J Korean Ophthalmol Soc.
2017 Oct;58(10):1183-1188. 10.3341/jkos.2017.58.10.1183.
A Case of Surgical Diagnosis and Treatment of Idiopathic Orbital Myositis with Sudden Vision Loss
- Affiliations
-
- 1Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. oculoplasty@gmail.com
- 2T2B Infrastructure Center for Ocular Disease, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2393171
- DOI: http://doi.org/10.3341/jkos.2017.58.10.1183
Abstract
- PURPOSE
We report a case of idiopathic orbital myositis with sudden onset of unilateral visual loss and hypertrophy of the lateral rectus muscle at the apex of the orbit that was diagnosed using orbital biopsy and treated with intravenous corticosteroids.
CASE SUMMARY
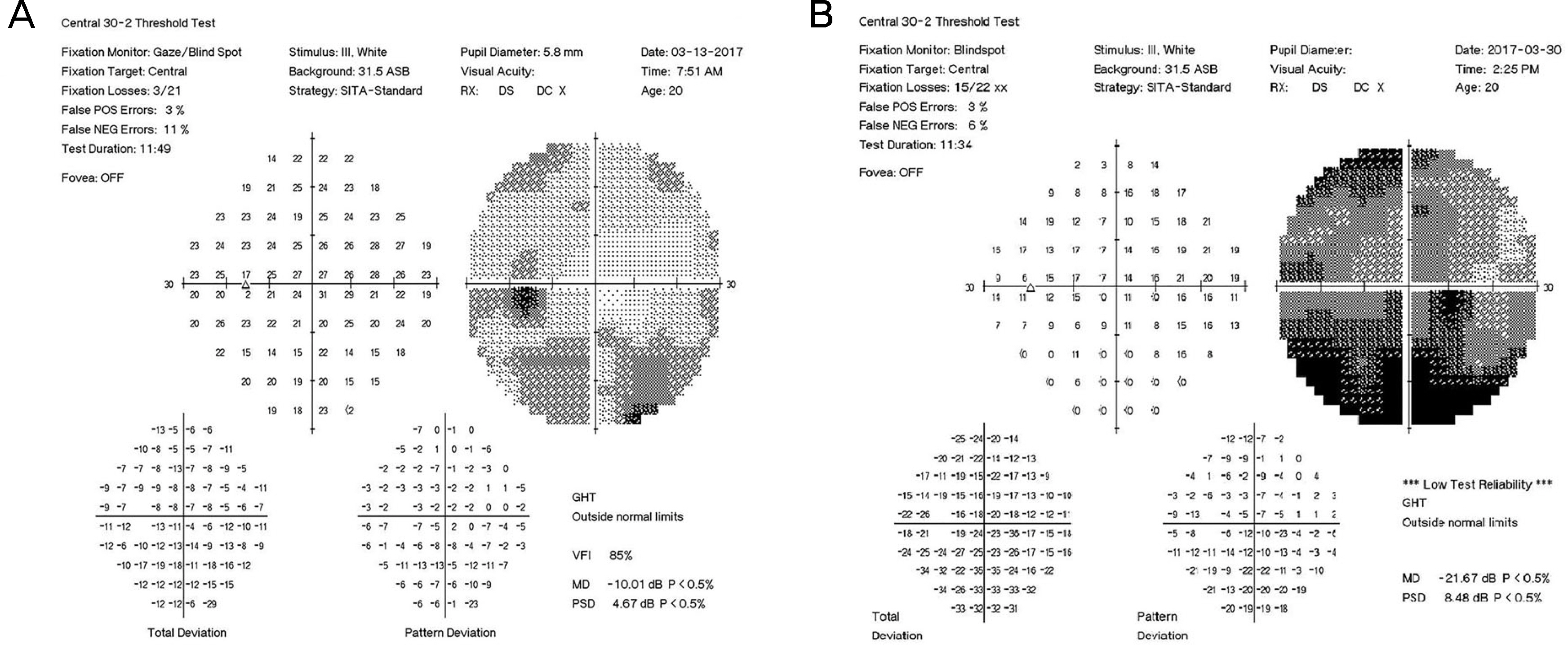
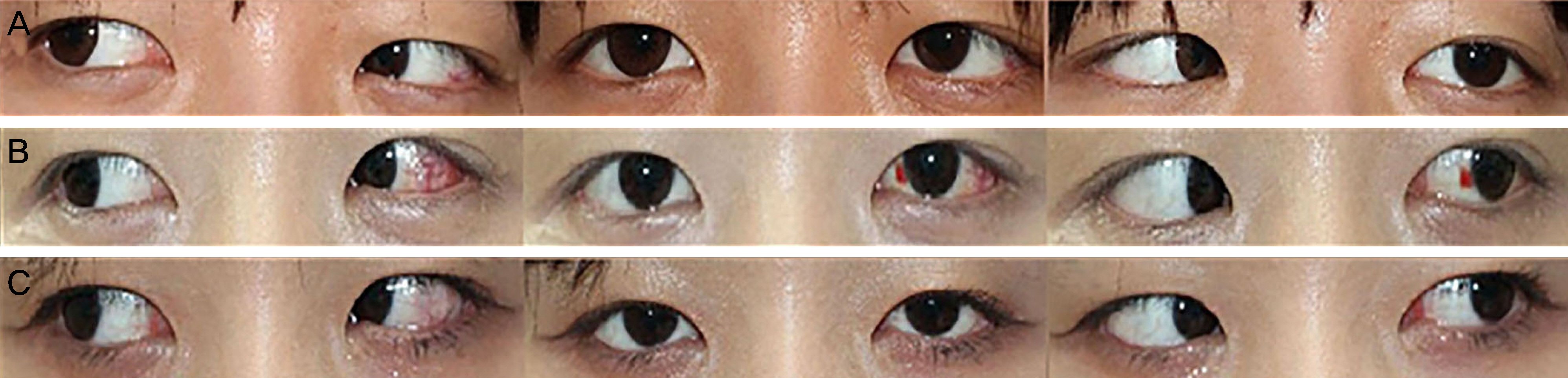
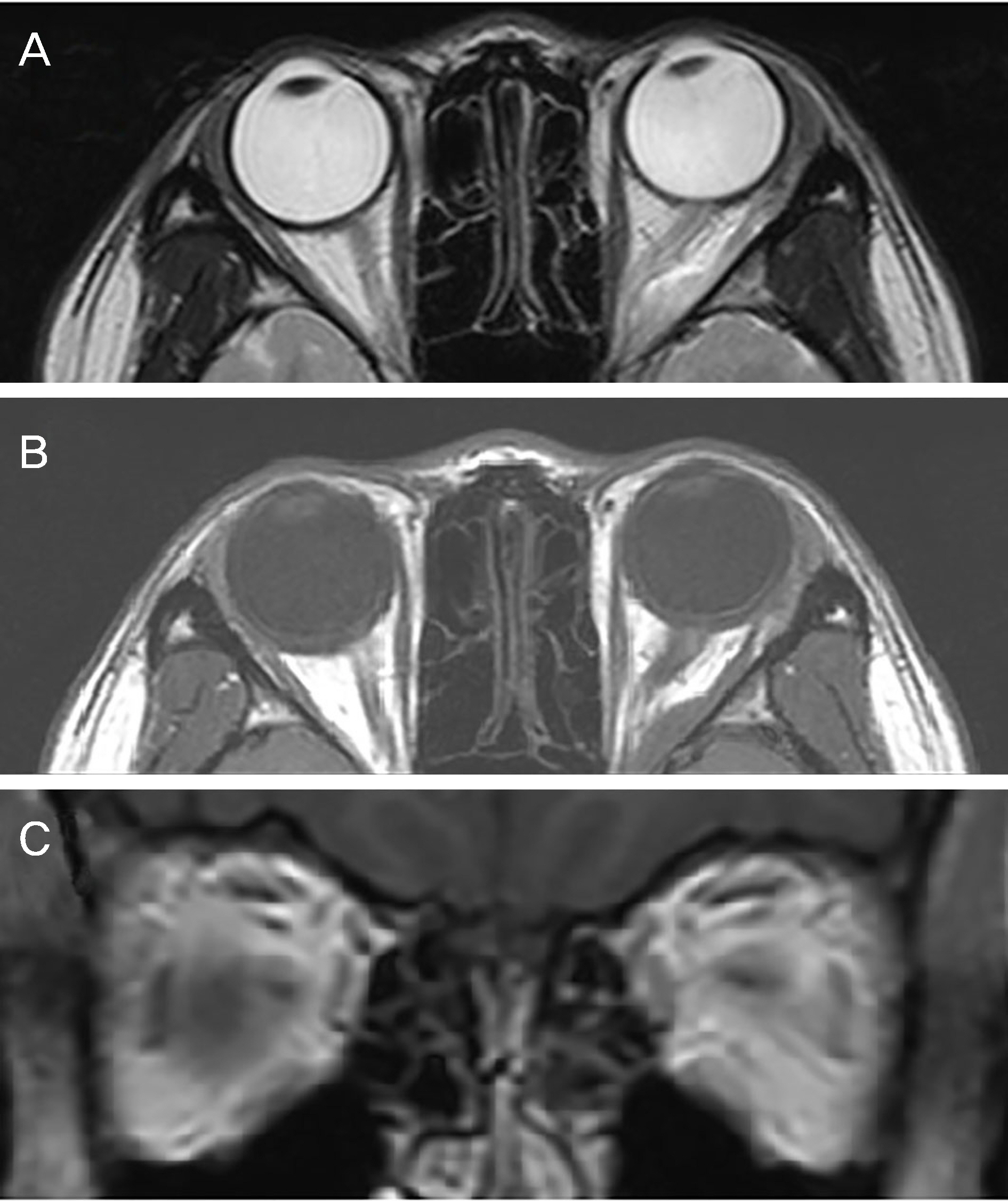
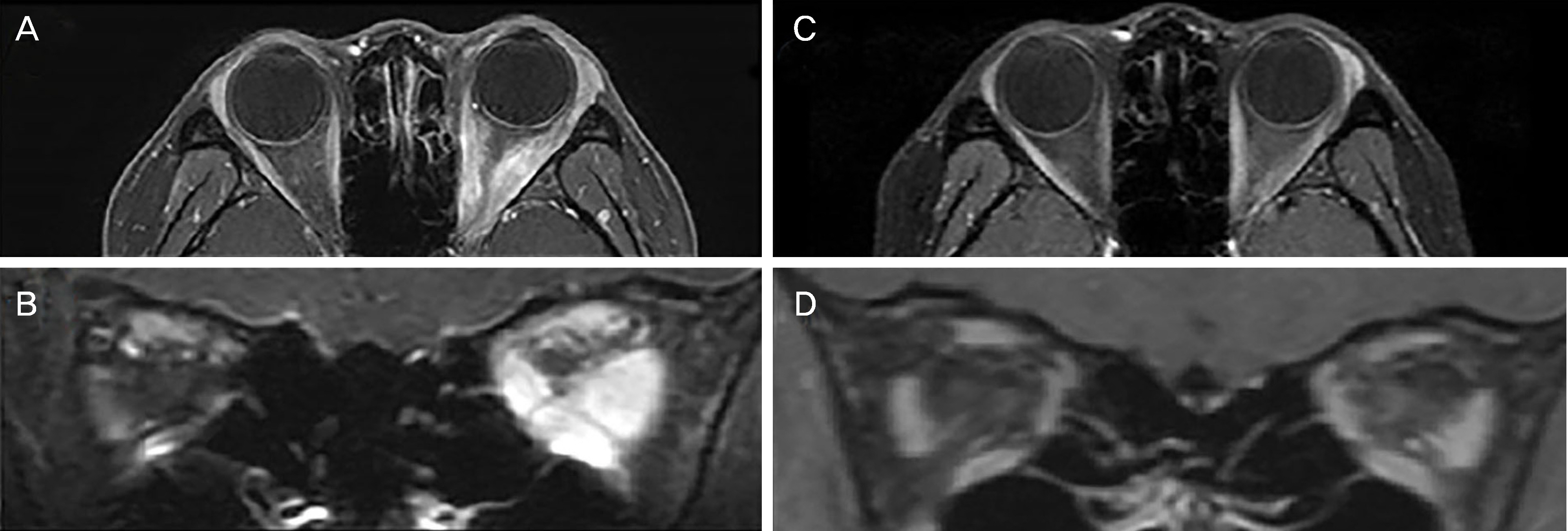
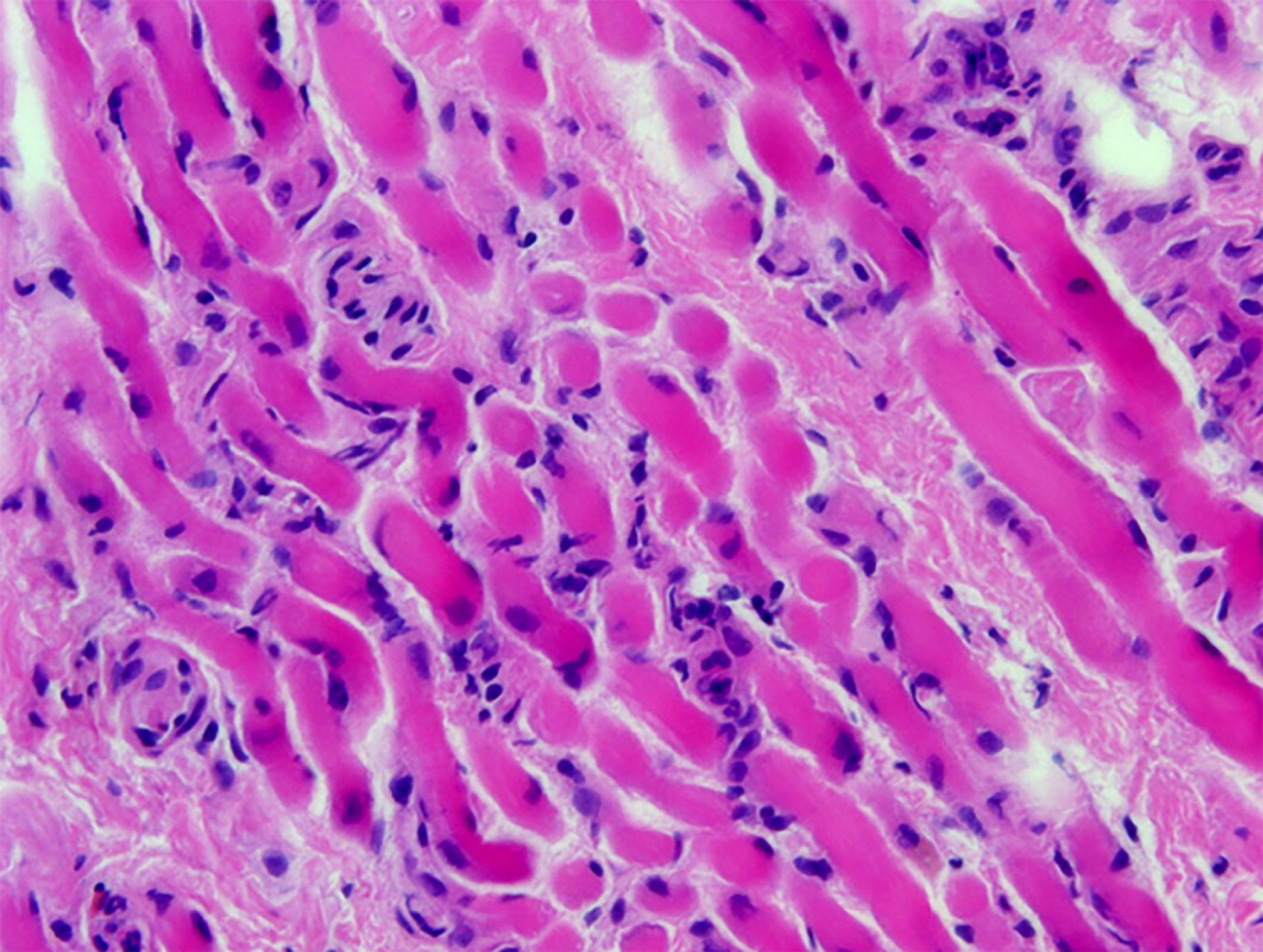
We examined a 20-year-old woman who complained of decreased visual acuity and binocular diplopia for 2 weeks. She showed 40-prism diopter left esotropia at the primary position. Her visual acuity with eyeglasses was 0.7 and 0.2 in the right and left eyes, respectively. Brain magnetic resonance imaging (MRI) revealed a round mass on the left lateral rectus muscle at the apex of the orbit with optic nerve compression. We planned orbital biopsy to exclude orbital lymphoma and other biopsy-requiring diseases. After 3 weeks, the visual acuity of her left eye decreased to 0.02. Repeated MRI revealed enlargement of all extraocular muscles on the left orbit. With biopsy showing several lymphocytes infiltrating muscle fibers, we made a diagnosis of idiopathic orbital myositis. Intravenous injection of corticosteroids was administered during hospitalization. After 2 weeks of corticosteroid therapy, the visual acuity of her left eye was improved to 0.63, the esotropia disappeared, and the enlargement of the left lateral rectus muscle was improved on orbital MRI.
CONCLUSIONS
For non-specific idiopathic orbital myositis located at the apex of the orbit and enlargement of the extraocular muscle in a short period with decreased visual acuity, administration of intravenous injection of corticosteroids before orbital biopsy could help restore vision.
MeSH Terms
Figure
Reference
-
References
1. Scott IU, Siatkowski RM. Idiopathic orbital myositis. Curr Opin Rheumatol. 1997; 9:504–12.
Article2. Schoser BG. Ocular myositis: diagnostic assessment, differential diagnoses, and therapy of a rare muscle disease – five new cases and review. Clin Ophthalmol. 2007; 1:37–42.3. Mombaerts I, Goldschmeding R, Schlingemann RO, Koornneef L. What is orbital pseudotumor? Surv Ophthalmol. 1996; 41:66–78.
Article4. Kim CH, Lim JY, Ahn JH, Jang JW. A case of idiopathic orbital myositis involving all extraocular muscles of both eyes. J Korean Ophthalmol Soc. 2001; 42:1615–20.5. Peter J, Andrew NH, Smith C, et al. Idiopathic inflammatory abdominal myositis presenting with vision loss. Orbit. 2014; 33:449–52.6. Rollnik JD, Requadt H. Ocular myositis as a rare cause of vision loss. Nervenarzt. 2017; 88:415–8.7. Matsuno K, Osako M, Osako S, et al. A case of orbital myositis complicated with optic neuropathy–analysis of the pathological mechanism of optic neuropathy from magnetic resonance imaging findings. Nippon Ganka Gakkai Zasshi. 2002; 106:304–11.8. Dursun D, Akova Y, Yücel E. Myositis and scleritis associated with Behcet's disease: an atypical presentation. Ocul Immunol Inflamm. 2004; 12:329–32.9. Moorman C, Elston JS. Acute orbital myositis. Eye (Lond). 1995; 9(Pt 1):96–101.
Article10. Lacey B, Chang W, Rootman J. Nonthyroid causes of extraocular muscle disease. Surv Ophthalmol. 1999; 44:187–213.
Article11. Jacobs D, Galetta S. Diagnosis and management of orbital pseudotumor. Curr Opin Ophthalmol. 2002; 13:347–51.
Article12. Harris GJ. Idiopathic orbital inflammation: a pathogenetic abdominal and treatment strategy: The 2005 ASOPRS Foundation Lecture. Ophthal Plast Reconstr Surg. 2006; 22:79–86.13. Weinstein GS, Dresner SC, Slamovits TL, Kennerdell JS. Acute and subacute orbital myositis. Am J Ophthalmol. 1983; 96:209–17.
Article14. Kubota T. Orbital myositis, idiopathic inflammatory myopathies-recent developments. InTech. 2011. http://www.intechopen.com/books/idiopathic-inflammatory-myopathies-recent-abdominals/orbital-myositis.15. Gordon LK. Orbital inflammatory disease: a diagnostic and abdominal challenge. Eye (Lond). 2006; 20:1196–206.16. Sung MS, Oh HJ, Ko BY, Yoon KC. Clinical features and results of steroid therapy for orbital inflammatory pseudotumor. J Korean Ophthalmol Soc. 2013; 54:185–91.
Article17. Park SJ, Jung SJ, Lee DG, Jang JW. Pseudotumor: distribution, clinical features, treatment outcomes. J Korean Ophthalmol Soc. 2008; 49:1379–86.18. Scott IU, Siatkowski RM. Thyroid eye disease. Semin Ophthalmol. 1999; 14:52–61.
Article19. Kim SH, Shin HH, Rho BK, et al. A case of intramuscular abdominal presenting with large-angle hypertropia. Korean J Ophthalmol. 2006; 20:195–8.20. Mombaerts I, Schlingemann RO, Goldschmeding R, Koornneef L. Are systemic corticosteroids useful in the management of orbital pseudotumors? Ophthalmology. 1996; 103:521–8.
Article21. Char DH, Miller T. Orbital pseudotumor. Fine-needle aspiration abdominal and response to therapy. Ophthalmology. 1993; 100:1702–10.22. Lee IS, Kim SJ, Kim HY, Lee SY. A case of sclerosing orbital pseudotumor. J Korean Ophthalmol Soc. 1996; 37:1321–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Idiopathic Orbital Myositis Involving All Extraocular Muscles of Both Eyes
- Effect of Corticosteroid on Orbital Pseudotumor Caused by Orbital Myositis
- Isolated Unilateral Ptosis Caused by Idiopathic Orbital Myositis
- Unilateral Ptosis Due to Isolated Levator Myositis
- A Case of Idiopathic Orbital Myositis