Brain Tumor Res Treat.
2018 Apr;6(1):43-46. 10.14791/btrt.2018.6.e7.
Extensive Pituitary Apoplexy after Chemotherapy in a Patient with Metastatic Breast Cancer
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Pathology, National Cancer Center, Graduate School of Cancer Science and Policy, Goyang, Korea.
- 3Department of Cancer Control, National Cancer Center, Graduate School of Cancer Science and Policy, Goyang, Korea. nsghs@ncc.re.kr
- KMID: 2410237
- DOI: http://doi.org/10.14791/btrt.2018.6.e7
Abstract
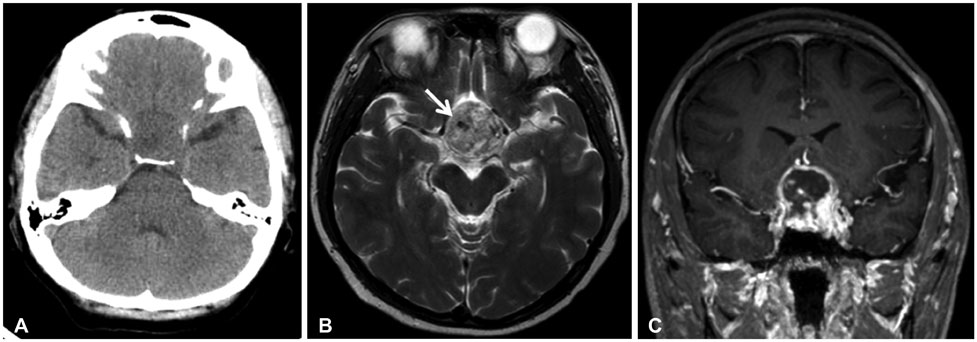
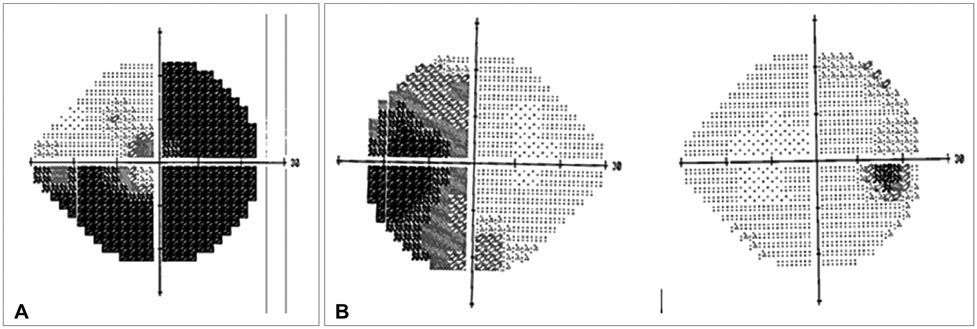
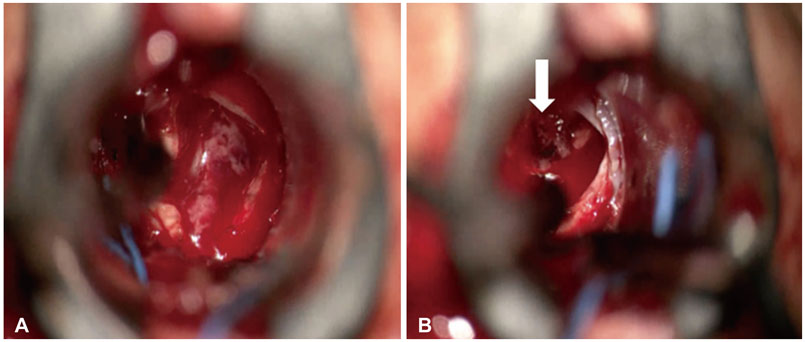
- Surgery, anticoagulation therapy, pregnancy, and hormone treatments, such as bromocriptine, are well-characterized precipitating factors for pituitary apoplexy. However, whether cytotoxic chemotherapy for systemic cancer could cause pituitary apoplexy has not been investigated. Here, we present a case of a 41-year-old woman who developed a severe headache with decreased visual acuity after intravenous cytotoxic chemotherapy to treat metastatic breast cancer. Preoperative neuroimaging revealed pituitary adenoma with necrosis. Operative findings and pathologic examination concluded extensive necrosis with a small intratumoral hemorrhage in a pre-existing pituitary adenoma. We reviewed two additional previously published cases of pituitary apoplexy after systemic chemotherapy and suggest that cytotoxic chemotherapy may induce pituitary apoplexy.
MeSH Terms
Figure
Reference
-
1. Semple PL, Jane JA Jr, Laws ER Jr. Clinical relevance of precipitating factors in pituitary apoplexy. Neurosurgery. 2007; 61:956–961.
Article2. Guerrero-Pérez F, Marengo AP, Planas-Vilaseca A, Flores-Escobar V, Villabona-Artero C. Pituitary apoplexy induced by triptorelin in patient with prostate cancer. Endocrinol Nutr. 2015; 62:411–412.
Article3. Chng E, Dalan R. Pituitary apoplexy associated with cabergoline therapy. J Clin Neurosci. 2013; 20:1637–1643.
Article4. Silberstein L, Johnston C, Bhagat A, Tibi L, Harrison J. Pituitary apoplexy during induction chemotherapy for acute myeloid leukaemia. Br J Haematol. 2008; 143:151.
Article5. Davies JS, Rees DA, Evans LM, Scanlon MF. Pituitary apoplexy following combination chemotherapy-a case report. Endocr Relat Cancer. 1998; 5:151–153.6. Biousse V, Newman NJ, Oyesiku NM. Precipitating factors in pituitary apoplexy. J Neurol Neurosurg Psychiatry. 2001; 71:542–545.
Article