J Korean Soc Radiol.
2018 May;78(5):309-320. 10.3348/jksr.2018.78.5.309.
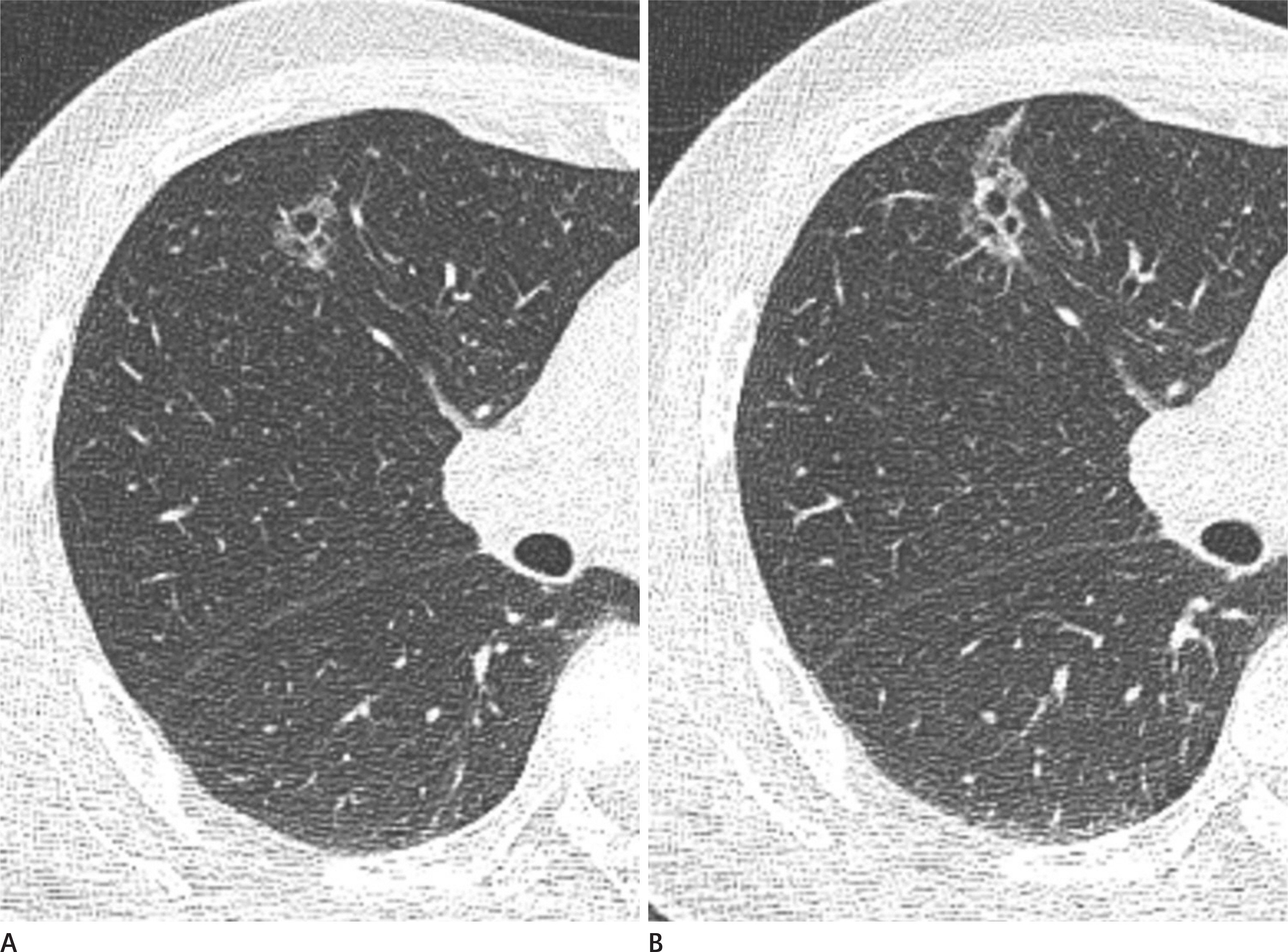
Pulmonary Subsolid Nodules: An Overview & Management Guidelines
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul, Korea. cmpark.morphius@gmail.com
- KMID: 2410720
- DOI: http://doi.org/10.3348/jksr.2018.78.5.309
Abstract
- Pulmonary subsolid nodules (SSNs) refer to the pulmonary pure ground-glass nodules and part-solid nodules. SSNs are frequently encountered in clinical settings, such as in screenings conducted with chest computed tomography. The main concern regarding pulmonary SSNs, particularly when they are persistent, has been a lung adenocarcinoma and the precursors to this condition. This review aims at describing the current understanding of the imaging features, histology, natural course, and to present the current management protocols based on the guidelines recently established by the Fleischner Society.
MeSH Terms
Figure
Reference
-
References
1. Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008; 246:697–722.
Article2. Naidich DP, Bankier AA, MacMahon H, Schaefer-Prokop CM, Pistolesi M, Goo JM, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013; 266:304–317.
Article3. MacMahon H, Naidich DP, Goo JM, Lee KS, Leung ANC, Mayo JR, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology. 2017; 284:228–243.4. Sone S, Takashima S, Li F, Yang Z, Honda T, Maruyama Y, et al. Mass screening for lung cancer with mobile spiral computed tomography scanner. Lancet. 1998; 351:1242–1245.
Article5. van Klaveren RJ, Oudkerk M, Prokop M, Scholten ET, Nackaerts K, Vernhout R, et al. Management of lung nodules detected by volume CT scanning. N Engl J Med. 2009; 361:2221–2229.
Article6. Yankelevitz DF, Yip R, Smith JP, Liang M, Liu Y, Xu DM, et al. CT screening for lung cancer: nonsolid nodules in baseline and annual repeat rounds. Radiology. 2015; 277:555–564.
Article7. Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, Miettinen OS. ELCAP Group. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol. 2002; 178:1053–1057.8. Godoy MC, Naidich DP. Overview and strategic management of subsolid pulmonary nodules. J Thorac Imaging. 2012; 27:240–248.
Article9. Felix L, Serra-Tosio G, Lantuejoul S, Timsit JF, Moro-Sibilot D, Brambilla C, et al. CT characteristics of resolving groundglass opacities in a lung cancer screening programme. Eur J Radiol. 2011; 77:410–416.
Article10. Oh JY, Kwon SY, Yoon HI, Lee SM, Yim JJ, Lee JH, et al. Clinical significance of a solitary groundglass opacity (GGO) lesion of the lung detected by chest CT. Lung Cancer. 2007; 55:67–73.
Article11. Lee SM, Park CM, Goo JM, Lee CH, Lee HJ, Kim KG, et al. Transient part-solid nodules detected at screening thin-section CT for lung cancer: comparison with persistent part-solid nodules. Radiology. 2010; 255:242–251.
Article12. Park CM, Goo JM, Lee HJ, Lee CH, Chun EJ, Im JG. Nodular groundglass opacity at thin-section CT: histologic correlation and evaluation of change at follow-up. Radiographics. 2007; 27:391–408.
Article13. Gandara DR, Aberle D, Lau D, Jett J, Akhurst T, Heelan R, et al. Radiographic imaging of bronchioloalveolar carcinoma: screening, patterns of presentation and response assessment. J Thorac Oncol. 2006; 1(9 Suppl):): S20-S26.
Article14. Park CM, Goo JM, Lee HJ, Lee CH, Chung DH, Chun EJ, et al. Focal interstitial fibrosis manifesting as nodular groundglass opacity: thin-section CT findings. Eur Radiol. 2007; 17:2325–2331.
Article15. Aoki T, Nakata H, Watanabe H, Nakamura K, Kasai T, Hashimoto H, et al. Evolution of peripheral lung adenocarcinomas: CT findings correlated with histology and tumor doubling time. AJR Am J Roentgenol. 2000; 174:763–768.16. Takashima S, Li F, Maruyama Y, Hasegawa M, Takayama F, Kadoya M, et al. Discrimination of subtypes of small adenocarcinoma in the lung with thin-section CT. Lung Cancer. 2002; 36:175–182.
Article17. Takashima S, Maruyama Y, Hasegawa M, Saito A, Haniuda M, Kadoya M. High-resolution CT features: prognostic significance in peripheral lung adenocarcinoma with bronchioloalveolar carcinoma components. Respiration. 2003; 70:36–42.
Article18. Noguchi M, Morikawa A, Kawasaki M, Matsuno Y, Yamada T, Hirohashi S, et al. Small adenocarcinoma of the lung. Histologic characteristics and prognosis. Cancer. 1995; 75:2844–2852.
Article19. Noguchi M, Shimosato Y. The development and progression of adenocarcinoma of the lung. Cancer Treat Res. 1995; 72:131–142.
Article20. Lee HY, Lee KS. Ground-glass opacity nodules: histopathology, imaging evaluation, and clinical implications. J Thorac Imaging. 2011; 26:106–118.21. Takashima S, Maruyama Y, Hasegawa M, Yamanda T, Honda T, Kadoya M, et al. CT findings and progression of small peripheral lung neoplasms having a replacement growth pattern. AJR Am J Roentgenol. 2003; 180:817–826.
Article22. Austin JH, Garg K, Aberle D, Yankelevitz D, Kuriyama K, Lee HJ, et al. Radiologic implications of the 2011 classification of adenocarcinoma of the lung. Radiology. 2013; 266:62–71.
Article23. Lee HJ, Goo JM, Lee CH, Park CM, Kim KG, Park EA, et al. Predictive CT findings of malignancy in groundglass nodules on thin-section chest CT: the effects on radiologist performance. Eur Radiol. 2009; 19:552–560.
Article24. Oda S, Awai K, Liu D, Nakaura T, Yanaga Y, Nomori H, et al. Ground-glass opacities on thin-section helical CT: differentiation between bronchioloalveolar carcinoma and atypical adenomatous hyperplasia. AJR Am J Roentgenol. 2008; 190:1363–1368.
Article25. Takahashi S, Tanaka N, Okimoto T, Tanaka T, Ueda K, Matsumoto T, et al. Long term follow-up for small pure groundglass nodules: implications of determining an optimum follow-up period and high-resolution CT findings to predict the growth of nodules. Jpn J Radiol. 2012; 30:206–217.
Article26. Lee SM, Park CM, Goo JM, Lee HJ, Wi JY, Kang CH. Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as groundglass nodules: differentiation by using CT features. Radiology. 2013; 268:265–273.
Article27. Kim HY, Shim YM, Lee KS, Han J, Yi CA, Kim YK. Persistent pulmonary nodular groundglass opacity at thin-section CT: histopathologic comparisons. Radiology. 2007; 245:267–275.
Article28. Takashima S, Sone S, Li F, Maruyama Y, Hasegawa M, Kadoya M. Indeterminate solitary pulmonary nodules revealed at population-based CT screening of the lung: using first follow-up diagnostic CT to differentiate benign and malignant lesions. AJR Am J Roentgenol. 2003; 180:1255–1263.29. Hasegawa M, Sone S, Takashima S, Li F, Yang ZG, Maruyama Y, et al. Growth rate of small lung cancers detected on mass CT screening. Br J Radiol. 2000; 73:1252–1259.
Article30. Song YS, Park CM, Park SJ, Lee SM, Jeon YK, Goo JM. Volume and mass doubling times of persistent pulmonary subsolid nodules detected in patients without known malignancy. Radiology. 2014; 273:276–284.
Article31. Oda S, Awai K, Murao K, Ozawa A, Utsunomiya D, Yanaga Y, et al. Volume-doubling time of pulmonary nodules with ground glass opacity at multidetector CT: assessment with computer-aided three-dimensional volumetry. Acad Radiol. 2011; 18:63–69.32. Chang B, Hwang JH, Choi YH, Chung MP, Kim H, Kwon OJ, et al. Natural history of pure groundglass opacity lung nodules detected by low-dose CT scan. Chest. 2013; 143:172–178.
Article33. Silva M, Sverzellati N, Manna C, Negrini G, Marchianò A, Zompatori M, et al. Long-term surveillance of groundglass nodules: evidence from the MILD trial. J Thorac Oncol. 2012; 7:1541–1546.34. Hiramatsu M, Inagaki T, Inagaki T, Matsui Y, Satoh Y, Okumura S, et al. Pulmonary groundglass opacity (GGO) lesion-slarge size and a history of lung cancer are risk factors for growth. J Thorac Oncol. 2008; 3:1245–1250.
Article35. Kodama K, Higashiyama M, Yokouchi H, Takami K, Kuriyama K, Kusunoki Y, et al. Natural history of pure groundglass opacity after longterm follow-up of more than 2 years. Ann Thorac Surg. 2002; 73:386–392. ; discussion 392–393.
Article36. Lee JH, Park CM, Lee SM, Kim H, McAdams HP, Goo JM. Persistent pulmonary subsolid nodules with solid portions of 5 mm or smaller: Their natural course and predictors of interval growth. Eur Radiol. 2016; 26:1529–1537.37. Kobayashi Y, Fukui T, Ito S, Usami N, Hatooka S, Yatabe Y, et al. How long should small lung lesions of groundglass opacity be followed? J Thorac Oncol. 2013; 8:309–314.
Article38. Lee JH, Park CM, Kim H, Hwang EJ, Park J, Goo JM. Persistent part-solid nodules with solid part of 5 mm or smaller: Can the ‘follow-up and surgical resection after interval growth'policy have a negative effect on patient prognosis? Eur Radiol. 2017; 27:195–202.39. Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M, et al. Prediction of pathologic node-negative clinical stage IA lung adenocarcinoma for optimal candidates undergoing sublobar resection. J Thorac Cardiovasc Surg. 2012; 144:1365–1371.
Article40. Tsutani Y, Miyata Y, Nakayama H, Okumura S, Adachi S, Yoshimura M, et al. Prognostic significance of using solid versus whole tumor size on high-resolution computed tomography for predicting pathologic malignant grade of tumors in clinical stage IA lung adenocarcinoma: a multicenter study. J Thorac Cardiovasc Surg. 2012; 143:607–612.
Article41. Murakawa T, Konoeda C, Ito T, Inoue Y, Sano A, Nagayama K, et al. The ground glass opacity component can be eliminated from the T-factor assessment of lung adenocarcinoma. Eur J Cardiothorac Surg. 2013; 43:925–932.
Article42. Tsutani Y, Miyata Y, Yamanaka T, Nakayama H, Okumura S, Adachi S, et al. Solid tumors versus mixed tumors with a groundglass opacity component in patients with clinical stage IA lung adenocarcinoma: prognostic comparison using high-resolution computed tomography findings. J Thorac Cardiovasc Surg. 2013; 1461:17–23.
Article43. Asamura H, Hishida T, Suzuki K, Koike T, Nakamura K, Kusumoto M, et al. Radiographically determined noninvasive adenocarcinoma of the lung: survival outcomes of Japan Clinical Oncology Group 0201. J Thorac Cardiovasc Surg. 2013; 146:24–30.
Article44. Suzuki K, Koike T, Asakawa T, Kusumoto M, Asamura H, Nagai K, et al. A prospective radiological study of thin-section computed tomography to predict pathological nonin-vasiveness in peripheral clinical IA lung cancer (Japan Clinical Oncology Group 0201). J Thorac Oncol. 2011; 6:751–756.
Article45. Aoki T, Tomoda Y, Watanabe H, Nakata H, Kasai T, Hashimoto H, et al. Peripheral lung adenocarcinoma: correlation of thin-section CT findings with histologic prognostic factors and survival. Radiology. 2001; 220:803–809.
Article46. Haraguchi N, Satoh H, Kikuchi N, Kagohashi K, Ishikawa H, Ohtsuka M. Prognostic value of tumor disappearance rate on computed tomography in advanced-stage lung adenocarcinoma. Clin Lung Cancer. 2007; 8:327–330.
Article47. Kakinuma R, Kodama K, Yamada K, Yokoyama A, Adachi S, Mori K, et al. Performance evaluation of 4 measuring methods of groundglass opacities for predicting the 5-year relapse-free survival of patients with peripheral nonsmall cell lung cancer: a multicenter study. J Comput Assist Tomogr. 2008; 32:792–798.48. Hwang EJ, Park CM, Ryu Y, Lee SM, Kim YT, Kim YW, et al. Pulmonary adenocarcinomas appearing as part-solid groundglass nodules: is measuring solid component size a better prognostic indicator? Eur Radiol. 2015; 25:558–567.
Article49. Hwang EJ, Park CM, Kim YT, Kim H, Goo JM. Microscopic invasions, prognoses, and recurrence patterns of stage I adenocarcinomas manifesting as part-solid groundglass nodules: comparison with adenocarcinomas appearing as solid nodules after matching their solid parts'size. Medicine (Baltimore). 2016; 95:e3419.50. Hoda SA. Book review: AJCC cancer staging manual, eighth edition. Adv Anat Pathol. 2017; 24:112.51. Kim TJ, Park CM, Goo JM, Lee KW. Is there a role for FDG PET in the management of lung cancer manifesting predominantly as groundglass opacity? AJR Am J Roentgenol. 2012; 198:83–88.
Article52. Lee SM, Park CM, Paeng JC, Im HJ, Goo JM, Lee HJ, et al. Accuracy and predictive features of FDG-PET/CT and CT for diagnosis of lymph node metastasis of T1 non-small-cell lung cancer manifesting as a subsolid nodule. Eur Radiol. 2012; 22:1556–1563.
Article53. Matsuguma H, Yokoi K, Anraku M, Kondo T, Kamiyama Y, Mori K, et al. Proportion of groundglass opacity on highres-olution computed tomography in clinical T1 N0 M0 adenocarcinoma of the lung: a predictor of lymph node metastasis. J Thorac Cardiovasc Surg. 2002; 124:278–284.
Article54. Hur J, Lee HJ, Nam JE, Kim YJ, Kim TH, Choe KO, et al. Diagnostic accuracy of CT fluoroscopy-guided needle aspiration biopsy of groundglass opacity pulmonary lesions. AJR Am J Roentgenol. 2009; 192:629–634.
Article55. Yamagami T, Yoshimatsu R, Miura H, Yamada K, Takahata A, Matsumoto T, et al. Diagnostic performance of percutaneous lung biopsy using automated biopsy needles under CT-fluoroscopic guidance for groundglass opacity lesions. Br J Radiol. 2013; 86:20120447.
Article56. Shimizu K, Ikeda N, Tsuboi M, Hirano T, Kato H. Percutaneous CT-guided fine needle aspiration for lung cancer smaller than 2 cm and revealed by groundglass opacity at CT. Lung Cancer. 2006; 51:173–179.57. Kim TJ, Lee JH, Lee CT, Jheon SH, Sung SW, Chung JH, et al. Diagnostic accuracy of CT-guided core biopsy of groundglass opacity pulmonary lesions. AJR Am J Roentgenol. 2008; 190:234–239.
Article58. Lu CH, Hsiao CH, Chang YC, Lee JM, Shih JY, Wu LA, et al. Percutaneous computed tomography-guided coaxial core biopsy for small pulmonary lesions with groundglass attenuation. J Thorac Oncol. 2012; 7:143–150.
Article59. Lee SM, Park CM, Song YS, Kim H, Kim YT, Park YS, et al. CT assessment-based direct surgical resection of part-solid nodules with solid component larger than 5 mm without preoperative biopsy: experience at a single tertiary hospital. Eur Radiol. 2017; 27:5119–5126.60. Lee SM, Park CM, Lee KH, Bahn YE, Kim JI, Goo JM. C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of lung nodules: clinical experience in 1108 patients. Radiology. 2014; 271:291–300.
Article61. Choi JW, Park CM, Goo JM, Park YK, Sung W, Lee HJ, et al. C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of small (≤20 mm) lung nodules: diagnostic accuracy and complications in 161 patients. AJR Am J Roentgenol. 2012; 199:W322–W330.62. Goo JM, Park CM, Lee HJ. Ground-glass nodules on chest CT as imaging biomarkers in the management of lung adenocarcinoma. AJR Am J Roentgenol. 2011; 196:533–543.
Article63. Erasmus JJ, Connolly JE, McAdams HP, Roggli VL. Solitary pulmonary nodules: part I. morphologic evaluation for differentiation of benign and malignant lesions. Radiographics. 2000; 20:43–58.
Article64. Travis WD, Asamura H, Bankier AA, Beasley MB, Detterbeck F, Flieder DB, et al. The IASLC lung cancer staging project: proposals for coding t categories for subsolid nodules and assessment of tumor size in part-solid tumors in the forthcoming eighth edition of the TNM classification of lung cancer. J Thorac Oncol. 2016; 11:1204–1223.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Pulmonary Malignant Melanoma Presenting as Bilateral Multiple Subsolid Nodules: A Case Report
- Semi-Quantitative Analysis for Determining the Optimal Threshold Value on CT to Measure the Solid Portion of Pulmonary Subsolid Nodules
- The Effect of Lung Volume on the Size and Volume of Pulmonary Subsolid Nodules on CT: Intraindividual Comparison between Total Lung Capacity and Tidal Volume
- A Case of Benign Multiple Pulmonary Nodules in a Patient with Osteosarcoma
- Updated guidelines for the diagnosis and management of thyroid nodules