Nutr Res Pract.
2013 Apr;7(2):77-81.
Short-term impact of sugar consumption on hunger and ad libitum food intake in young women
- Affiliations
-
- 1Laboratory of Eating Practices and Behavior (PratiCA), Course of Nutrition and Metabolism, University of Sao Paulo, Ribeirao Preto, SP, Brazil. ferpenaforte@usp.br
- 2Department of Nutrition, Federal University of Triangulo Mineiro, Uberaba, MG, Brazil.
- 3Course of Nutrition and Metabolism, University of Sao Paulo, Ribeirao Preto, SP, Brazil.
Abstract
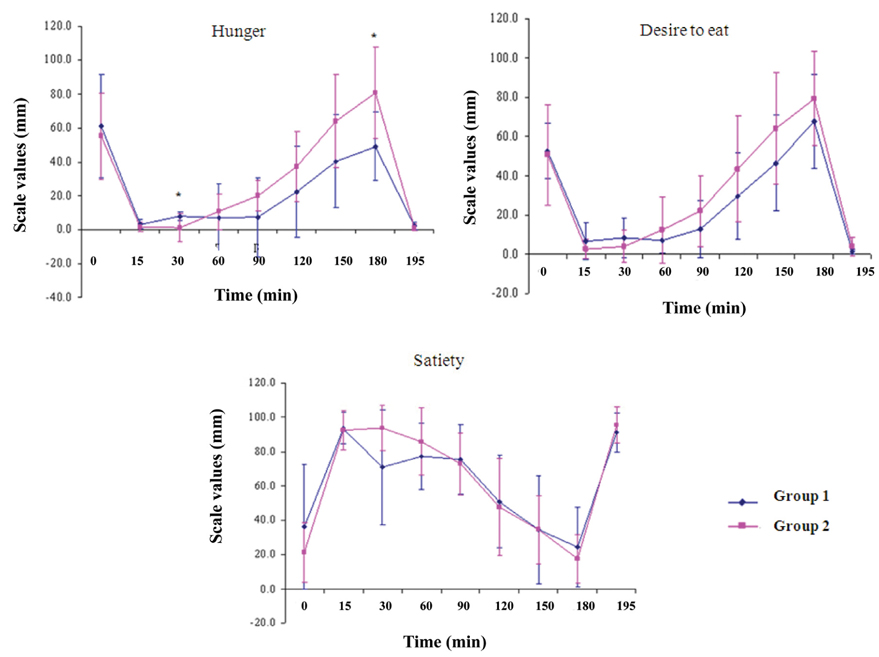
- The hypothesis of this study was that greater sugar consumption at breakfast promotes a stronger sensation of hunger and a later increase in energy consumption. The objective was to assess the relation between sugar consumption in a meal and the subsequent sensations of hunger and ad libitum food consumption. Sixteen women consumed a breakfast accompanied by 2 drinks sweetened ad libitum with sugar. After 3 h, a lunch was offered to evaluate ad libitum food consumption. During the period from breakfast to lunch, hunger sensations were evaluated at 30 min intervals. Women were divided according to the median amount of sugar used to sweeten the breakfast drinks (20 g). The group who consumed sugar above the median showed a greater hunger sensation in the preprandial period, and a greater ad libitum intake at lunch (390 +/- 130 g x 256 +/- 67 g, P = 0.002), compared to the group who had a lower sugar consumption. The amount of sugar consumed at breakfast was correlated positively with the sensation of preprandial hunger and food intake at lunch. We concluded that foods with a high glycemic index can modulate the appetite within a short period of time.
Keyword
Figure
Reference
-
1. Burger KN, Beulens JW, Boer JM, Spijkerman AM, van der AD. Dietary glycemic load and glycemic index and risk of coronary heart disease and stroke in Dutch men and women: the EPIC-MORGEN study. PLoS One. 2011. 6:e25955.
Article2. Kochan AM, Wolever TM, Chetty VT, Anand SS, Gerstein HC, Sharma AM. Glycemic index predicts individual glucose responses after self-selected breakfasts in free-living, abdominally obese adults. J Nutr. 2012. 142:27–32.
Article3. Morris KL, Zemel MB. Glycemic index, cardiovascular disease, and obesity. Nutr Rev. 1999. 57:273–276.
Article4. Gonçalves Reis CE, Dullius J. Glycemic acute changes in type 2 diabetics caused by low and high glycemic index diets. Nutr Hosp. 2011. 26:546–552.5. Jenkins DJ, Wolever TM, Taylor RH, Barker H, Fielden H, Baldwin JM, Bowling AC, Newman HC, Jenkins AL, Goff DV. Glycemic index of foods: a physiological basis for carbohydrate exchange. Am J Clin Nutr. 1981. 34:362–366.
Article6. Brand-Miller JC, Holt SH, Pawlak DB, McMillan J. Glycemic index and obesity. Am J Clin Nutr. 2002. 76:281S–285S.
Article7. Brouns F, Bjorck I, Frayn KN, Gibbs AL, Lang V, Slama G, Wolever TM. Glycaemic index methodology. Nutr Res Rev. 2005. 18:145–171.
Article8. Reid M, Hetherington M. Relative effects of carbohydrates and protein on satiety -- a review of methodology. Neurosci Biobehav Rev. 1997. 21:295–308.
Article9. Caruso L, Menezes EW. Glycemic index of foods. J Braz Soc Food Nutr. 2000. 19:49–64.10. Parillo M, Licenziati MR, Vacca M, De Marco D, Iannuzzi A. Metabolic changes after a hypocaloric, low-glycemic-index diet in obese children. J Endocrinol Invest. 2012. 35:629–633.11. Spieth LE, Harnish JD, Lenders CM, Raezer LB, Pereira MA, Hangen SJ, Ludwig DS. A low-glycemic index diet in the treatment of pediatric obesity. Arch Pediatr Adolesc Med. 2000. 154:947–951.
Article12. Roberts SB. High-glycemic index foods, hunger, and obesity: is there a connection? Nutr Rev. 2000. 58:163–169.
Article13. Venn BJ, Green TJ. Glycemic index and glycemic load: measurement issues and their effect on diet-disease relationships. Eur J Clin Nutr. 2007. 61:Suppl 1. S122–S131.
Article14. Vigilância alimentar e nutricional - SISVAN: orientações básicas para a coleta, processamento, análise de dados e informação em serviços de saúde. 2004. Brasília: Ministério da Saúde.15. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000. 894:i–xii. 1–253.16. Flint A, Raben A, Blundell JE, Astrup A. Reproducibility, power and validity of visual analogue scales in assessment of appetite sensations in single test meal studies. Int J Obes Relat Metab Disord. 2000. 24:38–48.
Article17. de Graaf C. The validity of appetite ratings. Appetite. 1993. 21:156–160.
Article18. Arumugam V, Lee JS, Nowak JK, Pohle RJ, Nyrop JE, Leddy JJ, Pelkman CL. A high-glycemic meal pattern elicited increased subjective appetite sensations in overweight and obese women. Appetite. 2008. 50:215–222.
Article19. Anderson GH, Woodend D. Consumption of sugars and the regulation of short-term satiety and food intake. Am J Clin Nutr. 2003. 78:843S–849S.
Article20. Campfield LA, Smith FJ. Blood glucose dynamics and control of meal initiation: a pattern detection and recognition theory. Physiol Rev. 2003. 83:25–58.
Article21. Louie JC, Buyken AE, Brand-Miller JC, Flood VM. The link between dietary glycemic index and nutrient adequacy. Am J Clin Nutr. 2012. 95:694–702.
Article22. Nilsson AC, Ostman EM, Holst JJ, Björck IM. Including indigestible carbohydrates in the evening meal of healthy subjects improves glucose tolerance, lowers inflammatory markers, and increases satiety after a subsequent standardized breakfast. J Nutr. 2008. 138:732–739.
Article23. Furchner-Evanson A, Petrisko Y, Howarth L, Nemoseck T, Kern M. Type of snack influences satiety responses in adult women. Appetite. 2010. 54:564–569.
Article24. Batista SM, Assis MA, Teixeira E, Damian C. Evaluation of the glycemic response, satiety and palatability after the consumption of high and low glycemic index diets. Aliment Nutr. 2007. 18:315–323.25. Diabetes Prevention Program Research Group. The cost-effectiveness of DPP interventions to delay or prevent type 2 diabetes. Diabetes. 2002. 51:A74.26. Warren JM, Henry CJ, Simonite V. Low glycemic index breakfasts and reduced food intake in preadolescent children. Pediatrics. 2003. 112:e414.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chia seed (Salvia Hispanica L.) added yogurt reduces short-term food intake and increases satiety: randomised controlled trial
- Diabetes and Non‑Nutritive Sweeteners
- Effects of Spicy Soup with Red Pepper on Body Temperature, Blood Pressure, Appetite and Energy Intake
- Factors affecting sugar intake in adults based on the social cognitive theory
- High School Students' Sugar Intake Behaviors and Consumption of Sugary Processed Food Based on the Level of Sugar-related Nutrition Knowledge in Seoul Area