J Endocr Surg.
2018 Jun;18(2):121-131. 10.16956/jes.2018.18.2.121.
Prevention, Identification and Management of Postoperative Hypoparathyroidism
- Affiliations
-
- 1Surgical Oncology Division, Department of Human Pathology in Adulthood and Childhood “G. Barresiâ€, University Hospital G. Martino, University of Messina, Messina, Italy.
- 2Department of Surgery, Policlinico Vittorio Emanuele University Hospital - General Surgery and Oncology Unit, University of Catania, Catania, Italy.
- 3Division of ENT Surgery, Department of Human Pathology in Adulthood and Childhood “G. Barresiâ€, University Hospital G. Martino, University of Messina, Messina, Italy.
- 4Division of Endocrine Surgery, Department of General Surgery, Ege University Hospital, Izmir, Turkey.
- 5Division for Endocrine and Minimally Invasive Surgery, Department of Human Pathology in Adulthood and Childhood “G. Barresiâ€, University Hospital G. Martino, University of Messina, Messina, Italy. gdionigi@unime.it
- KMID: 2420767
- DOI: http://doi.org/10.16956/jes.2018.18.2.121
Abstract
- The objective of this article is to detail and present our experience on the incidence and management of parathyroid dysfunction after thyroid surgery. Selective evaluation of original articles and reviews that were retrieved by a PubMed search over the years 1990 to 2018, as well as of the recommendations of medical societies including the American, European and Asian Thyroid/Endocrine Associations. The literature presents several contributions, with controversial results. The recommended management for the diagnosis and treatment of parathyroid dysfunction after bilateral thyroid surgery or recurrent surgery consists of an intact parathyroid hormone (iPTH) determination 12-24 hours after surgery and calcium substitution in iPTH < 15 pg/mL, no substitution with iPTH ≥15 pg/mL. This procedure is safe for the patient and is accepted by patients and social insurances (for short hospital stay).
MeSH Terms
Figure
Reference
-
1.Asari R., Passler C., Kaczirek K., Scheuba C., Niederle B. Hypoparathyroidism after total thyroidectomy: a prospective study. Arch Surg. 2008. 143:132–7.2.Selberherr A., Scheuba C., Riss P., Niederle B. Postoperative hypoparathyroidism after thyroidectomy: efficient and cost-effective diagnosis and treatment. Surgery. 2015. 157:349–53.
Article3.Pattou F., Combemale F., Fabre S., Carnaille B., Decoulx M., Wemeau JL, et al. Hypocalcemia following thyroid surgery: incidence and prediction of outcome. World J Surg. 1998. 22:718–24.
Article4.Sitges-Serra A., Ruiz S., Girvent M., Manjón H., Dueñas JP., Sancho JJ. Outcome of protracted hypoparathyroidism after total thyroidectomy. Br J Surg. 2010. 97:1687–95.
Article5.Bergenfelz A., Jansson S., Kristoffersson A., Mårtensson H., Reihnér E., Wallin G, et al. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg. 2008. 393:667–73.
Article6.Veyseller B., Aksoy F., Yildirim YS., Karatas A., Ozturan O. Effect of recurrent laryngeal nerve identification technique in thyroidectomy on recurrent laryngeal nerve paralysis and hypoparathyroidism. Arch Otolaryngol Head Neck Surg. 2011. 137:897–900.
Article7.Kara M., Tellioglu G., Krand O., Fersahoglu T., Berber I., Erdogdu E, et al. Predictors of hypocalcemia occurring after a total/near total thyroidectomy. Surg Today. 2009. 39:752–7.
Article8.Shaha AR., Burnett C., Jaffe BM. Parathyroid autotransplantation during thyroid surgery. J Surg Oncol. 1991. 46:21–4.
Article9.Reeve T., Thompson NW. Complications of thyroid surgery: how to avoid them, how to manage them, and observations on their possible effect on the whole patient. World J Surg. 2000. 24:971–5.
Article10.Hallgrimsson P., Nordenström E., Bergenfelz A., Almquist M. Hypocalcaemia after total thyroidectomy for Graves' disease and for benign atoxic multinodular goitre. Langenbecks Arch Surg. 2012. 397:1133–7.
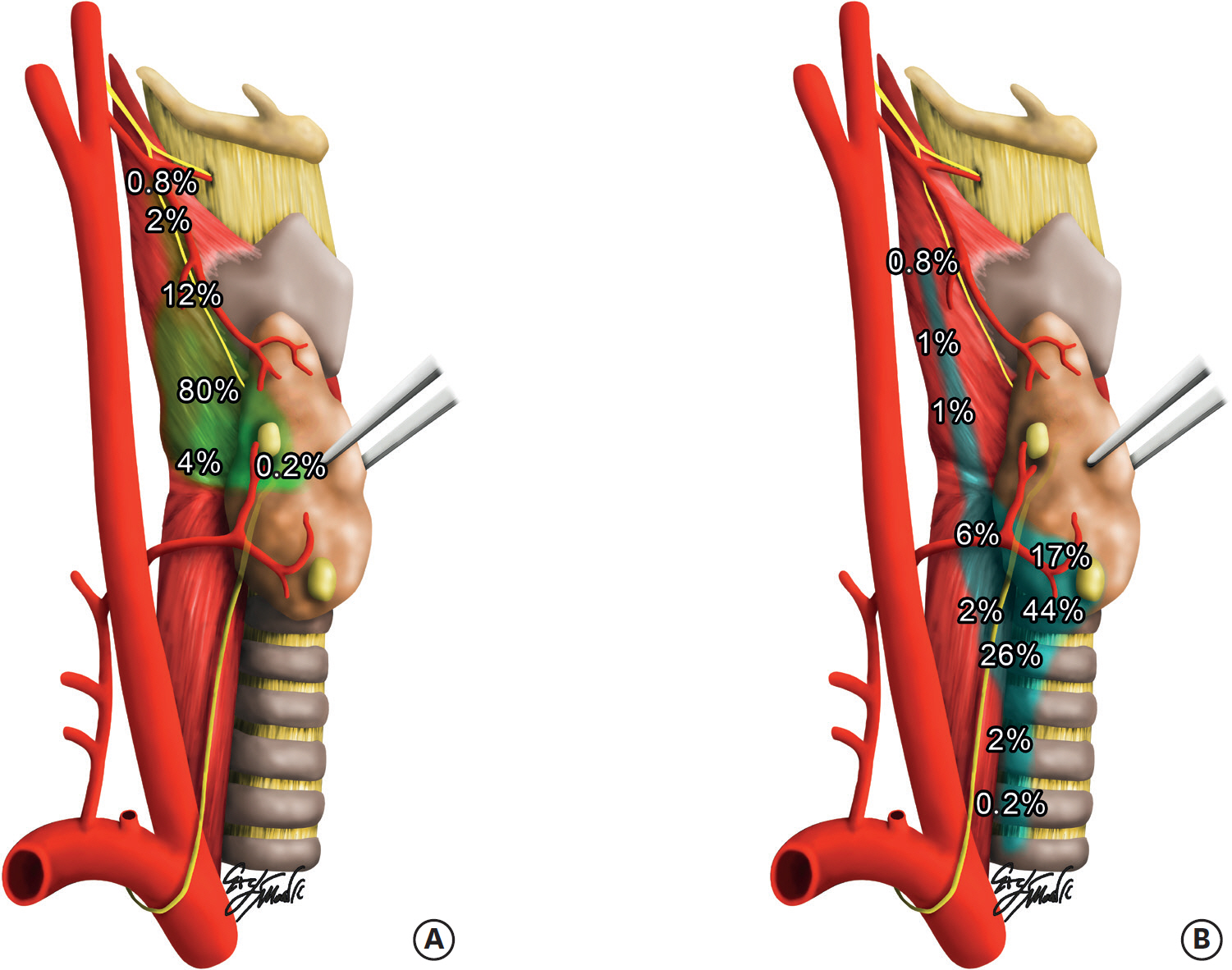
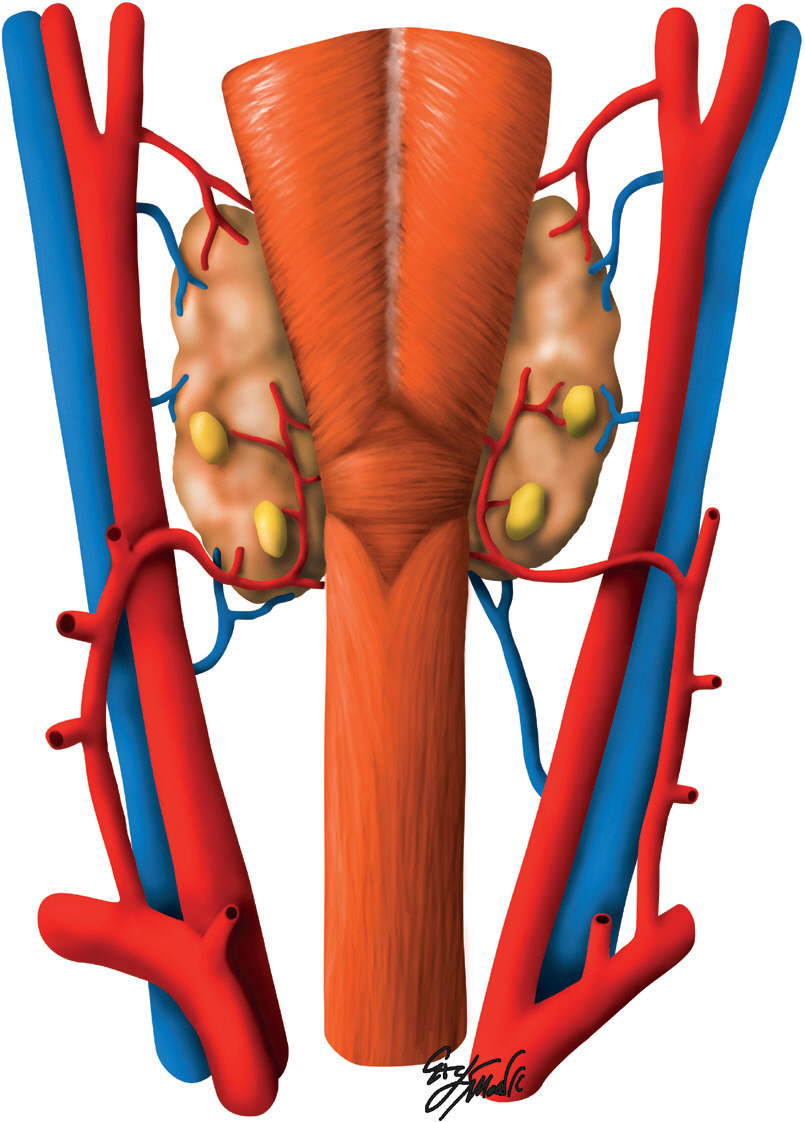
Article11.Mohebati A., Shaha AR. Anatomy of thyroid and parathyroid glands and neurovascular relations. Clin Anat. 2012. 25:19–31.
Article12.Policeni BA., Smoker WR., Reede DL. Anatomy and embryology of the thyroid and parathyroid glands. Semin Ultrasound CT MR. 2012. 33:104–14.
Article13.Testini M., Nacchiero M., Piccinni G., Portincasa P., Di Venere B., Lissidini G, et al. Total thyroidectomy is improved by loupe magnification. Microsurgery. 2004. 24:39–42.
Article14.Dionigi G., Van Slycke S., Rausei S., Boni L., Dionigi R. Parathyroid function after open thyroidectomy: a prospective randomized study for ligasure precise versus harmonic FOCUS. Head Neck. 2013. 35:562–7.
Article15.Saint Marc O., Cogliandolo A., Piquard A., Famà F., Pidoto RR. LigaSure vs clamp-and-tie technique to achieve hemostasis in total thyroidectomy for benign multinodular goiter: a prospective randomized study. Arch Surg. 2007. 142:150–6.16.Niederle B., Roka R., Brennan MF. The transplantation of parathyroid tissue in man: development, indications, technique, and results. Endocr Rev. 1982. 3:245–79.
Article17.Zedenius J., Wadstrom C., Delbridge L. Routine autotransplantation of at least one parathyroid gland during total thyroidectomy may reduce permanent hypoparathyroidism to zero. Aust N Z J Surg. 1999. 69:794–7.
Article18.Barczyń ski M., Konturek A., Stopa M., Cichoń S., Richter P., Nowak W. Total thyroidectomy for benign thyroid disease: is it really worthwhile? Ann Surg. 2011. 254:724–9.19.Erbil Y., Barbaros U., Salmaslioğ lu A., Yanik BT., Bozbora A., Ozarmağ an S. The advantage of near-total thyroidectomy to avoid postoperative hypoparathyroidism in benign multinodular goiter. Langenbecks Arch Surg. 2006. 391:567–73.
Article20.Dralle H. Postoperative hypoparathyroidism: central neck dissection is a significant risk factor. Chirurg. 2012. 83:1082.21.Wang JB., Wu K., Shi LH., Sun YY., Li FB., Xie L. In situ preservation of the inferior parathyroid gland during central neck dissection for papillary thyroid carcinoma. Br J Surg. 2017. 104:1514–22.
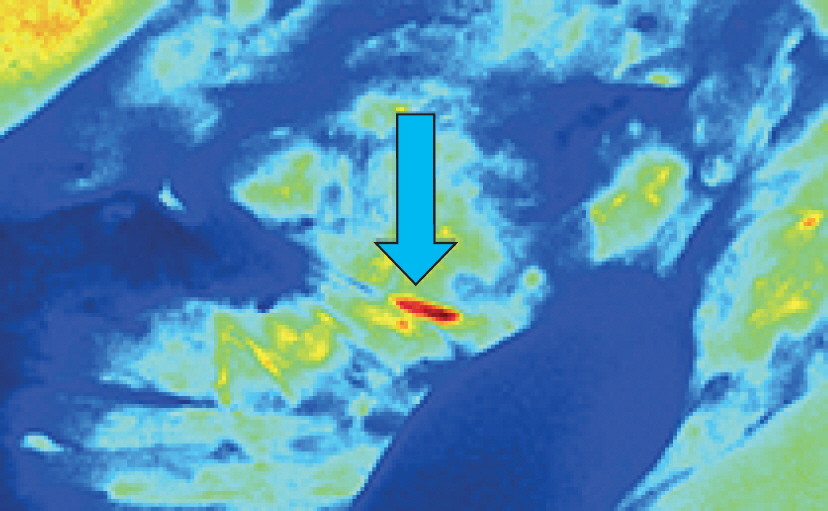
Article22.Vidal Fortuny J., Sadowski SM., Belfontali V., Guigard S., Poncet A., Ris F, et al. Randomized clinical trial of intraoperative parathyroid gland angiography with indocyanine green fluorescence predicting parathyroid function after thyroid surgery. Br J Surg. 2018. 105:350–57.
Article23.Riss P., Kaczirek K., Heinz G., Bieglmayer C., Niederle B. A “defined baseline” in PTH monitoring increases surgical success in patients with multiple gland disease. Surgery. 2007. 142:398–404.
Article24.Grodski S., Serpell J. Evidence for the role of perioperative PTH measurement after total thyroidectomy as a predictor of hypocalcemia. World J Surg. 2008. 32:1367–73.
Article25.Barczyń ski M., Cichoń S., Konturek A., Cichoń W. Applicability of intraoperative parathyroid hormone assay during total thyroidectomy as a guide for the surgeon to selective parathyroid tissue autotransplantation. World J Surg. 2008. 32:822–8.
Article26.Barczyń ski M., Cichoń S., Konturek A. Which criterion of intraoperative iPTH assay is the most accurate in prediction of true serum calcium levels after thyroid surgery? Langenbecks Arch Surg. 2007. 392:693–8.
Article27.Raffaelli M., De Crea C., Carrozza C., D'Amato G., Zuppi C., Bellantone R, et al. Combining early postoperative parathyroid hormone and serum calcium levels allows for an efficacious selective post-thyroidectomy supplementation treatment. World J Surg. 2012. 36:1307–13.
Article28.Doran HE., England J. Palazzo FBritish Association of Endocrine and Thyroid Surgeons. Questionable safety of thyroid surgery with same day discharge. Ann R Coll Surg Engl. 2012. 94:543–7.
Article29.Doran HE., Palazzo F. Day-case thyroid surgery. Br J Surg. 2012. 99:741–3.
Article30.Selberherr A., Niederle B. Avoidance and management of hypoparathyroidism after thyroid gland surgery. Chirurg. 2015. 86:13–6.31.Sung TY., Lee Y., Yoon JH., Chung KW., Hong SJ. The best surgical tips for parathyroid preservation in thyroid surgery. VideoEndocrinology. 2015. 2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors and Prevention (New Technology) for Hypoparathyroidism after Thyroidectomy
- Postoperative Hypoparathyroidism and the Viability of the Parathyroid Glands During Thyroidectomy
- Postoperative Change of Ionized Calcium Level after Total Thyroidectomy and Risk Factors of Postoperative Permanent Hypoparathyroidism
- Hypoparathyroidism in children and adolescents
- Hypoparathyroidism, sensorineural deafness, and renal dysgenesis syndrome with a GATA3 mutation