Cancer Res Treat.
2018 Apr;50(2):551-561. 10.4143/crt.2017.189.
Evaluation of the Benefit of Radiotherapy in Patients with Occult Breast Cancer: A Population-Based Analysis of the SEER Database
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Radiation Oncology, Chungnam National University College of Medicine, Daejeon, Korea. ijeannyi@daum.net
- 3Department of Radiation Oncology, Ewha Womans University College of Medicine, Seoul, Korea. kyubokim.ro@gmail.com
- KMID: 2411143
- DOI: http://doi.org/10.4143/crt.2017.189
Abstract
- PURPOSE
Few studies for occult breast cancer (OBC) have evaluated the effect of radiotherapy (RT) after mastectomy or axillary lymph node dissection (ALND) with/without breast surgery. Therefore, we investigated clinicopathologic factors of OBC with the impact of postoperative RT to determine its prognostic significance using large population-based data.
MATERIALS AND METHODS
We performed a retrospective cohort study using the Surveillance, Epidemiology, and End Results (SEER) database from 1983 to 2013. A total of 1,045 eligible patients with OBC were identified. We compared overall survival (OS) using Cox proportional hazards regression with propensity score matching after verifying an imbalance of prognosticators between RT group (n=518) and non-RT group (n=479).
RESULTS
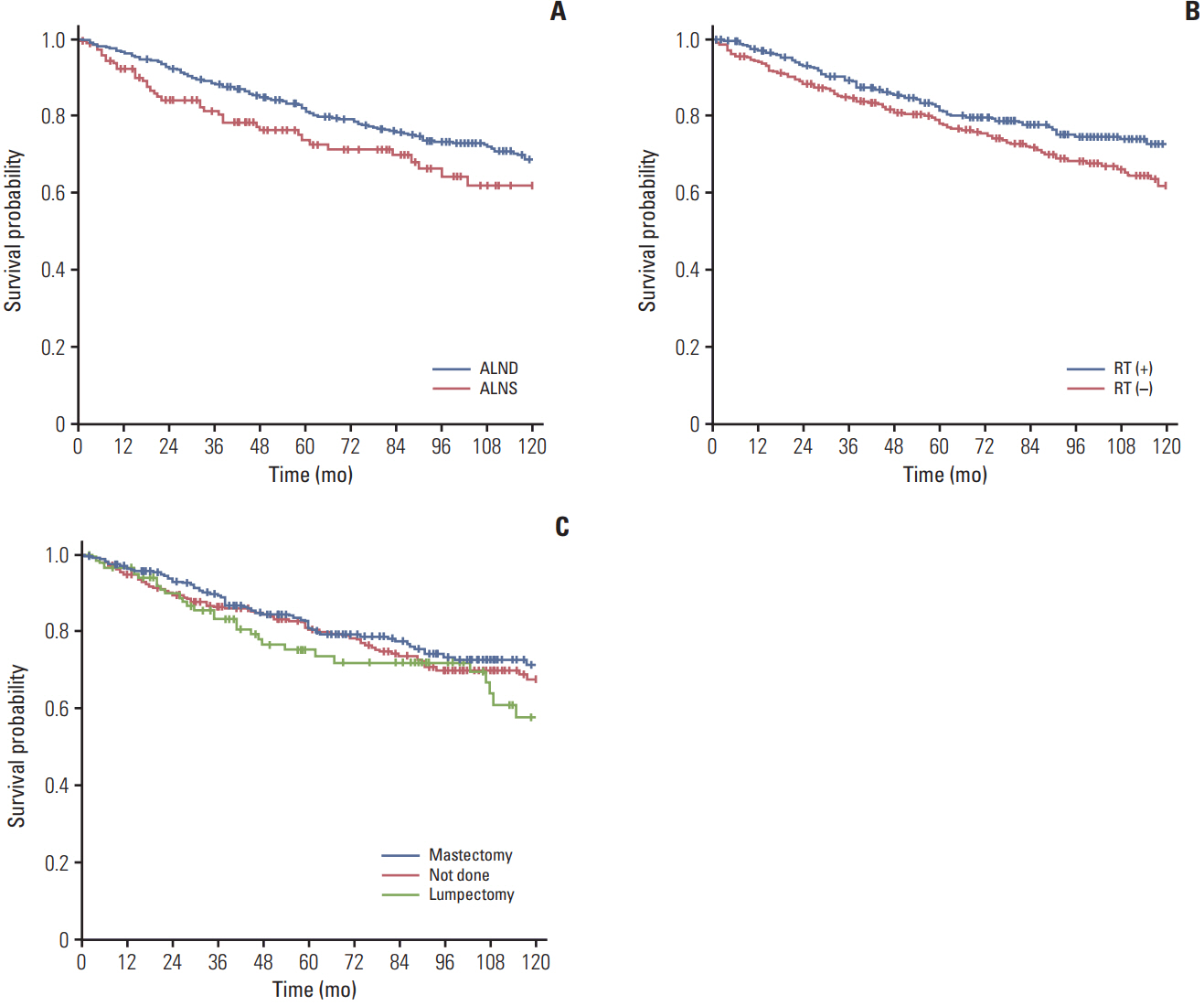
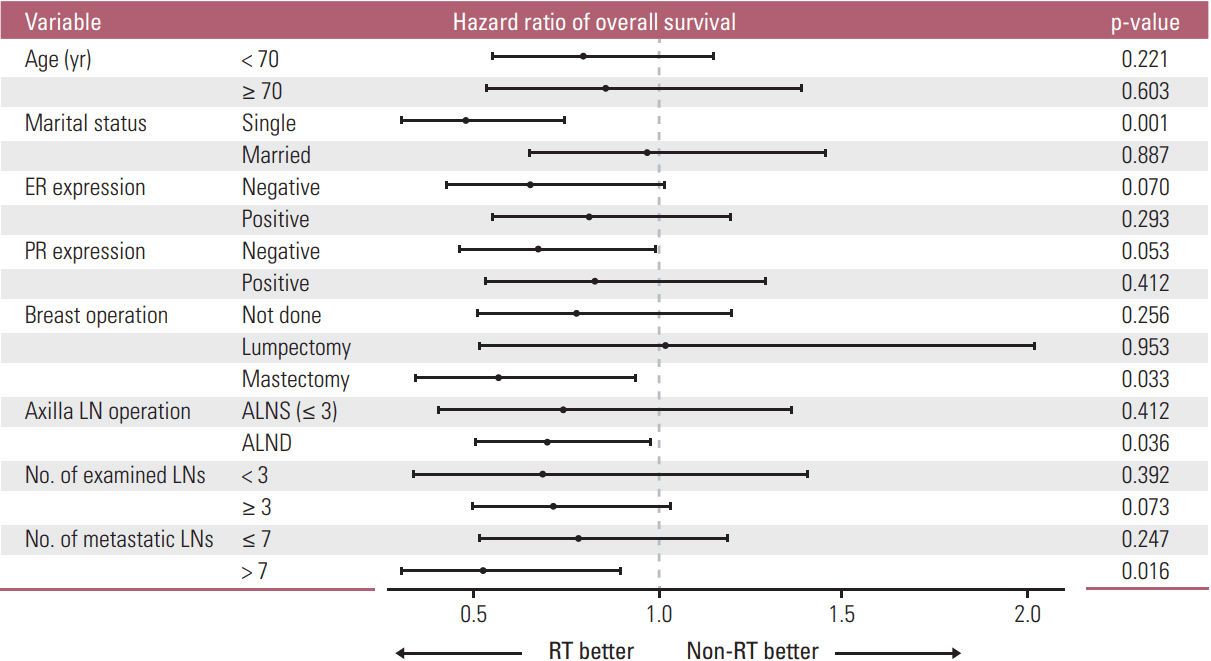
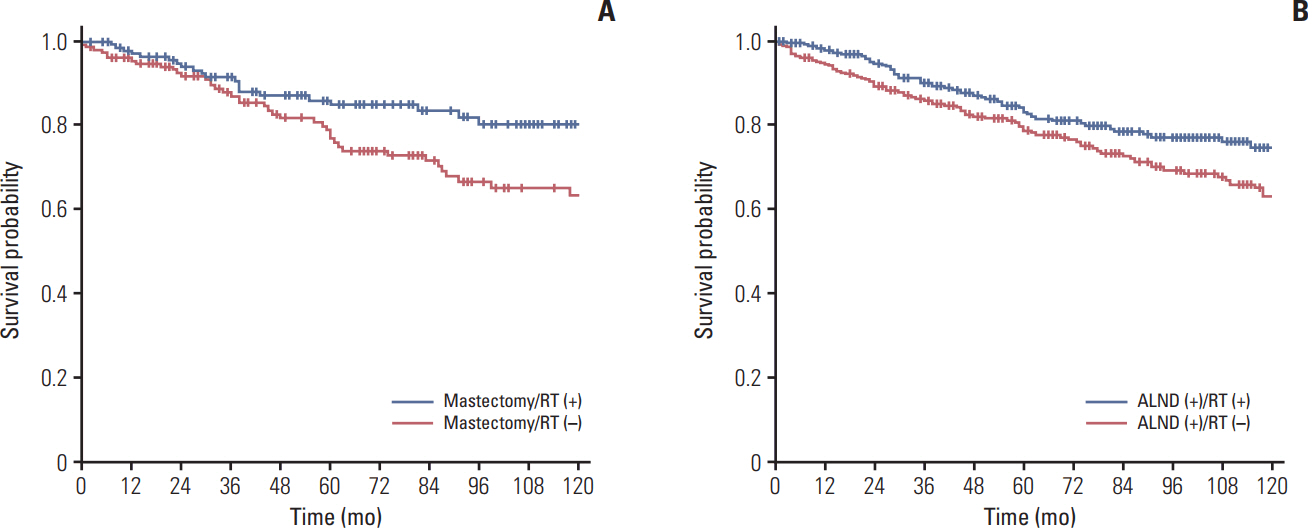
Patients with age < 70 (p=0.033), married marital status (p < 0.001), undergoing ALND (p < 0.001), more examined lymph nodes (LNs) (p < 0.001), and more metastatic LNs (p < 0.001) were more likely to receive RT. Multivariate analysis after propensity score matching (n=798) showed that patients treated with RT survived significantly longer than those without RT (5-year OS, 81.5% vs. 78.3%; p=0.014). A significantly prolonged OS was observed when RT was given to patients treated with mastectomy (p=0.033), those treated with ALND (p=0.036), or those with more than seven metastatic LNs (p=0.016).
CONCLUSION
RT may offer survival benefit in OBC even after mastectomy or ALND, especially in patients with more than seven metastatic LNs. Further prospective studies are needed to validate these findings.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Patel J, Nemoto T, Rosner D, Dao TL, Pickren JW. Axillary lymph node metastasis from an occult breast cancer. Cancer. 1981; 47:2923–7.
Article2. Walker GV, Smith GL, Perkins GH, Oh JL, Woodward W, Yu TK, et al. Population-based analysis of occult primary breast cancer with axillary lymph node metastasis. Cancer. 2010; 116:4000–6.
Article3. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology, Breast cancer. v.2.2016 [Internet]. Fort Washington, PA: National Comprehensive Cancer Network;2016. [cited 2017 Jun 1]. Available from: http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf.4. Masinghe SP, Faluyi OO, Kerr GR, Kunkler IH. Breast radiotherapy for occult breast cancer with axillary nodal metastases: does it reduce the local recurrence rate and increase overall survival? Clin Oncol (R Coll Radiol). 2011; 23:95–100.5. He M, Tang LC, Yu KD, Cao AY, Shen ZZ, Shao ZM, et al. Treatment outcomes and unfavorable prognostic factors in patients with occult breast cancer. Eur J Surg Oncol. 2012; 38:1022–8.
Article6. Sohn G, Son BH, Lee SJ, Kang EY, Jung SH, Cho SH, et al. Treatment and survival of patients with occult breast cancer with axillary lymph node metastasis: a nationwide retrospective study. J Surg Oncol. 2014; 110:270–4.
Article7. Rueth NM, Black DM, Limmer AR, Gabriel E, Huo L, Fornage BD, et al. Breast conservation in the setting of contemporary multimodality treatment provides excellent outcomes for patients with occult primary breast cancer. Ann Surg Oncol. 2015; 22:90–5.
Article8. Fayanju OM, Stoll CR, Fowler S, Colditz GA, Jeffe DB, Margenthaler JA. Geographic and temporal trends in the management of occult primary breast cancer: a systematic review and meta-analysis. Ann Surg Oncol. 2013; 20:3308–16.
Article9. Khandelwal AK, Garguilo GA. Therapeutic options for occult breast cancer: a survey of the American Society of Breast Surgeons and review of the literature. Am J Surg. 2005; 190:609–13.
Article10. Sagara Y, Freedman RA, Vaz-Luis I, Mallory MA, Wong SM, Aydogan F, et al. Patient prognostic score and associations with survival improvement offered by radiotherapy after breast-conserving surgery for ductal carcinoma in situ: a population-based longitudinal cohort study. J Clin Oncol. 2016; 34:1190–6.
Article11. Orel SG, Weinstein SP, Schnall MD, Reynolds CA, Schuchter LM, Fraker DL, et al. Breast MR imaging in patients with axillary node metastases and unknown primary malignancy. Radiology. 1999; 212:543–9.
Article12. Vlastos G, Jean ME, Mirza AN, Mirza NQ, Kuerer HM, Ames FC, et al. Feasibility of breast preservation in the treatment of occult primary carcinoma presenting with axillary metastases. Ann Surg Oncol. 2001; 8:425–31.
Article13. EBCTCG (Early Breast Cancer Trialists' Collaborative Group), McGale P, Taylor C, Correa C, Cutter D, Duane F, et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: metaanalysis of individual patient data for 8135 women in 22 randomised trials. Lancet. 2014; 383:2127–35.14. Recht A, Comen EA, Fine RE, Fleming GF, Hardenbergh PH, Ho AY, et al. Postmastectomy radiotherapy: an American Society of Clinical Oncology, American Society for Radiation Oncology, and Society of Surgical Oncology focused guideline update. Pract Radiat Oncol. 2016; 6:e219–34.
Article15. Park HJ, Shin KH, Kim JH, Ahn SD, Kim JY, Park W, et al. Incorporating risk factors to identify the indication of postmastectomy radiotherapy in N1 breast cancer treated with optimal systemic therapy: a multicenter analysis in Korea (KROG 14-23). Cancer Res Treat. 2017; 49:739–47.
Article16. Barton SR, Smith IE, Kirby AM, Ashley S, Walsh G, Parton M. The role of ipsilateral breast radiotherapy in management of occult primary breast cancer presenting as axillary lymphadenopathy. Eur J Cancer. 2011; 47:2099–106.
Article17. Shannon C, Walsh G, Sapunar F, A'Hern R, Smith I. Occult primary breast carcinoma presenting as axillary lymphadenopathy. Breast. 2002; 11:414–8.
Article18. Ellerbroek N, Holmes F, Singletary E, Evans H, Oswald M, McNeese M. Treatment of patients with isolated axillary nodal metastases from an occult primary carcinoma consistent with breast origin. Cancer. 1990; 66:1461–7.
Article19. Blanchard DK, Farley DR. Retrospective study of women presenting with axillary metastases from occult breast carcinoma. World J Surg. 2004; 28:535–9.
Article20. Macedo FI, Eid JJ, Flynn J, Jacobs MJ, Mittal VK. Optimal surgical management for occult breast carcinoma: a meta-analysis. Ann Surg Oncol. 2016; 23:1838–44.
Article21. Woo SM, Son BH, Lee JW, Kim HJ, Yu JH, Ko BS, et al. Survival outcomes of different treatment methods for the ipsilateral breast of occult breast cancer patients with axillary lymph node metastasis: a single center experience. J Breast Cancer.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optimal positive lymph node ratio showing the benefit of postoperative radiotherapy in pathologic N2 non-small cell lung cancer: an exploratory study using the Surveillance, Epidemiology, and End Results data
- Omitting Adjuvant Radiotherapy for Hormone Receptor‒Positive Early-Stage Breast Cancer in Old Age: A Propensity Score Matched SEER Analysis
- Current Approaches in Development of Immunotherapeutic Vaccines for Breast Cancer
- Interactions of Family History of Breast Cancer with Radiotherapy in Relation to the Risk of Breast Cancer Recurrence
- Identification of Biomarkers for Breast Cancer Using Databases