Cancer Res Treat.
2019 Jan;51(1):326-336. 10.4143/crt.2018.163.
Omitting Adjuvant Radiotherapy for Hormone Receptor‒Positive Early-Stage Breast Cancer in Old Age: A Propensity Score Matched SEER Analysis
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University College of Medicine, Seoul, Korea. radiat@snu.ac.kr
- 2Department of Radiation Oncology, Ewha Womans University College of Medicine, Seoul, Korea.
- KMID: 2437623
- DOI: http://doi.org/10.4143/crt.2018.163
Abstract
- PURPOSE
The purpose of this study was to investigate the non-inferiority of omitting radiotherapy (RT) after breast-conserving surgery (BCS) for hormone receptor (HR)"’positive T1N0 breast cancer in elderly women.
MATERIALS AND METHODS
From 2004 to 2014, HR-positive T1N0 breast cancer patients aged 50 years or older and receiving BCS were retrieved from the Surveillance, Epidemiology, and End
RESULTS
18 database. After propensity score matching between the no-RT and RT groups, univariate and multivariate analyses were performed. Identified prognostic factors were used to stratify the risk groups. In each risk group, 10-year cancer-specific survival (CSS) rates were compared between the no-RT and RT groups.
RESULTS
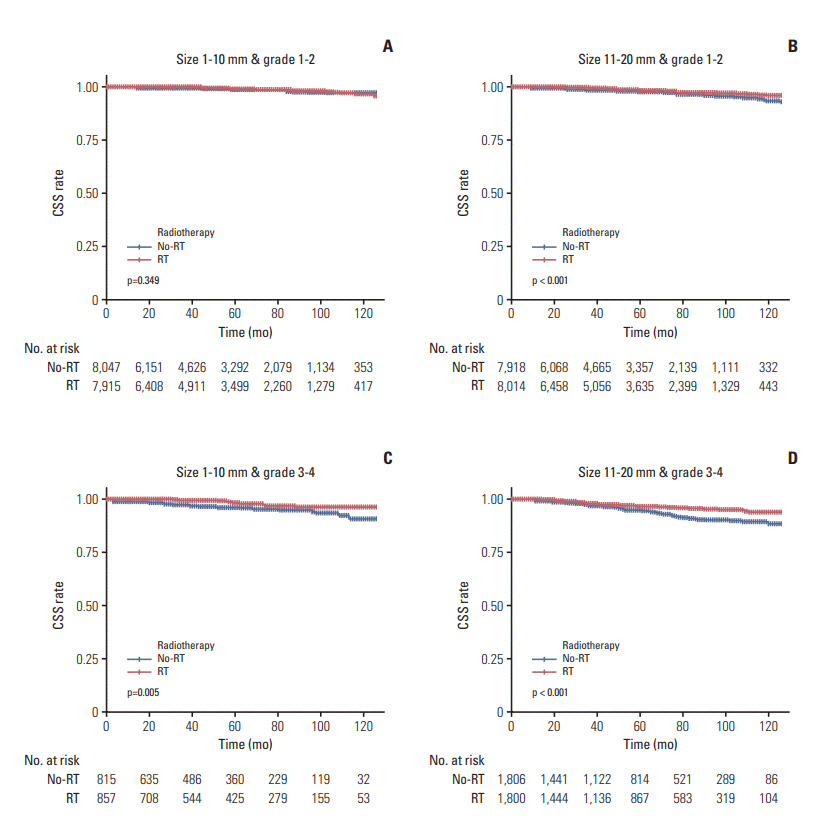
After propensity score matching, the numbers of patients in the no-RT and RT groups were both 18,586. For patients who satisfied both a tumor size of 1-10 mm and a tumor grade of 1-2, omitting RT did not decrease the CSS rate at any age group, ranging from ≥ 50 to ≥ 85 years; for patients aged ≥ 50 years, the 10-year CSS rates in the no-RT and RT groups were 97.2% and 96.8%, respectively (adjusted hazard ratio, 0.862; p=0.312). However, for patients with a tumor size of 11-20 mm or tumor grade of 3-4, RT significantly increased the CSS rate irrespective of age.
CONCLUSION
RT after BCS for HR-positive T1N0 breast cancer in elderly women might be omitted without causing a decrease in the CSS rate, but only in patients who satisfy both a small tumor size (≤ 10 mm) and low tumor grade (1-2).
Keyword
MeSH Terms
Figure
Reference
-
References
1. Girones R, Torregrosa D, Diaz-Beveridge R. Comorbidity, disability and geriatric syndromes in elderly breast cancer survivors: results of a single-center experience. Crit Rev Oncol Hematol. 2010; 73:236–45.2. van de Water W, Markopoulos C, van de Velde CJ, Seynaeve C, Hasenburg A, Rea D, et al. Association between age at diagnosis and disease-specific mortality among postmenopausal women with hormone receptor-positive breast cancer. JAMA. 2012; 307:590–7.
Article3. Bovelli D, Plataniotis G, Roila F; ESMO Guidelines Working Group. Cardiotoxicity of chemotherapeutic agents and radiotherapy-related heart disease: ESMO Clinical Practice Guidelines. Ann Oncol. 2010; 21 Suppl 5:v277–82.
Article4. Arvold ND, Taghian AG, Niemierko A, Abi Raad RF, Sreedhara M, Nguyen PL, et al. Age, breast cancer subtype approximation, and local recurrence after breast-conserving therapy. J Clin Oncol. 2011; 29:3885–91.
Article5. Bastiaannet E, Portielje JE, van de Velde CJ, de Craen AJ, van der Velde S, Kuppen PJ, et al. Lack of survival gain for elderly women with breast cancer. Oncologist. 2011; 16:415–23.
Article6. Hughes KS, Schnaper LA, Bellon JR, Cirrincione CT, Berry DA, McCormick B, et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. J Clin Oncol. 2013; 31:2382–7.
Article7. Kunkler IH, Williams LJ, Jack WJ, Cameron DA, Dixon JM; PRIME II investigators. Breast-conserving surgery with or without irradiation in women aged 65 years or older with early breast cancer (PRIME II): a randomised controlled trial. Lancet Oncol. 2015; 16:266–73.
Article8. Potter R, Gnant M, Kwasny W, Tausch C, Handl-Zeller L, Pakisch B, et al. Lumpectomy plus tamoxifen or anastrozole with or without whole breast irradiation in women with favorable early breast cancer. Int J Radiat Oncol Biol Phys. 2007; 68:334–40.9. Bastiaannet E, Liefers GJ, de Craen AJ, Kuppen PJ, van de Water W, Portielje JE, et al. Breast cancer in elderly compared to younger patients in the Netherlands: stage at diagnosis, treatment and survival in 127,805 unselected patients. Breast Cancer Res Treat. 2010; 124:801–7.
Article10. Schonberg MA, Marcantonio ER, Li D, Silliman RA, Ngo L, McCarthy EP. Breast cancer among the oldest old: tumor characteristics, treatment choices, and survival. J Clin Oncol. 2010; 28:2038–45.
Article11. National Comprehensive Cancer Network Clnical Practice Guidelines in Oncology, Older Adult Oncology, (NCCN Guidelines Version 2.2017) [Internet]. Fort Washington, PA: National Comprehensive Cancer Network;2017. [cited 2018 May 4]. Available from: https://www.nccn.org/profession-als/physician_gls/pdf/senior.pdf.12. Biganzoli L, Wildiers H, Oakman C, Marotti L, Loibl S, Kunkler I, et al. Management of elderly patients with breast cancer: updated recommendations of the International Society of Geriatric Oncology (SIOG) and European Society of Breast Cancer Specialists (EUSOMA). Lancet Oncol. 2012; 13:e148–60.
Article13. Coates AS, Winer EP, Goldhirsch A, Gelber RD, Gnant M, Piccart-Gebhart M, et al. Tailoring therapies: improving the management of early breast cancer: St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2015. Ann Oncol. 2015; 26:1533–46.14. Yancik R, Wesley MN, Ries LA, Havlik RJ, Edwards BK, Yates JW. Effect of age and comorbidity in postmenopausal breast cancer patients aged 55 years and older. JAMA. 2001; 285:885–92.
Article15. Kim KS, Shin KH, Choi N, Lee SW. Hypofractionated whole breast irradiation: new standard in early breast cancer after breast-conserving surgery. Radiat Oncol J. 2016; 34:81–7.
Article16. Voduc KD, Cheang MC, Tyldesley S, Gelmon K, Nielsen TO, Kennecke H. Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol. 2010; 28:1684–91.
Article17. Dawood S, Hu R, Homes MD, Collins LC, Schnitt SJ, Connolly J, et al. Defining breast cancer prognosis based on molecular phenotypes: results from a large cohort study. Breast Cancer Res Treat. 2011; 126:185–92.
Article18. Early Breast Cancer Trialists' Collaborative Group (EBCTCG), Darby S, McGale P, Correa C, Taylor C, Arriagada R, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: metaanalysis of individual patient data for 10,801 women in 17 randomised trials. Lancet. 2011; 378:1707–16.19. DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, Jemal A. Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA Cancer J Clin. 2016; 66:31–42.
Article20. Nguyen PL, Taghian AG, Katz MS, Niemierko A, Abi Raad RF, Boon WL, et al. Breast cancer subtype approximated by estrogen receptor, progesterone receptor, and HER-2 is associated with local and distant recurrence after breast-conserving therapy. J Clin Oncol. 2008; 26:2373–8.
Article21. Haffty BG, Yang Q, Reiss M, Kearney T, Higgins SA, Weidhaas J, et al. Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol. 2006; 24:5652–7.
Article22. Sayan M, Wilson K, Nelson C, Gagne H, Rubin D, Heimann R. A novel schedule of accelerated partial breast radiation using intensity-modulated radiation therapy in elderly patients: survival and toxicity analysis of a prospective clinical trial. Radiat Oncol J. 2017; 35:32–8.
Article23. Rakha EA, Reis-Filho JS, Baehner F, Dabbs DJ, Decker T, Eusebi V, et al. Breast cancer prognostic classification in the molecular era: the role of histological grade. Breast Cancer Res. 2010; 12:207.
Article24. Giuliano AE, Connolly JL, Edge SB, Mittendorf EA, Rugo HS, Solin LJ, et al. Breast Cancer-Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017; 67:290–303.25. Vaz-Luis I, Ottesen RA, Hughes ME, Mamet R, Burstein HJ, Edge SB, et al. Outcomes by tumor subtype and treatment pattern in women with small, node-negative breast cancer: a multi-institutional study. J Clin Oncol. 2014; 32:2142–50.
Article26. Houvenaeghel G, Goncalves A, Classe JM, Garbay JR, Giard S, Charytensky H, et al. Characteristics and clinical outcome of T1 breast cancer: a multicenter retrospective cohort study. Ann Oncol. 2014; 25:623–8.
Article27. Kasangian AA, Moretti A, Biagioli E, Bernardin E, Cordovana A, Gherardi G, et al. Does tumor size in T1-T2 early breast cancer (EBC) still have a prognostic role? J Clin Oncol. 2017; 35 Suppl:Abstr e12087.
Article28. Fyles AW, McCready DR, Manchul LA, Trudeau ME, Merante P, Pintilie M, et al. Tamoxifen with or without breast irradiation in women 50 years of age or older with early breast cancer. N Engl J Med. 2004; 351:963–70.
Article29. Hepel JT, Wazer DE. Should a woman age 70 to 80 years receive radiation after breast-conserving surgery? J Clin Oncol. 2013; 31:2377–81.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Adjuvant Hormonal Therapy on the Development of Pulmonary Fibrosis after Postoperative Radiotherapy for Breast Cancer
- Evaluation of the Benefit of Radiotherapy in Patients with Occult Breast Cancer: A Population-Based Analysis of the SEER Database
- Hormone Treatment for Breast Cancer
- Hypofractionated Radiotherapy for Early-Stage Breast Cancer: A Propensity Score Matched Analysis
- Postoperative Radiotherapy Improves Survival in Gastric Signet-Ring Cell Carcinoma: a SEER Database Analysis