J Periodontal Implant Sci.
2019 Jun;49(3):158-170. 10.5051/jpis.2019.49.3.158.
Association between health status and tooth loss in Korean adults: longitudinal results from the National Health Insurance Service-Health Examinee Cohort, 2002–2015
- Affiliations
-
- 1Department of Periodontology, Daejeon Dental Hospital, Institute of Wonkwang Dental Research, Wonkwang University College of Dentistry, Daejeon, Korea. ljaehong@gmail.com
- 2Department of Health Insurance Research, Ilsan Hospital, National Health Insurance Service, Goyang, Korea.
- KMID: 2454086
- DOI: http://doi.org/10.5051/jpis.2019.49.3.158
Abstract
- PURPOSE
This study investigated the association between health status and tooth loss based on data from the National Health Insurance Service-Health Examinee Cohort in 2002-2015.
METHODS
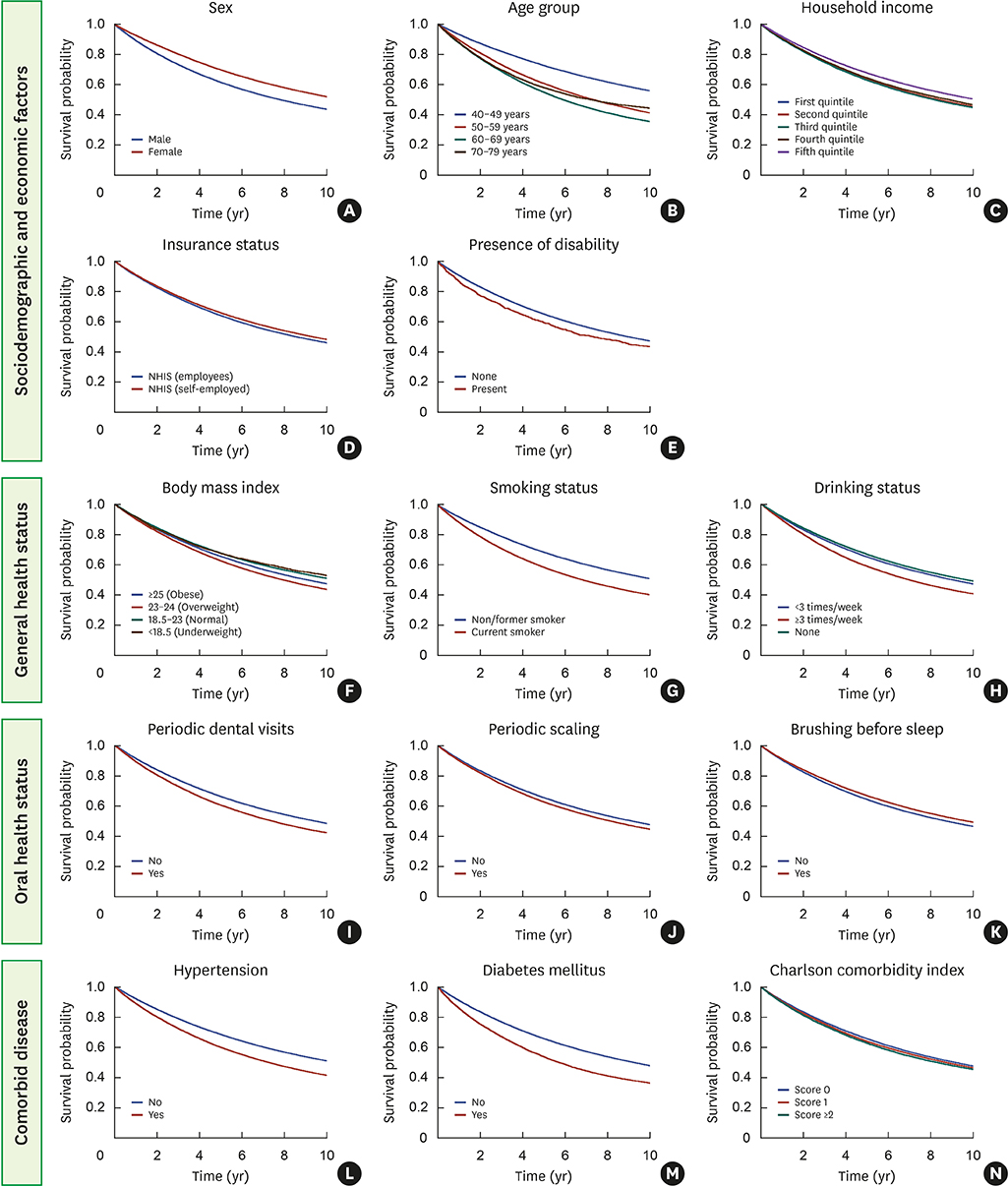
Multivariate Cox proportional hazards regression analyses were applied to a longitudinal retrospective database, which was updated and newly released in 2018, to assess the association between health status and tooth loss while adjusting for potential confounders among sociodemographic and economic factors (sex, age, household income, insurance, and presence of disability), general and oral health status (body mass index [BMI], smoking and drinking status, periodic dental visits and scaling, and brushing before sleep), and comorbid disease (hypertension, diabetes mellitus [DM], and Charlson comorbidity index [CCI]).
RESULTS
Among 514,866 participants from a South Korean population, 234,247 (45.5%) participants satisfying the inclusion criteria were analyzed. In the adjusted multivariate analysis, sex, age, household income, insurance, presence of disability, BMI, smoking and drinking status, periodic scaling, tooth brushing before sleep, DM, and CCI showed statistically significant associations with the loss of at least 1 tooth. The risk of experiencing a loss of ≥4 teeth was associated with an increase in age (in those 50-59 years of age: hazard ratio [HR], 1.98; 95% confidence interval [CI], 1.93-2.03; in those 60-69 years of age: HR, 2.93; 95% CI, 2.85-3.02; and in those 70-79 years of age: HR, 2.93; 95%, CI 2.81-3.05), smoking (HR, 1.69; 95% CI, 1.65-1.73), and DM (HR, 1.43; 95% CI, 1.38-1.48).
CONCLUSIONS
The results of this study showed that the risk of experiencing tooth loss was related to multiple determinants. DM and smoking were especially significantly associated with tooth loss.
MeSH Terms
Figure
Reference
-
1. Petersen PE. World Health Organization global policy for improvement of oral health--World Health Assembly 2007. Int Dent J. 2008; 58:115–121.
Article2. Choi JK, Kim YT, Kweon HI, Park EC, Choi SH, Lee JH. Effect of periodontitis on the development of osteoporosis: results from a nationwide population-based cohort study (2003–2013). BMC Womens Health. 2017; 17:77.
Article3. Lee JH, Kweon HH, Choi JK, Kim YT, Choi SH. Association between periodontal disease and prostate cancer: results of a 12-year longitudinal cohort study in South Korea. J Cancer. 2017; 8:2959–2965.
Article4. N'gom PI, Woda A. Influence of impaired mastication on nutrition. J Prosthet Dent. 2002; 87:667–673.5. Mealey BL. Periodontal disease and diabetes. A two-way street. J Am Dent Assoc. 2006; 137:Suppl. 26S–31S.6. Lee JH, Jeong SN, Choi SH. Predictive data mining for diagnosing periodontal disease: the Korea National Health and Nutrition Examination Surveys (KNHANES V and VI) from 2010 to 2015. J Public Health Dent. 2018; 79:44–52.
Article7. Lee JH, Lee JS, Park JY, Choi JK, Kim DW, Kim YT, et al. Association of lifestyle-related comorbidities with periodontitis: a nationwide cohort study in Korea. Medicine (Baltimore). 2015; 94:e1567.8. Lee JH, Lim NK, Cho MC, Park HY. Epidemiology of heart failure in Korea: present and future. Korean Circ J. 2016; 46:658–664.
Article9. Lee JH, Oh JY, Choi JK, Kim YT, Park YS, Jeong SN, et al. Trends in the incidence of tooth extraction due to periodontal disease: results of a 12-year longitudinal cohort study in South Korea. J Periodontal Implant Sci. 2017; 47:264–272.
Article10. Lee JH, Lee JS, Choi JK, Kweon HI, Kim YT, Choi SH. National dental policies and socio-demographic factors affecting changes in the incidence of periodontal treatments in Korean: a nationwide population-based retrospective cohort study from 2002-2013. BMC Oral Health. 2016; 16:118.
Article11. Lee JH, Choi JK, Jeong SN, Choi SH. Charlson comorbidity index as a predictor of periodontal disease in elderly participants. J Periodontal Implant Sci. 2018; 48:92–102.
Article12. Reisine ST, Psoter W. Socioeconomic status and selected behavioral determinants as risk factors for dental caries. J Dent Educ. 2001; 65:1009–1016.
Article13. Petersen PE. Sociobehavioural risk factors in dental caries - international perspectives. Community Dent Oral Epidemiol. 2005; 33:274–279.
Article14. Tonetti MS, Muller-Campanile V, Lang NP. Changes in the prevalence of residual pockets and tooth loss in treated periodontal patients during a supportive maintenance care program. J Clin Periodontol. 1998; 25:1008–1016.
Article15. Lee JH, Oh JY, Youk TM, Jeong SN, Kim YT, Choi SH. Association between periodontal disease and non-communicable diseases: a 12-year longitudinal health-examinee cohort study in South Korea. Medicine (Baltimore). 2017; 96:e7398.16. Meisel P, Reifenberger J, Haase R, Nauck M, Bandt C, Kocher T. Women are periodontally healthier than men, but why don't they have more teeth than men? Menopause. 2008; 15:270–275.
Article17. Russell SL, Gordon S, Lukacs JR, Kaste LM. Sex/Gender differences in tooth loss and edentulism: historical perspectives, biological factors, and sociologic reasons. Dent Clin North Am. 2013; 57:317–337.18. Bernabé E, Marcenes W. Income inequality and tooth loss in the United States. J Dent Res. 2011; 90:724–729.
Article19. Pitiphat W, Merchant AT, Rimm EB, Joshipura KJ. Alcohol consumption increases periodontitis risk. J Dent Res. 2003; 82:509–513.
Article20. Hach M, Holm-Pedersen P, Adegboye AR, Avlund K. The effect of alcohol consumption on periodontitis in older Danes. Int J Dent Hyg. 2015; 13:261–267.
Article21. Reynolds MA. Modifiable risk factors in periodontitis: at the intersection of aging and disease. Periodontol 2000. 2014; 64:7–19.
Article22. Tezal M, Grossi SG, Ho AW, Genco RJ. The effect of alcohol consumption on periodontal disease. J Periodontol. 2001; 72:183–189.
Article23. Susin C, Wagner MC, Haas AN, Oppermann RV, Albandar JM. The association between alcohol consumption and periodontitis in southern Brazilian adults. J Periodontal Res. 2015; 50:622–628.
Article24. Agnihotri R, Gaur S. Implications of tobacco smoking on the oral health of older adults. Geriatr Gerontol Int. 2014; 14:526–540.
Article25. Khader YS, Dauod AS, El-Qaderi SS, Alkafajei A, Batayha WQ. Periodontal status of diabetics compared with nondiabetics: a meta-analysis. J Diabetes Complications. 2006; 20:59–68.
Article26. Kaur G, Holtfreter B, Rathmann W, Schwahn C, Wallaschofski H, Schipf S, et al. Association between type 1 and type 2 diabetes with periodontal disease and tooth loss. J Clin Periodontol. 2009; 36:765–774.
Article27. Lalla E, Papapanou PN. Diabetes mellitus and periodontitis: a tale of two common interrelated diseases. Nat Rev Endocrinol. 2011; 7:738–748.
Article28. Scannapieco FA. Position paper of the American Academy of Periodontology: periodontal disease as a potential risk factor for systemic diseases. J Periodontol. 1998; 69:841–850.29. Taylor GW. Bidirectional interrelationships between diabetes and periodontal diseases: an epidemiologic perspective. Ann Periodontol. 2001; 6:99–112.
Article30. Calsina G, Ramón JM, Echeverría JJ. Effects of smoking on periodontal tissues. J Clin Periodontol. 2002; 29:771–776.
Article31. Patel MH, Kumar JV, Moss ME. Diabetes and tooth loss: an analysis of data from the National Health and Nutrition Examination Survey, 2003–2004. J Am Dent Assoc. 2013; 144:478–485.
Article32. Taylor GW, Manz MC, Borgnakke WS. Diabetes, periodontal diseases, dental caries, and tooth loss: a review of the literature. Compend Contin Educ Dent. 2004; 25:179–184. 86–178. 9033. Pischon N, Heng N, Bernimoulin JP, Kleber BM, Willich SN, Pischon T. Obesity, inflammation, and periodontal disease. J Dent Res. 2007; 86:400–409.
Article34. Al-Zahrani MS, Bissada NF, Borawskit EA. Obesity and periodontal disease in young, middle-aged, and older adults. J Periodontol. 2003; 74:610–615.
Article35. Wood N, Johnson RB, Streckfus CF. Comparison of body composition and periodontal disease using nutritional assessment techniques: Third National Health and Nutrition Examination Survey (NHANES III). J Clin Periodontol. 2003; 30:321–327.
Article36. Baek HJ, Lee SG, Song KB, Kwon HJ. The association of metabolic syndrome and periodontitis in Korean adult population. J Korean Acad Oral Health. 2010; 34:338–345.37. Shimazaki Y, Saito T, Yonemoto K, Kiyohara Y, Iida M, Yamashita Y. Relationship of metabolic syndrome to periodontal disease in Japanese women: the Hisayama Study. J Dent Res. 2007; 86:271–275.
Article38. Faulks D, Hennequin M. Evaluation of a long-term oral health program by carers of children and adults with intellectual disabilities. Spec Care Dentist. 2000; 20:199–208.
Article39. Altun C, Guven G, Akgun OM, Akkurt MD, Basak F, Akbulut E. Oral health status of disabled individuals attending special schools. Eur J Dent. 2010; 4:361–366.40. Joshipura KJ, Douglass CW, Willett WC. Possible explanations for the tooth loss and cardiovascular disease relationship. Ann Periodontol. 1998; 3:175–183.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The financial estimate of dental implant treatment about the National Health Insurance coverage for the Korean young adults
- Status of Diabetic Neuropathy in Korea: A National Health Insurance Service-National Sample Cohort Analysis (2006 to 2015) (Diabetes Metab J 2021;45:115-9)
- Analysis of the incidence of dementia in complete edentulous patients using the National Health Insurance Service-Elderly Cohort Database (NHIS-ECD)
- Severe periodontitis with tooth loss as a modifiable risk factor for the development of Alzheimer, vascular, and mixed dementia: National Health Insurance Service-National Health Screening Retrospective Cohort 2002–2015
- Trends in the incidence of tooth extraction due to periodontal disease: results of a 12-year longitudinal cohort study in South Korea