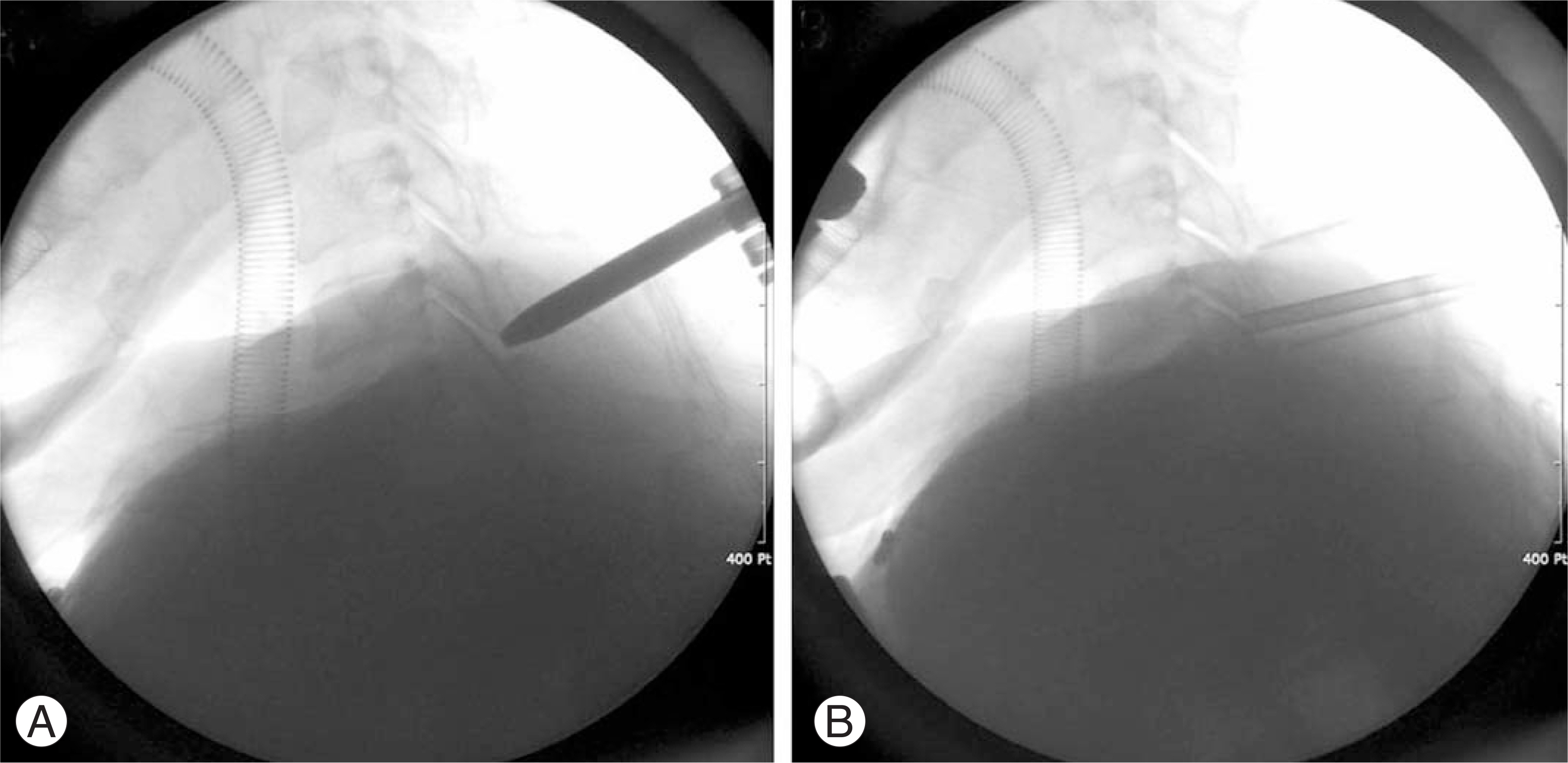
To report early surgical results of cervical posterior foraminotomy using a tubular retractor with minimally invasive deep muscle splitting. SUMMARY OF LITERTURE REVIEW: In previous studies of the posterior approach, good outcomes were established. The limitations of the posterior approach used to treat compression that was centrally located in the spinal canal were obvious, so the anterior approach was subsequently performed. Moreover, peri-incisional pain and discomfort related to the subperiosteal detachment of the muscle and ligament were the main limitations of this posterior approach. The use of the microendoscope allows very limited exposure with minimal tissue destruction, and has recently been used by various surgeons.
MATERIALS AND METHODS
Clinical results obtained in 13 patients who underwent posterior foraminotomy from Jan 2005 through Apr 2006 were assessed using a modified Prolo outcome scale. The posterior foraminotomy was performed in a minimally invasive fashion using a tubular retractor with muscle splitting dissection.
RESULTS
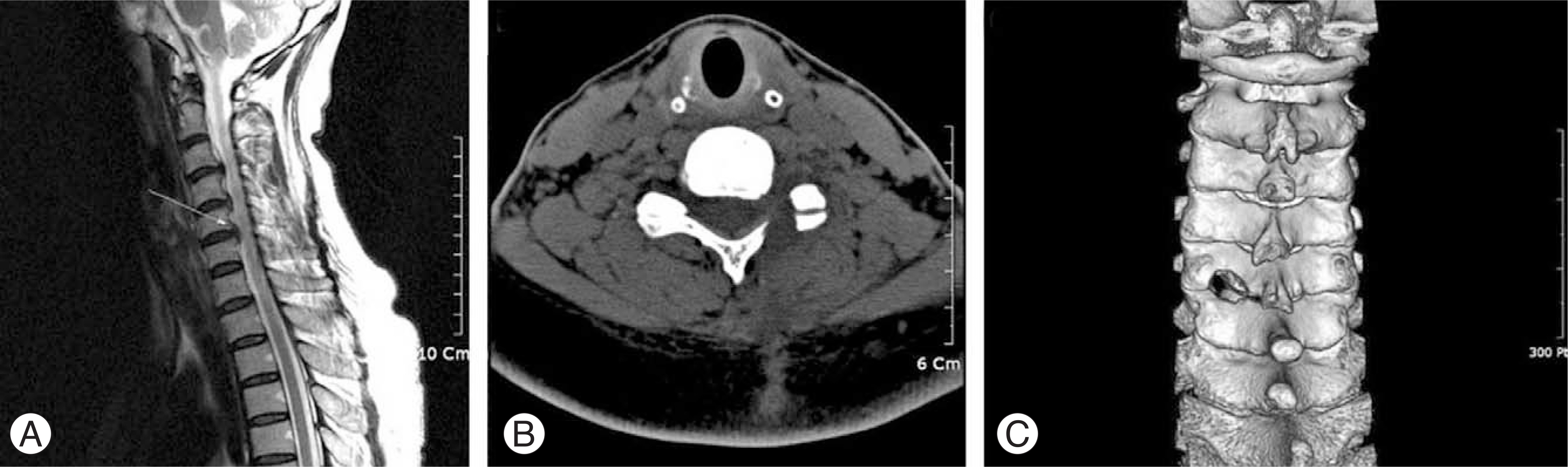
Eleven of 13 patients showed immediate relief of radiculopathy. Postoperative posterior cervical pain and spasm were negligible, and no surgically related complication was noted. During the follow-up period, 12 of 13 patients demonstrated a good outcome based on the modified Prolo outcome scale.
CONCLUSIONS
Posterior foraminotomy using a tubular retractor is a minimally invasive surgical option for treating cervical radiculopathy and alleviating post-incisional discomfort on the neck.
MeSH Terms
Figure
Cited by 1 articles
-
Long-Term Clinical and Radiologic Outcomes of Minimally Invasive Posterior Cervical Foraminotomy
Young-Joon Kwon
J Korean Neurosurg Soc. 2014;56(3):224-229. doi: 10.3340/jkns.2014.56.3.224.
Reference
-
1). Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958; 40:607–624.
Article2). Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958; 15:602–617.
Article3). DePalma AF, Rothman RH, Lewinnek GE, Canale ST. Anterior interbody fusion for severe cervical disc degeneration. Surg Gynecol Obstet. 1972; 134:755–758.4). Hilibrand AS, Yoo JU, Carlson GD, Bohlman HH. The success of anterior cervical arthrodesis adjacent to a previous fusion. Spine. 1997; 22:1574–1579.
Article5). Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997; 3:301–307.6). Adamson TE. Microendoscopic posterior cervical laminoforaminotomy for unilateral radiculopathy: results of a new technique in 100 cases. J Neurosurg. 2001; 95:51–57.
Article7). Fessler RG, Khoo LT. Minimally invasive cervical microendoscopic foraminotomy: an initial clinical experience. Neurosurgery. 2002; 51:37–45.
Article8). Ditunno JF Jr, Young W, Donovan WH, Creasey G. The international standards booklet for neurological and functional classification of spinal cord injury. American Spinal Injury Association. Paraplegia. 1994; 32:70–80.9). Davis RA. A longterm outcome study of 170 surgically treated patients with compressive cervical radiculopathy. Surg Neurol. 1996; 46:523–530.
Article10). Raynor RB, Pugh J, Shapiro I. Cervical facetectomy and its effect on spine strength. J Neurosurg. 1985; 63:278–282.
Article11). Frykholm R. Deformities of dural pouches and strictures of dural sheaths in the cervical region producing nerve-root compression: A contribution to the etiology and operative treatment of brachial neuralgia. J Neurosurg. 1947; 4:403–413.12). Scoville WB, Whitcomb BB. Lateral rupture of cervical intervertebral disks. Postgrad Med. 1966; 39:174–180.
Article13). Grieve JP, Kitchen ND, Moore AJ, Marsh HT. Results of posterior cervical foraminotomy for treatment of cervical spondylitic radiculopathy. Br J Neurosurg. 2000; 14:40–43.14). Kumar GR, Maurice-Williams RS, Bradford R. Cervical foraminotomy: an effective treatment for cervical spondylotic radiculopathy. Br J Neurosurg. 1998; 12:563–568.
Article15). Witzmann A, Hejazi N, Krasznai L. Posterior cervical foraminotomy. A followup study of 67 surgically treated patients with compressive radiculopathy. Neurosurg Rev. 2000; 23:213–217.
Article16). Woertgen C, Holzschuh M, Rothoerl RD, Haeusler E, Brawanski A. Prognostic factors of posterior cervical disc surgery: a prospective, consecutive study of 54 patients. Neurosurgery. 1997; 40:724–728. discussion 728-729.
Article17). Kim KK, Choi BK, Choi CH. Surgical Results of Posterior Laminoforaminotomy and Discectomy for Cervical Disc Herniation. J Korean Neurosurg Soc. 2004; 36:138–144.18). Perez-Cruet MJ, Fessler RG, Perin NI. Review: complications of minimally invasive spinal surgery. Neurosurgery. 2002; 51:26–36.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison Between Open Procedure and Tubular Retractor Assisted Procedure for Cervical Radiculopathy: Results of a Randomized Controlled Study
- Usefulness of Minimally Invasive Posterior Foraminotomy using Tubular Retractor for Lumbar Spinal Stenosis with Foraminal Stenosis
- Posterior Endoscopic Cervical Decompression: Review and Technical Note
- Mini Open Foraminotomy for Cervical Radiculopathy: A Comparison of Large Tubular and TrimLine Retractors
- A Minimally Invasive Lumbar Spine Surgery Technique Using a Modified Thoracoport: Proposal of a New Tubular Retractor