J Breast Cancer.
2011 Sep;14(3):204-212.
The Prognostic Significance of the Lymph Node Ratio in Axillary Lymph Node Positive Breast Cancer
- Affiliations
-
- 1Department of Radiation Oncology, The Catholic University of Korea College of Medicine, Seoul, Korea. sumic@catholic.ac.kr
- 2Department of General Surgery, The Catholic University of Korea College of Medicine, Seoul, Korea.
Abstract
- PURPOSE
This study evaluated the prognostic impact of the lymph node ratio (LNR; i.e., the ratio of positive to dissected lymph nodes) on recurrence and survival in breast cancer patients with positive axillary lymph nodes (LNs).
METHODS
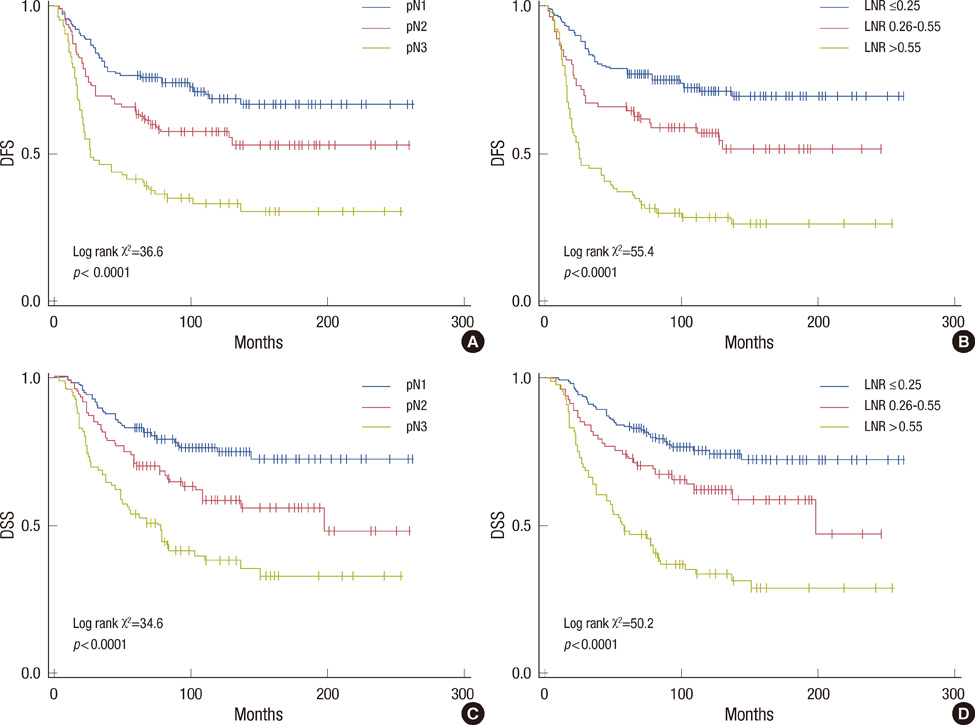
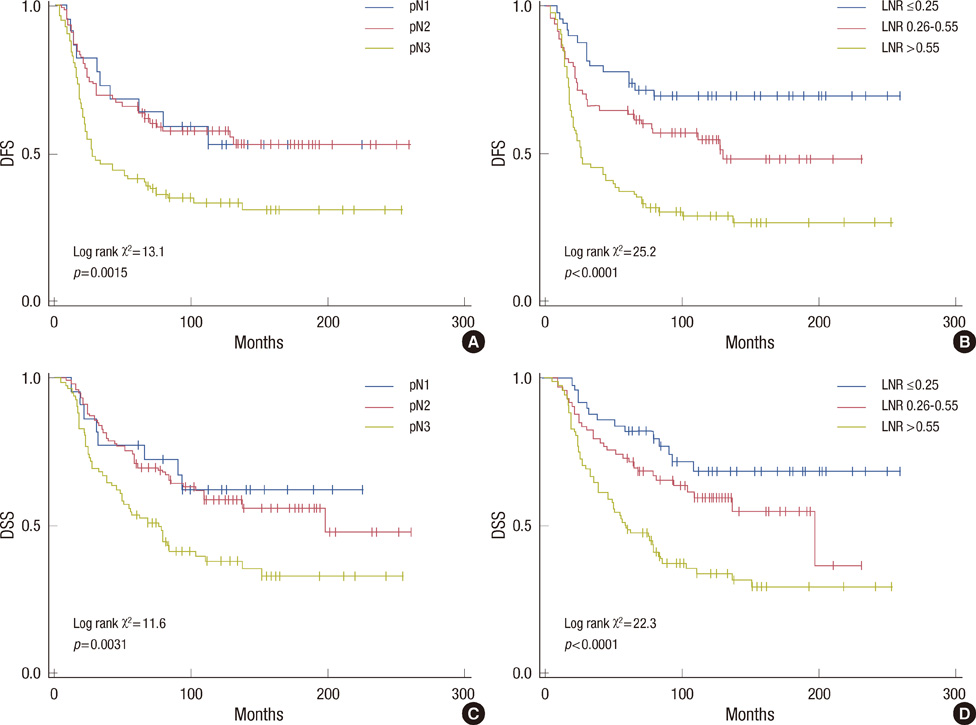
The study cohort was comprised of 330 breast cancer patients with positive axillary nodes who received postoperative radiotherapy between 1987 and 2004. Ten-year Kaplan-Meier locoregional failure, distant metastasis, disease-free survival (DFS) and disease-specific survival (DSS) rates were compared using Kaplan-Meier curves. The prognostic significance of the LNR was evaluated by multivariate analysis.
RESULTS
Median follow-up was 7.5 years. By minimum p-value approach, 0.25 and 0.55 were the cutoff values of LNR at which most significant difference in DFS and DSS was observed. The DFS and DSS rates correlated significantly with tumor size, pN classification, LNR, histologic grade, lymphovascular invasion, the status of estrogen receptor and progesterone receptor. The LNR based classification yielded a statistically larger separation of the DFS curves than pN classification. In multivariate analysis, histologic grade and pN classification were significant prognostic factors for DFS and DSS. However, when the LNR was included as a covariate in the model, the LNR was highly significant (p<0.0001), and pN classification was not statistically significant (p>0.05).
CONCLUSION
The LNR predicts recurrence and survival more accurately than pN classification in our study. The pN classification and LNR should be considered together in risk estimates for axillary LNs positive breast cancer patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Jatoi I, Hilsenbeck SG, Clark GM, Osborne CK. Significance of axillary lymph node metastasis in primary breast cancer. J Clin Oncol. 1999. 17:2334–2340.
Article2. Wilking N, Rutqvist LE, Carstensen J, Mattsson A, Skoog L. Stockholm Breast Cancer Study Group. Prognostic significance of axillary nodal status in primary breast cancer in relation to the number of resected nodes. Acta Oncol. 1992. 31:29–35.
Article3. Schaapveld M, Otter R, de Vries EG, Fidler V, Grond JA, van der Graaf WT, et al. Variability in axillary lymph node dissection for breast cancer. J Surg Oncol. 2004. 87:4–12.
Article4. Voordeckers M, Vinh-Hung V, Van de Steene J, Lamote J, Storme G. The lymph node ratio as prognostic factor in node-positive breast cancer. Radiother Oncol. 2004. 70:225–230.
Article5. Woodward WA, Vinh-Hung V, Ueno NT, Cheng YC, Royce M, Tai P, et al. Prognostic value of nodal ratios in node-positive breast cancer. J Clin Oncol. 2006. 24:2910–2916.
Article6. Vinh-Hung V, Verkooijen HM, Fioretta G, Neyroud-Caspar I, Rapiti E, Vlastos G, et al. Lymph node ratio as an alternative to pN staging in node-positive breast cancer. J Clin Oncol. 2009. 27:1062–1068.
Article7. van der Wal BC, Butzelaar RM, van der Meij S, Boermeester MA. Axillary lymph node ratio and total number of removed lymph nodes: predictors of survival in stage I and II breast cancer. Eur J Surg Oncol. 2002. 28:481–489.
Article8. Kuru B. Prognostic significance of total number of nodes removed, negative nodes removed, and ratio of positive nodes to removed nodes in node positive breast carcinoma. Eur J Surg Oncol. 2006. 32:1082–1088.
Article9. Lale Atahan I, Yildiz F, Ozyigit G, Sari S, Gurkaynak M, Selek U, et al. Percent positive axillary lymph node metastasis predicts survival in patients with non-metastatic breast cancer. Acta Oncol. 2008. 47:232–238.
Article10. Kim JY, Lim HI, Lee SK, Choi JH, Kim WW, Choe JH, et al. The impact of the ratio of positive nodes to removed nodes on recurrence and overall survival in node positive breast cancer patients. J Breast Cancer. 2008. 11:194–200.
Article11. Grills IS, Kestin LL, Goldstein N, Mitchell C, Martinez A, Ingold J, et al. Risk factors for regional nodal failure after breast-conserving therapy: regional nodal irradiation reduces rate of axillary failure in patients with four or more positive lymph nodes. Int J Radiat Oncol Biol Phys. 2003. 56:658–670.
Article12. Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, et al. AJCC Cancer Staging Manual. 2002. 6th ed. New York: Springer;223–236.13. Veronesi U, Rilke F, Luini A, Sacchini V, Galimberti V, Campa T, et al. Distribution of axillary node metastases by level of invasion. An analysis of 539 cases. Cancer. 1987. 59:682–687.
Article14. Kiricuta CI, Tausch J. A mathematical model of axillary lymph node involvement based on 1446 complete axillary dissections in patients with breast carcinoma. Cancer. 1992. 69:2496–2501.
Article15. Kuru B, Bozgul M. The impact of axillary lymph nodes removed in staging of node-positive breast carcinoma. Int J Radiat Oncol Biol Phys. 2006. 66:1328–1334.
Article16. Hack TF, Cohen L, Katz J, Robson LS, Goss P. Physical and psychological morbidity after axillary lymph node dissection for breast cancer. J Clin Oncol. 1999. 17:143–149.
Article17. Forrest AP, Everington D, McDonald CC, Steele RJ, Chetty U, Stewart HJ. The Edinburgh randomized trial of axillary sampling or clearance after mastectomy. Br J Surg. 1995. 82:1504–1508.
Article18. Lambah A, Dixon JM, Prescott RJ, Jack W, Forrest AP, Rodger A, et al. Randomised study of axillary clearance versus four node sampling. Eur J Cancer. 2001. 37:Suppl 5. 2.
Article19. Chetty U, Jack W, Prescott RJ, Tyler C, Rodger A. Management of the axilla in operable breast cancer treated by breast conservation: a randomized clinical trial. Edinburgh Breast Unit. Br J Surg. 2000. 87:163–169.
Article20. Krag DN, Weaver DL, Alex JC, Fairbank JT. Surgical resection and radiolocalization of the sentinel lymph node in breast cancer using a gamma probe. Surg Oncol. 1993. 2:335–339.
Article21. Greenstein AJ, Litle VR, Swanson SJ, Divino CM, Packer S, Wisnivesky JP. Prognostic significance of the number of lymph node metastases in esophageal cancer. J Am Coll Surg. 2008. 206:239–246.
Article22. De Ridder M, Vinh-Hung V, Van Nieuwenhove Y, Hoorens A, Sermeus A, Storme G. Prognostic value of the lymph node ratio in node positive colon cancer. Gut. 2006. 55:1681.
Article23. Chan JK, Kapp DS, Cheung MK, Osann K, Shin JY, Cohn D, et al. The impact of the absolute number and ratio of positive lymph nodes on survival of endometrioid uterine cancer patients. Br J Cancer. 2007. 97:605–611.
Article24. Farshid G, Pradhan M, Kollias J, Gill PG. A decision aid for predicting non-sentinel node involvement in women with breast cancer and at least one positive sentinel node. Breast. 2004. 13:494–501.
Article25. Barranger E, Coutant C, Flahault A, Delpech Y, Darai E, Uzan S. An axilla scoring system to predict non-sentinel lymph node status in breast cancer patients with sentinel lymph node involvement. Breast Cancer Res Treat. 2005. 91:113–119.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- Quadrantectomy and axillary lymph node dissection on breast cancer
- The Number of Removed Lymph Nodes for an Acceptable False Negative Rate in Sentinel Lymph Node Biopsy for Breast Cancer
- Incidence of Axillary Lymph Node Metastases in T1 Breast Cancer
- The Significance of Micrometastasis in Axillary Lymph Node Negative Breast Cancer