Korean Circ J.
2018 Mar;48(3):209-216. 10.4070/kcj.2017.0166.
Array Comparative Genomic Hybridization as the First-line Investigation for Neonates with Congenital Heart Disease: Experience in a Single Tertiary Center
- Affiliations
-
- 1Department of Pediatrics, Kyungpook National University Children's Hospital, Kyungpook National University School of Medicine, Daegu, Korea. kimyhmd@knu.ac.kr
- KMID: 2406924
- DOI: http://doi.org/10.4070/kcj.2017.0166
Abstract
- BACKGROUND AND OBJECTIVES
The purpose of the present study was to investigate the advantages and disadvantages of verifying genetic abnormalities using array comparative genomic hybridization (a-CGH) immediately after diagnosis of congenital heart disease (CHD).
METHODS
Among neonates under the age of 28 days who underwent echocardiography from January 1, 2014 to April 30, 2016, neonates whose chromosomal and genomic abnormalities were tested using a-CGH in cases of an abnormal finding on echocardiography were enrolled.
RESULTS
Of the 166 patients diagnosed with CHD, 81 underwent a-CGH and 11 patients (11/81, 13.5%) had abnormal findings on a-CGH. 22q11.2 deletion syndrome was the most common (4/11, 36.4%). On the first a-CGH, 4 patients were negative (4/81, 5%). Three of them were finally diagnosed with Williams syndrome using fluorescent in situ hybridization (FISH), 1 patient was diagnosed with Noonan syndrome through exome sequencing. All of them exhibited diffuse pulmonary artery branch hypoplasia, as well as increased velocity of blood flow, on repeated echocardiography. Five patients started rehabilitation therapy at mean 6 months old age in outpatient clinics and epilepsy was diagnosed in 2 patients. Parents of 2 patients (22q11.2 deletion syndrome and Patau syndrome) refused treatment due to the anticipated prognosis.
CONCLUSIONS
Screening tests for genetic abnormalities using a-CGH in neonates with CHD has the advantage of early diagnosis of genetic abnormality during the neonatal period in which there is no obvious symptom of genetic abnormality. However, there are disadvantages that some genetic abnormalities cannot be identified on a-CGH.
MeSH Terms
-
Ambulatory Care Facilities
Comparative Genomic Hybridization*
Diagnosis
DiGeorge Syndrome
Early Diagnosis
Echocardiography
Epilepsy
Exome
Heart Defects, Congenital*
Humans
In Situ Hybridization, Fluorescence
Infant, Newborn*
Mass Screening
Noonan Syndrome
Parents
Prognosis
Pulmonary Artery
Rehabilitation
Williams Syndrome
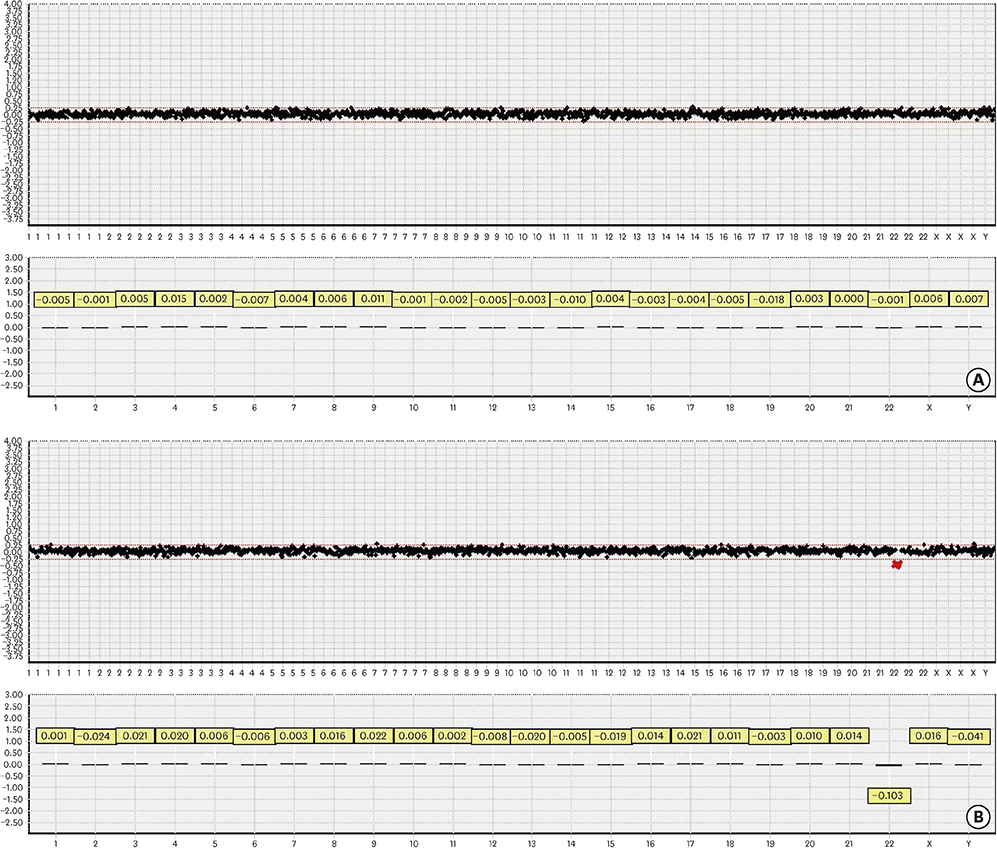
Figure
Cited by 1 articles
-
Chromosomal Microarray: Application for Congenital Heart Diseases
Jung Min Ko
Korean Circ J. 2018;48(3):233-235. doi: 10.4070/kcj.2018.0032.
Reference
-
1. Nora JJ. Multifactorial inheritance hypothesis for the etiology of congenital heart diseases. The genetic-environmental interaction. Circulation. 1968; 38:604–617.2. Pediatric Cardiac Genomics Consortium. The Congenital Heart Disease Genetic Network Study: rationale, design, and early results. Circ Res. 2013; 112:698–706.3. Pierpont ME, Basson CT, Benson DW Jr, et al. Genetic basis for congenital heart defects: current knowledge: a scientific statement from the American Heart Association Congenital Cardiac Defects Committee, Council on Cardiovascular Disease in the Young: endorsed by the American Academy of Pediatrics. Circulation. 2007; 115:3015–3038.4. Park SJ, Jung EH, Ryu RS, Kang HW, Chung HD, Kang HY. The clinical application of array CGH for the detection of chromosomal defects in 20,126 unselected newborns. Mol Cytogenet. 2013; 6:21.
Article5. van Trier DC, Feenstra I, Bot P, de Leeuw N, Draaisma JM. Cardiac anomalies in individuals with the 18q deletion syndrome; report of a child with Ebstein anomaly and review of the literature. Eur J Med Genet. 2013; 56:426–431.
Article6. Anderlid BM, Schoumans J, Annerén G, et al. Subtelomeric rearrangements detected in patients with idiopathic mental retardation. Am J Med Genet. 2002; 107:275–284.
Article7. Committee on Genetics. American Academy of Pediatrics: health care supervision for children with Williams syndrome. Pediatrics. 2001; 107:1192–1204.8. van der Burgt I. Noonan syndrome. Orphanet J Rare Dis. 2007; 2:4.
Article9. Roberts AE, Allanson JE, Tartaglia M, Gelb BD. Noonan syndrome. Lancet. 2013; 381:333–342.
Article10. Lee BH, Kim JM, Jin HY, Kim GH, Choi JH, Yoo HW. Spectrum of mutations in Noonan syndrome and their correlation with phenotypes. J Pediatr. 2011; 159:1029–1035.
Article11. Ko JM, Kim JM, Kim GH, Yoo HW. PTPN11, SOS1, KRAS, and RAF1 gene analysis, and genotype-phenotype correlation in Korean patients with Noonan syndrome. J Hum Genet. 2008; 53:999–1006.
Article12. Egbe A, Lee S, Ho D, Uppu S, Srivastava S. Prevalence of congenital anomalies in newborns with congenital heart disease diagnosis. Ann Pediatr Cardiol. 2014; 7:86–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status and Future Clinical Applications of Array.based Comparative Genomic Hybridization
- Array-based Comparative Genomic Hybridization and Its Application to Cancer Genomes and Human Genetics
- Next generation sequencing and array-based comparative genomic hybridization for molecular diagnosis of pediatric endocrine disorders
- Analysis of Chromosomal Aberrations in Lung Cancer Cell Line, NCI-H1373
- RAN-aCGH: R GUI Tools for Analysis and Visualization of an Array-CGH Experiment