Ann Surg Treat Res.
2018 Aug;95(2):111-120. 10.4174/astr.2018.95.2.111.
Clinical usefulness of transarterial chemoembolization response prior to liver transplantation as predictor of optimal timing for living donor liver transplantation
- Affiliations
-
- 1Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea.
- 2Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jw.joh@samsung.com
- 3Department of Surgery, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Korea.
- KMID: 2417777
- DOI: http://doi.org/10.4174/astr.2018.95.2.111
Abstract
- PURPOSE
Response to preoperative transarterial chemoembolization (TACE) has been recommended as a biological selection criterion for liver transplantation (LT). The aim of our study was to identify optimal timing of living donor liver transplantation (LDLT) after TACE based on the TACE response.
METHODS
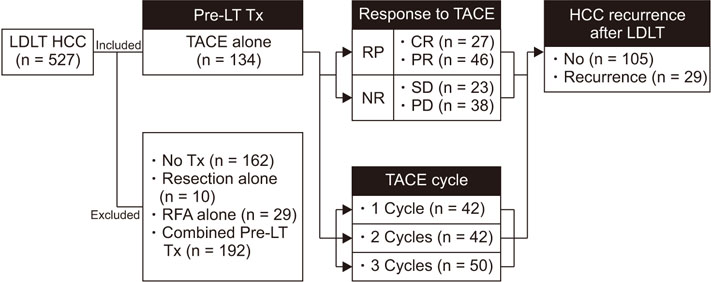
We performed a retrospective study to assess recurrence in 128 hepatocellular carcinoma (HCC) patients who underwent LDLT following sequential TACE from January 2002 to March 2015 at a single institute. Cox proportional hazard models and Kaplan-Meier analysis were utilized to estimate HCC recurrence and find optimal timing for LDLT.
RESULTS
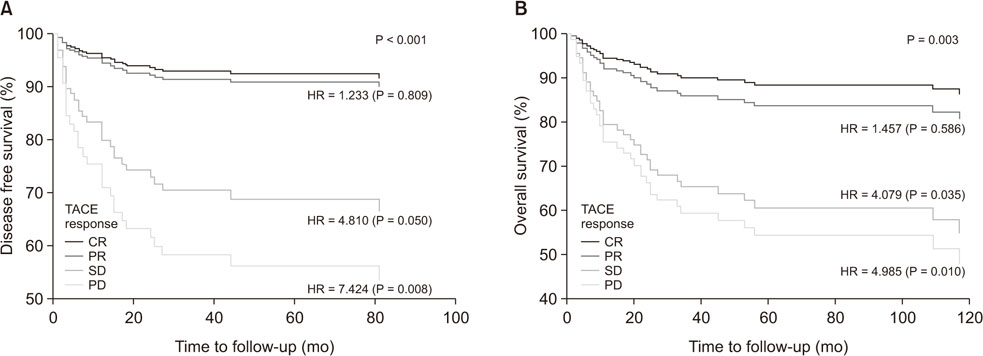
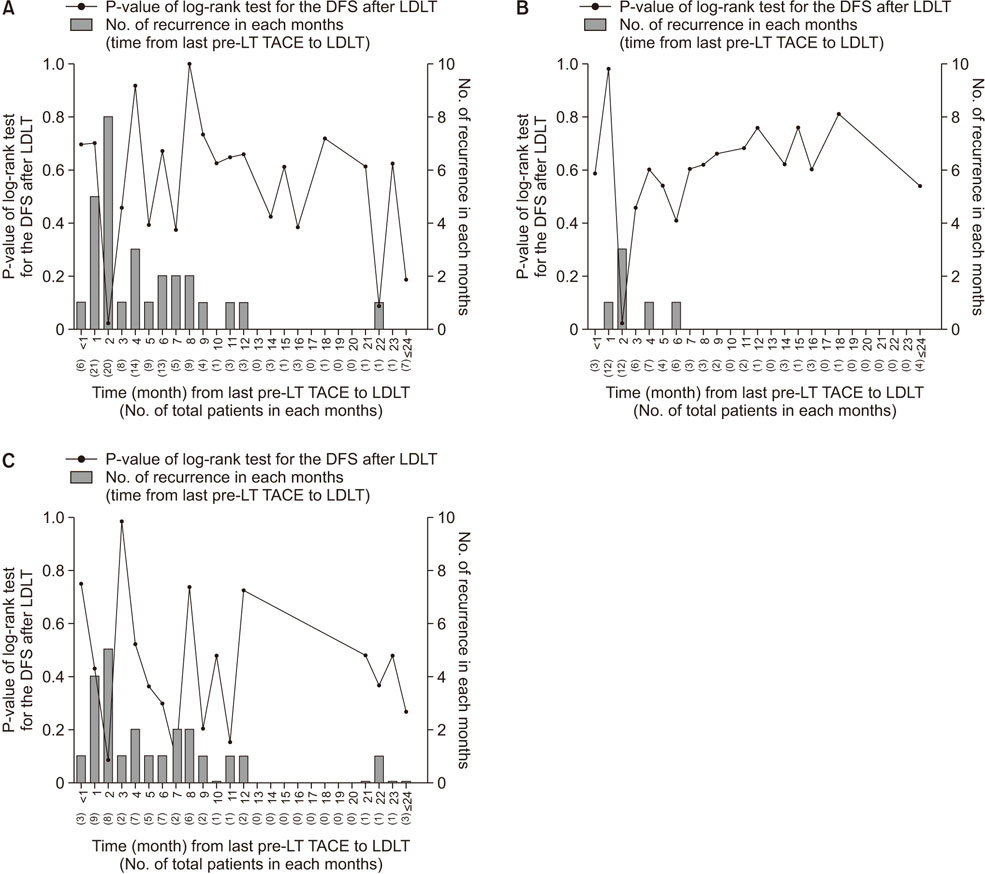
Seventy-three and 61 patients were divided as the responder and nonresponder, respectively. Multivariate analysis showed independent pre-liver transplantation (pre-LT) predictors of recurrence were larger sized tumor (>3 cm, P = 0.024), nonresponse to TACE (P = 0.031), vascular invasion (P = 0.002), and extrahepatic nodal involvement (P = 0.001). In the 3-month time difference between last pre-LT TACE and LDLT subgroup, TACE responders showed significantly higher adjusted hazard ratio (aHR) of recurrence free survival (aHR, 6.284; P = 0.007), cancer specific survival (aHR, 7.033; P = 0.016), and overall survival (aHR, 7.055; P = 0.005). Moreover, for overall patients and responder groups, the significant time difference between last pre-LT TACE and LDLT was 2 months in the minimum P-value approach.
CONCLUSION
In selected patients who showed good response to pre-LT TACE, a shorter time interval between TACE and LDLT may be associated with higher recurrence free survival, cancer specific survival, and overall survival.
MeSH Terms
Figure
Reference
-
1. Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996; 334:693–699.
Article2. Kim JM, Kwon CH, Joh JW, Kim SJ, Shin M, Kim EY, et al. Patients with unresectable hepatocellular carcinoma beyond Milan criteria: should we perform transarterial chemoembolization or liver transplantation? Transplant Proc. 2010; 42:821–824.
Article3. Kwon CH, Kim DJ, Han YS, Park JB, Choi GS, Kim SJ, et al. HCC in living donor liver transplantation: can we expand the Milan criteria? Dig Dis. 2007; 25:313–319.
Article4. Otto G, Schuchmann M, Hoppe-Lotichius M, Heise M, Weinmann A, Hansen T, et al. How to decide about liver transplantation in patients with hepatocellular carcinoma: size and number of lesions or response to TACE? J Hepatol. 2013; 59:279–284.
Article5. Yang SH, Suh KS, Lee HW, Cho EH, Cho JY, Cho YB, et al. A revised scoring system utilizing serum alphafetoprotein levels to expand candidates for living donor transplantation in hepatocellular carcinoma. Surgery. 2007; 141:598–609.
Article6. Yao FY. Selection criteria for liver transplantation in patients with hepatocellular carcinoma: beyond tumor size and number? Liver Transpl. 2006; 12:1189–1191.
Article7. Hwang S, Lee SG, Belghiti J. Liver transplantation for HCC: its role: Eastern and Western perspectives. J Hepatobiliary Pancreat Sci. 2010; 17:443–448.8. Lee SG, Moon DB. Living donor liver transplantation for hepatocellular carcinoma. Recent Results Cancer Res. 2013; 190:165–179.
Article9. Pompili M, Francica G, Ponziani FR, Iezzi R, Avolio AW. Bridging and downstaging treatments for hepatocellular carcinoma in patients on the waiting list for liver transplantation. World J Gastroenterol. 2013; 19:7515–7530.
Article10. Terzi E, Ray Kim W, Sanchez W, Charlton MR, Schmeltzer P, Gores GJ, et al. Impact of multiple transarterial chemoembolization treatments on hepatocellular carcinoma for patients awaiting liver transplantation. Liver Transpl. 2015; 21:248–257.
Article11. Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: Chemoembolization improves survival. Hepatology. 2003; 37:429–442.
Article12. Kim DJ, Clark PJ, Heimbach J, Rosen C, Sanchez W, Watt K, et al. Recurrence of hepatocellular carcinoma: importance of mRECIST response to chemoembolization and tumor size. Am J Transplant. 2014; 14:1383–1390.
Article13. Millonig G, Graziadei IW, Freund MC, Jaschke W, Stadlmann S, Ladurner R, et al. Response to preoperative chemoembolization correlates with outcome after liver transplantation in patients with hepatocellular carcinoma. Liver Transpl. 2007; 13:272–279.
Article14. Otto G, Herber S, Heise M, Lohse AW, Monch C, Bittinger F, et al. Response to transarterial chemoembolization as a biological selection criterion for liver transplantation in hepatocellular carcinoma. Liver Transpl. 2006; 12:1260–1267.
Article15. Vitale A, D'Amico F, Frigo AC, Grigoletto F, Brolese A, Zanus G, et al. Response to therapy as a criterion for awarding priority to patients with hepatocellular carcinoma awaiting liver transplantation. Ann Surg Oncol. 2010; 17:2290–2302.
Article16. Yamamoto Y, Ikoma H, Morimura R, Konishi H, Murayama Y, Komatsu S, et al. Optimal duration of the early and late recurrence of hepatocellular carcinoma after hepatectomy. World J Gastroenterol. 2015; 21:1207–1215.
Article17. Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010; 30:52–60.
Article18. Bargellini I, Vignali C, Cioni R, Petruzzi P, Cicorelli A, Campani D, et al. Hepatocellular carcinoma: CT for tumor response after transarterial chemoembolization in patients exceeding Milan criteria--selection parameter for liver transplantation. Radiology. 2010; 255:289–300.
Article19. Yao FY, Bass NM, Nikolai B, Davern TJ, Kerlan R, Wu V, et al. Liver transplantation for hepatocellular carcinoma: analysis of survival according to the intention-to-treat principle and dropout from the waiting list. Liver Transpl. 2002; 8:873–883.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hepatic Artery Reconstruction Using the Right Gastroepiploic Artery for Hepatic Artery Inflow in a Living Donor Liver Transplantation
- Liver retransplantation for adult recipients
- Optimal Timing and Evaluation of Liver Transplantation
- Pediatric liver transplantation in Korea: long-term outcomes and allocations
- Indication and Outcome of Liver Transplantation In Patients with Hepatocellular Carcinoma