Clin Orthop Surg.
2018 Mar;10(1):94-98. 10.4055/cios.2018.10.1.94.
Origin of Satellite Ganglion Cysts with Effusion in the Flexor Hallucis Longus Tendon Sheath around the Hallux
- Affiliations
-
- 1Division of Orthopaedic Surgery, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Orthopaedic Surgery, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. ykang77@daum.net
- 3Department of Diagnostic Radiology, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 4Department of Orthopaedic Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2405488
- DOI: http://doi.org/10.4055/cios.2018.10.1.94
Abstract
- BACKGROUND
To describe the clinical and magnetic resonance imaging findings of ganglion cysts with effusion in the flexor hallucis longus tendon sheath around the hallux to evaluate their origin.
METHODS
Patients with recurrent or painful ganglion cysts around the hallux with effusion in the flexor hallucis longus tendon sheath who underwent surgical treatment at St. Vincent's Hospital from February 2007 to August 2016 were investigated. Surgical indication was a painful or recurrent mass caused by the cystic lesions. Those without effusion of the flexor hallucis longus tendon sheath were excluded. We assessed the clinical and magnetic resonance imaging findings.
RESULTS
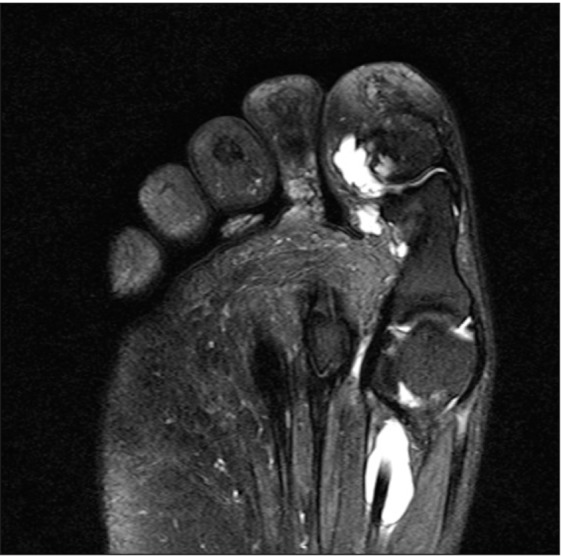
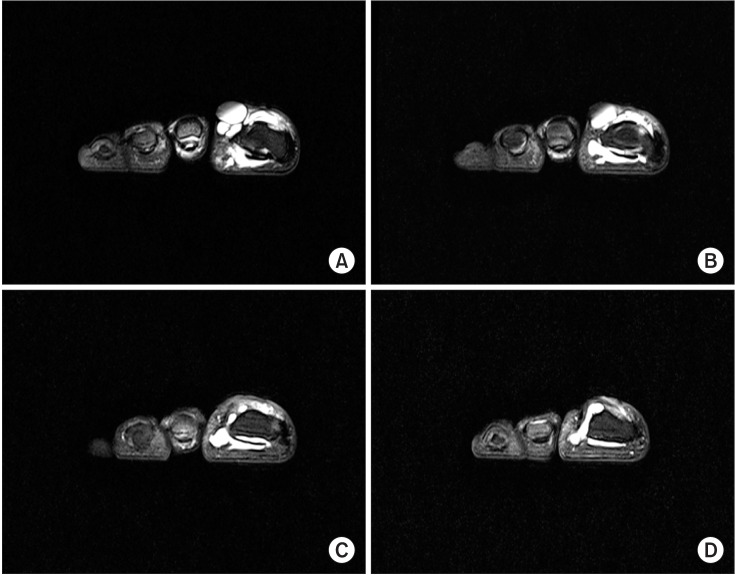
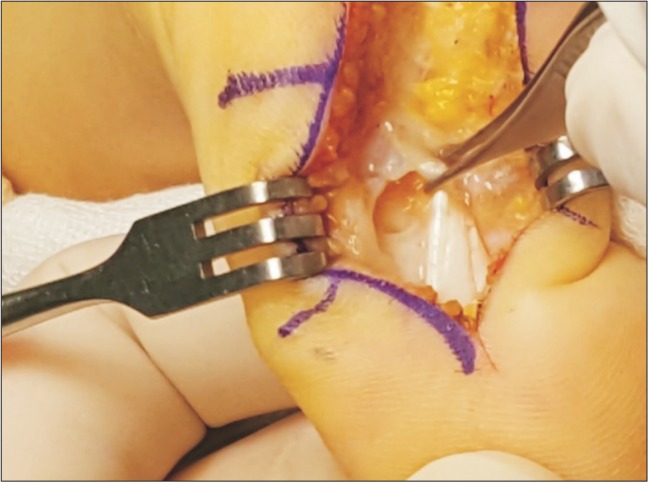
Magnetic resonance imaging findings in all patients showed several ganglion cysts around the hallux and large fluid accumulations within the flexor hallucis longus tendon sheath. Regarding the location, six ganglion cysts were on the dorsomedial aspect, one on the plantar medial aspect, seven on the plantar lateral aspect, and one in the toe pulp. Ten patients showed joint effusions in both the metatarsophalangeal and interphalangeal joints, two in the metatarsophalangeal joints, and three in the interphalangeal joints. There were communication stalks with a tail shape or abutment between ganglion cysts with surrounding joint effusions. Intraoperatively, connections between ganglion cysts, the synovial cyst of the flexor hallucis longus tendon sheath, and surrounding joints were seen.
CONCLUSIONS
Synovial fluid accumulation in the metatarsophalangeal or interphalangeal joint supplies the synovial cyst of the flexor hallucis longus tendon sheath and subsequently ganglion cysts in the hallux. In clinical practice, the surgeon should carefully check surrounding joints with tendon sheaths to prevent recurrence of the ganglion cysts around the hallux.
Keyword
MeSH Terms
Figure
Reference
-
1. Angelides AC, Wallace PF. The dorsal ganglion of the wrist: its pathogenesis, gross and microscopic anatomy, and surgical treatment. J Hand Surg Am. 1976; 1(3):228–235. PMID: 1018091.
Article2. Kirby EJ, Shereff MJ, Lewis MM. Soft-tissue tumors and tumor-like lesions of the foot: an analysis of eighty-three cases. J Bone Joint Surg Am. 1989; 71(4):621–626. PMID: 2703521.
Article3. Macdonald DJ, Holt G, Vass K, Marsh A, Kumar CS. The differential diagnosis of foot lumps: 101 cases treated surgically in North Glasgow over 4 years. Ann R Coll Surg Engl. 2007; 89(3):272–275. PMID: 17394713.
Article4. Weishaupt D, Schweitzer ME, Morrison WB, Haims AH, Wapner K, Kahn M. MRI of the foot and ankle: prevalence and distribution of occult and palpable ganglia. J Magn Reson Imaging. 2001; 14(4):464–471. PMID: 11599072.
Article5. Tanaka Y, Takakura Y, Kumai T, Sugimoto K, Taniguchi A, Hattori K. Sclerotherapy for intractable ganglion cyst of the hallux. Foot Ankle Int. 2009; 30(2):128–132. PMID: 19254507.
Article6. Kliman ME, Freiberg A. Ganglia of the foot and ankle. Foot Ankle. 1982; 3(1):45–46. PMID: 7129269.
Article7. Suen M, Fung B, Lung CP. Treatment of ganglion cysts. ISRN Orthop. 2013; 2013:940615. PMID: 24967120.
Article8. Pontious J, Good J, Maxian SH. Ganglions of the foot and ankle: a retrospective analysis of 63 procedures. J Am Podiatr Med Assoc. 1999; 89(4):163–168. PMID: 10220985.
Article9. Barrett C, Weaver TD, Schaffer SG. Ganglion cyst of the hallux: an aberrant presentation. J Foot Ankle Surg. 1995; 34(1):57–60. PMID: 7780394.
Article10. Nishikawa S, Toh S. Arthroscopic treatment of a ganglion of the first metatarsophalangeal joint. Arthroscopy. 2004; 20(1):69–72. PMID: 14716282.
Article11. Shimozono Y, Takao M, Miyamoto W, Yasui Y, Kawano H. Endoscopic treatment for intratendinous ganglion of the flexor hallucis longus tendon. J Orthop Sci. 2018; 23(1):190–193. PMID: 27329410.
Article12. Talawadekar GD, Damodaran P, Jain SA. Hourglass ganglion cyst of the foot: a case report. J Foot Ankle Surg. 2010; 49(5):489.e11–489.e12.
Article13. Tuncer S, Aydin A, Hocaoglu E. Ganglia of the hallux. Foot Ankle Surg. 2004; 10(2):97–99.
Article14. Wenig JA, McCarthy DJ. Synovial cyst of the hallux: a case report. J Am Podiatr Med Assoc. 1986; 76(1):7–12. PMID: 3941377.
Article15. Kawakatsu M, Ishiko T, Sumiya M. Tarsal tunnel syndrome due to three different types of ganglion during a 12-year period: a case report. J Foot Ankle Surg. 2017; 56(2):379–384. PMID: 28073652.
Article16. Kiehn MW, Gutowski KA. A recurrent foot ganglion managed with extensor digitorum brevis muscle flap coverage. J Foot Ankle Surg. 2004; 43(6):423–425. PMID: 15605057.
Article17. Rozbruch SR, Chang V, Bohne WH, Deland JT. Ganglion cysts of the lower extremity: an analysis of 54 cases and review of the literature. Orthopedics. 1998; 21(2):141–148. PMID: 9507266.
Article18. Lui TH. Arthroscopic ganglionectomy of the foot and ankle. Knee Surg Sports Traumatol Arthrosc. 2014; 22(7):1693–1700. PMID: 22648747.
Article19. Ahn JH, Choy WS, Kim HY. Operative treatment for ganglion cysts of the foot and ankle. J Foot Ankle Surg. 2010; 49(5):442–445. PMID: 20650661.
Article20. Blitz NM, Amrami KK, Spinner RJ. Magnetic resonance imaging of a deep peroneal intraneural ganglion cyst originating from the second metatarsophalangeal joint: a pattern of propagation supporting the unified articular (synovial) theory for the formation of intraneural ganglia. J Foot Ankle Surg. 2009; 48(1):80–84. PMID: 19110165.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trigger Toe in Soccer Player: A Case Report
- Reconstruction of Chronic Extensor Hallucis Longus Tendon Rupture Using Interposed Scar Tissue: A Case Report
- Synoivial Chondromatosis of the Ankle Joint and Flexor Hallucis Longus Tendon Sheath
- Minimally Invasive Surgery with Tenorrhaphy for Postoperative Hallux Varus Deformity Combined with Flexor Hallucis Longus Rupture after Hallux Valgus Correction: A Case Report
- Management of Checkrein Deformity