Trends in the incidence of tooth extraction due to periodontal disease: results of a 12-year longitudinal cohort study in South Korea
- Affiliations
-
- 1Department of Periodontology, Wonkwang University Daejeon Dental Hospital, Wonkwang University College of Dentistry, Daejeon, Korea.
- 2Department of Periodontology, Research Institute for Periodontal Regeneration, Yonsei University College of Dentistry, Seoul, Korea. shchoi726@yuhs.ac
- 3Department of Health Insurance Research, Ilsan Hospital, National Health Insurance Service, Goyang, Korea.
- KMID: 2392715
- DOI: http://doi.org/10.5051/jpis.2017.47.5.264
Abstract
- PURPOSE
This study evaluated trends in tooth extraction due to acute and chronic periodontal disease (PD) using data from the National Health Insurance Service-National Sample Cohort for 2002-2013.
METHODS
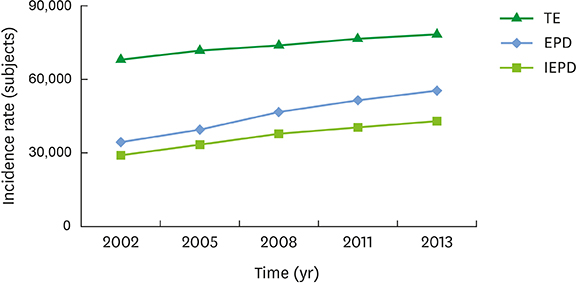
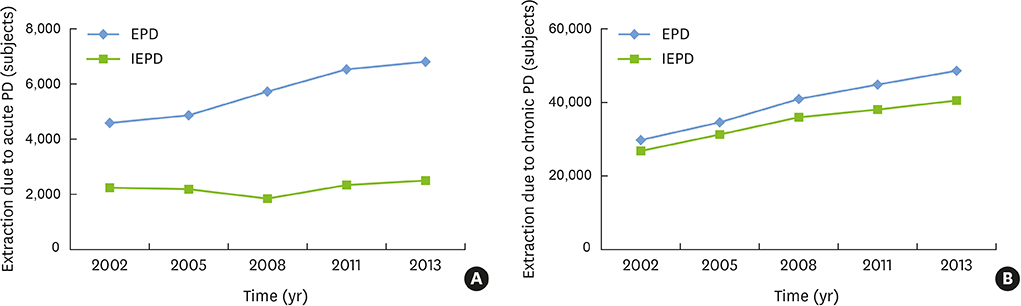
A random sample of 1,025,340 individuals was selected as a representative sample of the population, and a database (DB) of diagnostic and prescription codes was followed up for 12 years. We used multivariate logistic regression analysis to assess the incidence of total extraction (TE), extraction due to periodontal disease (EPD), and immediate extraction due to periodontal disease (IEPD) according to sociodemographic factors (sex, age, household income, health status, and area of residence).
RESULTS
The incidence of tooth extraction was found to be increasing, and at a higher rate for TE in PD patients. In 2002, 50.6% of cases of TE were caused by PD, and this increased to 70.8% in 2013, while the number of cases of IEPD increased from 42.8% to 54.9% over the same period. The incidence rates of extraction due to acute and chronic PD increased monotonically. We found that the incidence rates of TE, EPD, and IEPD were all 2-fold higher among patients with high income levels and those who were not beneficiaries of health insurance.
CONCLUSIONS
The rates of TE, EPD, and IEPD have been steadily increasing despite dental healthcare policies to expand public health insurance coverage, increasing the accessibility of dental clinics. Moreover, the effects of these policies were found to vary with both income and education levels. Consistent patient follow-up is required to observe changes in trends regarding tooth extraction according to changes in dental healthcare policies, and meticulous studies of such changes will ensure optimal policy reviews and revisions.
MeSH Terms
Figure
Cited by 4 articles
-
Diagnosis and prediction of periodontally compromised teeth using a deep learning-based convolutional neural network algorithm
Jae-Hong Lee, Do-hyung Kim, Seong-Nyum Jeong, Seong-Ho Choi
J Periodontal Implant Sci. 2018;48(2):114-123. doi: 10.5051/jpis.2018.48.2.114.Trends in the utilization of dental outpatient services affected by the expansion of health care benefits in South Korea to include scaling: a 6-year interrupted time-series study
Hee-Jung Park, Jun Hyup Lee, Sujin Park, Tae-Il Kim
J Periodontal Implant Sci. 2018;48(1):3-11. doi: 10.5051/jpis.2018.48.1.3.Association between health status and tooth loss in Korean adults: longitudinal results from the National Health Insurance Service-Health Examinee Cohort, 2002–2015
Yeon-Tae Kim, Jung-Kyu Choi, Do-Hyung Kim, Seong-Nyum Jeong, Jae-Hong Lee
J Periodontal Implant Sci. 2019;49(3):158-170. doi: 10.5051/jpis.2019.49.3.158.Charlson comorbidity index as a predictor of periodontal disease in elderly participants
Jae-Hong Lee, Jung-Kyu Choi, Seong-Nyum Jeong, Seong-Ho Choi
J Periodontal Implant Sci. 2018;48(2):92-102. doi: 10.5051/jpis.2018.48.2.92.
Reference
-
1. Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005; 83:661–669.2. Clarkson JJ, McLoughlin J. Role of fluoride in oral health promotion. Int Dent J. 2000; 50:119–128.
Article3. Hujoel PP. Endpoints in periodontal trials: the need for an evidence-based research approach. Periodontol 2000. 2004; 36:196–204.
Article4. Saintrain MV, de Souza EH. Impact of tooth loss on the quality of life. Gerodontology. 2012; 29:e632–6.
Article5. Yang SE, Park YG, Han K, Kim SY. Association between dental pain and tooth loss with health-related quality of life: the Korea national health and nutrition examination survey: a population-based cohort study. Medicine (Baltimore). 2016; 95:e4707.6. Joshipura KJ, Willett WC, Douglass CW. The impact of edentulousness on food and nutrient intake. J Am Dent Assoc. 1996; 127:459–467.
Article7. Naito M, Yuasa H, Nomura Y, Nakayama T, Hamajima N, Hanada N. Oral health status and health-related quality of life: a systematic review. J Oral Sci. 2006; 48:1–7.
Article8. Barbosa TS, Gavião MB. Oral health-related quality of life in children: part II. Effects of clinical oral health status. A systematic review. Int J Dent Hyg. 2008; 6:100–107.
Article9. Brennan DS, Spencer AJ, Roberts-Thomson KF. Tooth loss, chewing ability and quality of life. Qual Life Res. 2008; 17:227–235.
Article10. Chambrone LA, Chambrone L. Results of a 20-year oral hygiene and prevention programme on caries and periodontal disease in children attended at a private periodontal practice. Int J Dent Hyg. 2011; 9:155–158.
Article11. Nuvvula S, Chava VK, Nuvvula S. Primary culprit for tooth loss!! J Indian Soc Periodontol. 2016; 20:222–224.
Article12. Ribeiro LS, Dos Santos JN, Ramalho LM, Chaves S, Figueiredo AL, Cury PR. Risk indicators for tooth loss in Kiriri Adult Indians: a cross-sectional study. Int Dent J. 2015; 65:316–321.
Article13. Ogawa H, Yoshihara A, Hirotomi T, Ando Y, Miyazaki H. Risk factors for periodontal disease progression among elderly people. J Clin Periodontol. 2002; 29:592–597.
Article14. Armitage GC. Periodontal diagnoses and classification of periodontal diseases. Periodontol 2000. 2004; 34:9–21.
Article15. Lee JH, Choi JK, Kim SH, Cho KH, Kim YT, Choi SH, et al. Association between periodontal flap surgery for periodontitis and vasculogenic erectile dysfunction in Koreans. J Periodontal Implant Sci. 2017; 47:96–105.
Article16. Lee JH, Oh JY, Youk TM, Jeong SN, Kim YT, Choi SH. Association between periodontal disease and non-communicable diseases: a 12-year longitudinal health-examinee cohort study in South Korea. Medicine (Baltimore). 2017; 96:e7398.17. Choi JK, Kim YT, Kweon HI, Park EC, Choi SH, Lee JH. Effect of periodontitis on the development of osteoporosis: results from a nationwide population-based cohort study (2003–2013). BMC Womens Health. 2017; 17:77.
Article18. Singhrao SK, Harding A, Simmons T, Robinson S, Kesavalu L, Crean S. Oral inflammation, tooth loss, risk factors, and association with progression of Alzheimer’s disease. J Alzheimers Dis. 2014; 42:723–737.
Article19. Lee JH, Kweon HH, Choi JK, Kim YT, Choi SH. Association between periodontal disease and prostate cancer: results of a 12-year Longitudinal Cohort Study in South Korea. J Cancer. 2017; 8:2959–2965.
Article20. Lee JH, Lee JS, Choi JK, Kweon HI, Kim YT, Choi SH. National dental policies and socio-demographic factors affecting changes in the incidence of periodontal treatments in Korean: a nationwide population-based retrospective cohort study from 2002–2013. BMC Oral Health. 2016; 16:118.
Article21. Benjamin RM. Oral health: the silent epidemic. Public Health Rep. 2010; 125:158–159.
Article22. Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999; 4:1–6.
Article23. Page RC, Eke PI. Case definitions for use in population-based surveillance of periodontitis. J Periodontol. 2007; 78:1387–1399.
Article24. Celeste RK, Nadanovsky P, de Leon AP, Fritzell J. The individual and contextual pathways between oral health and income inequality in Brazilian adolescents and adults. Soc Sci Med. 2009; 69:1468–1475.
Article25. Lee JH, Lee JS, Park JY, Choi JK, Kim DW, Kim YT, et al. Association of lifestyle-related comorbidities with periodontitis: a nationwide cohort study in Korea. Medicine (Baltimore). 2015; 94:e1567.26. Celeste RK. Contextual effect of socioeconomic status influences chronic periodontitis. J Evid Based Dent Pract. 2007; 7:29–30.
Article27. Palmier AC, Andrade DA, Campos AC, Abreu MH, Ferreira EF. Socioeconomic indicators and oral health services in an underprivileged area of Brazil. Rev Panam Salud Publica. 2012; 32:22–29.28. Park HJ, Lee JH, Park S, Kim TI. Changes in dental care access upon health care benefit expansion to include scaling. J Periodontal Implant Sci. 2016; 46:405–414.
Article29. Organisation for Economic Co-operation and Development. Health care resources: dentists [Internet]. Paris: Organisation for Economic Co-operation and Development;cited 2017 May 17. Available from: http://stats.oecd.org/index.aspx?queryid=30177#.30. Health Insurance Review & Assessment Service (KR). Outpatient disease statistics [Internet]. Wonju: Health Insurance Review & Assessment Service;cited 2016 Oct 17. Available from: http://opendata.hira.or.kr/op/opc/olapHifrqSickInfo.do.31. Buchwald S, Kocher T, Biffar R, Harb A, Holtfreter B, Meisel P. Tooth loss and periodontitis by socio-economic status and inflammation in a longitudinal population-based study. J Clin Periodontol. 2013; 40:203–211.
Article32. Kim DW, Park JC, Rim TT, Jung UW, Kim CS, Donos N, et al. Socioeconomic disparities of periodontitis in Koreans based on the KNHANES IV. Oral Dis. 2014; 20:551–559.
Article33. Borges CM, Campos AC, Vargas AM, Ferreira EF. Adult tooth loss profile in accordance with social capital and demographic and socioeconomic characteristics. Cien Saude Colet. 2014; 19:1849–1858.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reasons for extraction of permanent teeth in Korea
- Analysis of reasons for extracting permanent teeth among Korean adults with oral diseases
- Autogenous tooth transplantation for replacing a lost tooth: case reports
- Healing pattern of the mucous membrane after tooth extraction in the maxillary sinus
- Association between health status and tooth loss in Korean adults: longitudinal results from the National Health Insurance Service-Health Examinee Cohort, 2002–2015