Yonsei Med J.
2018 Mar;59(2):310-316. 10.3349/ymj.2018.59.2.310.
Infarct Core Expansion on Computed Tomography before and after Intravenous Thrombolysis
- Affiliations
-
- 1Department of Neurology, Yonsei University College of Medicine, Seoul, Korea. jhheo@yuhs.ac
- 2Department of Neurology, CHA Bundang Medical Center, CHA University, Seongnam, Korea.
- 3Department of Biostatistics, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2418796
- DOI: http://doi.org/10.3349/ymj.2018.59.2.310
Abstract
- PURPOSE
Infarct core can expand rapidly in acute stroke patients receiving intravenous tissue plasminogen activator (IV t-PA). We investigated changes in the extent of infarct core during IV t-PA treatment, and explored the associative factors of this infarct core expansion in patients with proximal artery occlusion.
MATERIALS AND METHODS
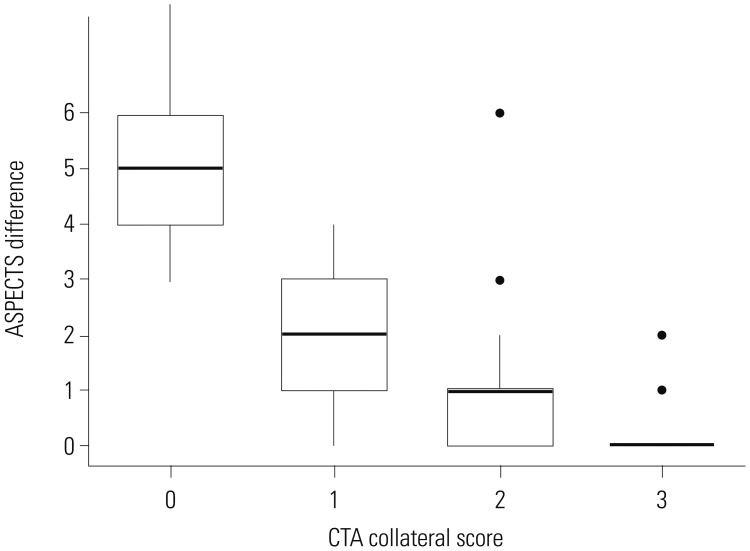
We included patients who were considered for sequential intra-arterial therapy (IAT) due to occlusion of intracranial proximal artery after IV t-PA. Patients who had a baseline Alberta Stroke Program Early Computed Tomography (CT) Score (ASPECTS) ≥6 and who underwent two consecutive CT scans before and shortly after IV t-PA infusion were enrolled. Patients were classified into no, moderate, and marked expansion groups based on decreases in ASPECTS (0-1, 2-3, and ≥4, respectively) on follow-up CT. Collateral status was graded using CT angiography.
RESULTS
Of the 104 patients, 16 (15.4%) patients showed moderate and 13 (12.5%) patients showed marked infarct core expansion on follow-up CT scans obtained at 71.1±19.1 min after baseline CT scan. Sixteen (15.4%) patients had an ASPECTS value < 6 on the follow-up CT. None of the patients with marked expansion were independent at 3 months. Univariate analysis and ordinal logistic regression analysis demonstrated that the infarct core expansion was significantly associated with collateral status (p < 0.001).
CONCLUSION
Among patients who were considered for IAT after IV t-PA treatment, one out of every seven patients exhibited marked expansion of infarct core on follow-up CT before IAT. These patients tend to have poor collaterals and poor outcomes despite rescue IAT.
Keyword
MeSH Terms
Figure
Reference
-
1. Badhiwala JH, Nassiri F, Alhazzani W, Selim MH, Farrokhyar F, Spears J, et al. Endovascular thrombectomy for acute ischemic stroke: a meta-analysis. JAMA. 2015; 314:1832–1843. PMID: 26529161.2. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20. PMID: 25517348.3. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018. PMID: 25671797.
Article4. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030. PMID: 25671798.5. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306. PMID: 25882510.
Article6. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–2295. PMID: 25882376.
Article7. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731. PMID: 26898852.
Article8. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare [rofessionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46:3020–3035. PMID: 26123479.
Article9. Song D, Lee K, Kim EH, Kim YD, Kim J, Song TJ, et al. Value of utilizing both ASPECTS and CT angiography collateral score for outcome prediction in acute ischemic stroke. Int J Stroke. 2015; 10:1018–1023. PMID: 25907633.
Article10. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. 2016; 316:1279–1288. PMID: 27673305.
Article11. Menon BK, Campbell BC, Levi C, Goyal M. Role of imaging in current acute ischemic stroke workflow for endovascular therapy. Stroke. 2015; 46:1453–1461. PMID: 25944319.
Article12. Kim YD, Nam HS, Kim SH, Kim EY, Song D, Kwon I, et al. Time-dependent thrombus resolution after tissue-type plasminogen activator in patients with stroke and mice. Stroke. 2015; 46:1877–1882. PMID: 25967573.
Article13. Nam HS, Kim EY, Kim SH, Kim YD, Kim J, Lee HS, et al. Prediction of thrombus resolution after intravenous thrombolysis assessed by CT-based thrombus imaging. Thromb Haemost. 2012; 107:786–794. PMID: 22318312.
Article14. Puetz V, Dzialowski I, Hill MD, Demchuk AM. The Alberta Stroke Program Early CT Score in clinical practice: what have we learned? Int J Stroke. 2009; 4:354–364. PMID: 19765124.
Article15. Tan JC, Dillon WP, Liu S, Adler F, Smith WS, Wintermark M. Systematic comparison of perfusion-CT and CT-angiography in acute stroke patients. Ann Neurol. 2007; 61:533–543. PMID: 17431875.
Article16. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329. PMID: 18815396.
Article18. Shuaib A, Butcher K, Mohammad AA, Saqqur M, Liebeskind DS. Collateral blood vessels in acute ischaemic stroke: a potential therapeutic target. Lancet Neurol. 2011; 10:909–921. PMID: 21939900.
Article19. Jung S, Gilgen M, Slotboom J, El-Koussy M, Zubler C, Kiefer C, et al. Factors that determine penumbral tissue loss in acute ischaemic stroke. Brain. 2013; 136(Pt 12):3554–3560. PMID: 24065722.
Article20. Miteff F, Levi CR, Bateman GA, Spratt N, McElduff P, Parsons MW. The independent predictive utility of computed tomography angiographic collateral status in acute ischaemic stroke. Brain. 2009; 132(Pt 8):2231–2238. PMID: 19509116.
Article21. Campbell BC, Christensen S, Tress BM, Churilov L, Desmond PM, Parsons MW, et al. Failure of collateral blood flow is associated with infarct growth in ischemic stroke. J Cereb Blood Flow Metab. 2013; 33:1168–1172. PMID: 23652626.
Article22. Bang OY, Saver JL, Kim SJ, Kim GM, Chung CS, Ovbiagele B, et al. Collateral flow predicts response to endovascular therapy for acute ischemic stroke. Stroke. 2011; 42:693–699. PMID: 21233472.
Article23. Leng X, Fang H, Leung TW, Mao C, Miao Z, Liu L, et al. Impact of collaterals on the efficacy and safety of endovascular treatment in acute ischaemic stroke: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2016; 87:537–544. PMID: 26063928.
Article24. Menon BK, Qazi E, Nambiar V, Foster LD, Yeatts SD, Liebeskind D, et al. Differential effect of baseline computed tomographic angiography collaterals on clinical outcome in patients enrolled in the Interventional Management of Stroke III Trial. Stroke. 2015; 46:1239–1244. PMID: 25791716.
Article25. Khatri P, Abruzzo T, Yeatts SD, Nichols C, Broderick JP, Tomsick TA. IMS I and II Investigators. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology. 2009; 73:1066–1072. PMID: 19786699.
Article26. Khatri P, Yeatts SD, Mazighi M, Broderick JP, Liebeskind DS, Demchuk AM, et al. Time to angiographic reperfusion and clinical outcome after acute ischaemic stroke: an analysis of data from the Interventional Management of Stroke (IMS III) phase 3 trial. Lancet Neurol. 2014; 13:567–574. PMID: 24784550.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Reperfusion Experimental Myocardial Infarction in Rats
- Coronary Thrombolysis with Intravenous Urokinase in Acute Myocardial Infarction
- Discrepancy in core infarct betweennon-contrast CT and CT perfusionwhen selecting for mechanicalthrombectomy
- Infective endocarditis with embolic renal infarct presenting as acute abdomen
- Renal Subcapsular Hematoma after Intravenous Thrombolysis in a Patient with Acute Cerebral Infarction