Pediatr Infect Vaccine.
2017 Apr;24(1):1-6. 10.14776/piv.2017.24.1.1.
Diagnostic Significance of the Delta Neutrophil Index and Other Conventional Parameters in Neonatal Bacteremia
- Affiliations
-
- 1Department of Pediatrics, Yonsei University Wonju College of Medicine, Wonju, the Republic of Korea. khm9120@yonsei.ac.kr
- KMID: 2390875
- DOI: http://doi.org/10.14776/piv.2017.24.1.1
Abstract
- PURPOSE
We investigated the effectiveness of the delta neutrophil index (DNI) for the prediction of neonatal bacteremia and compared it to other indices.
METHODS
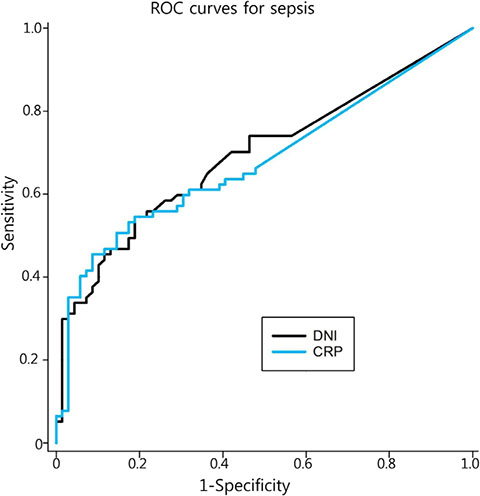
A total of 146 pediatric patients, aged less than 31 days, admitted to the neonatal intensive care unit of Wonju Severance Christian Hospital with fever before or during hospitalization were enrolled in this study. We divided the patients into two groups based on the existence of neonatal bacteremia and performed blood culture tests on both groups. We examined white blood cell count, absolute neutrophil count, DNI, platelet count, and C-reactive protein (CRP) test. We used a receiver operating characteristic (ROC) curve to evaluate their diagnostic significance.
RESULTS
Seventy-seven patients were diagnosed with neonatal bacteremia. The mean gestational age was 38.74 weeks and the mean birth weight was 3.20 kg. The mean gestational age of the control group was 33.34 weeks and the mean birth weight was 2.20 kg. Causative organisms of bacteremia included Staphylococcus aureus (n=22), Staphylococcus epidermidis (n=18), and Streptococcus agalactiae (n=8). Both DNI and CRP were significantly associated with neonatal bacteremia after adjusting for gestational age and birth weight. The area under the ROC curve (AUC) for DNI (0.70) was higher than that for CRP (0.68).
CONCLUSIONS
The DNI can be used to effectively predict neonatal bacteremia. The prediction will be more accurate if DNI is used in conjunction with other indices. In future, it will be useful to compare DNI with other indices and investigate its relationship with prognosis.
MeSH Terms
Figure
Cited by 1 articles
-
Delta neutrophil index as a predictor of vesicoureteral reflux in children with febrile urinary tract infection
Jae Eun Kim, Jun Suk Oh, Jung Min Yoon, Kyung Ok Ko, Eun Jung Cheon
Child Kidney Dis. 2022;26(1):46-51. doi: 10.3339/ckd.22.026.
Reference
-
1. Jiang JH, Chiu NC, Huang FY, Kao HA, Hsu CH, Hung HY, et al. Neonatal sepsis in the neonatal intensive care unit: characteristics of early versus late onset. J Microbiol Immunol Infect. 2004; 37:301–306.2. Garcia-Prats JA, Cooper TR, Schneider VF, Stager CE, Hansen TN. Rapid detection of microorganisms in blood cultures of newborn infants utilizing an automated blood culture system. Pediatrics. 2000; 105(3 Pt 1):523–527.
Article3. Kumar Y, Qunibi M, Neal TJ, Yoxall CW. Time to positivity of neonatal blood cultures. Arch Dis Child Fetal Neonatal Ed. 2001; 85:F182–F186.
Article4. Benitz WE. Adjunct laboratory tests in the diagnosis of early-onset neonatal sepsis. Clin Perinatol. 2010; 37:421–438.
Article5. Muller B, Christ-Crain M, Nylen ES, Snider R, Becker KL. Limits to the use of the procalcitonin level as a diagnostic marker. Clin Infect Dis. 2004; 39:1867–1868.
Article6. Arnon S, Litmanovitz I. Diagnostic tests in neonatal sepsis. Curr Opin Infect Dis. 2008; 21:223–227.
Article7. Nahm CH, Choi JW, Lee J. Delta neutrophil index in automated immature granulocyte counts for assessing disease severity of patients with sepsis. Ann Clin Lab Sci. 2008; 38:241–246.8. Centers for Disease Control and Prevention. Prevention of perinatal group B streptococcal disease: a public health perspective. MMWR Recomm Rep. 1996; 45(RR-7):1–24.9. Rodwell RL, Leslie AL, Tudehope DI. Early diagnosis of neonatal sepsis using a hematologic scoring system. J Pediatr. 1988; 112:761–767.
Article10. Benitz WE, Han MY, Madan A, Ramachandra P. Serial serum C-reactive protein levels in the diagnosis of neonatal infection. Pediatrics. 1998; 102:E41.
Article11. Ng PC, Cheng SH, Chui KM, Fok TF, Wong MY, Wong W, et al. Diagnosis of late onset neonatal sepsis with cytokines, adhesion molecule, and C-reactive protein in preterm very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 1997; 77:F221–F227.
Article12. Guibourdenche J, Bedu A, Petzold L, Marchand M, Mariani-Kurdjian P, Hurtaud-Roux MF, et al. Biochemical markers of neonatal sepsis: value of procalcitonin in the emergency setting. Ann Clin Biochem. 2002; 39(Pt 2):130–135.
Article13. Ng PC, Li G, Chui KM, Chu WC, Li K, Wong RP, et al. Neutrophil CD64 is a sensitive diagnostic marker for earlyonset neonatal infection. Pediatr Res. 2004; 56:796–803.
Article14. Schultz C, Rott C, Temming P, Schlenke P, Moller JC, Bucsky P. Enhanced interleukin-6 and interleukin-8 synthesis in term and preterm infants. Pediatr Res. 2002; 51:317–322.
Article15. Mehr S, Doyle LW. Cytokines as markers of bacterial sepsis in newborn infants: a review. Pediatr Infect Dis J. 2000; 19:879–887.
Article16. Mishra UK, Jacobs SE, Doyle LW, Garland SM. Newer approaches to the diagnosis of early onset neonatal sepsis. Arch Dis Child Fetal Neonatal Ed. 2006; 91:F208–F212.
Article17. Ng PC, Lam HS. Biomarkers for late-onset neonatal sepsis: cytokines and beyond. Clin Perinatol. 2010; 37:599–610.
Article18. Cornbleet PJ. Clinical utility of the band count. Clin Lab Med. 2002; 22:101–136.
Article19. Ansari-Lari MA, Kickler TS, Borowitz MJ. Immature granulocyte measurement using the Sysmex XE-2100. Relationship to infection and sepsis. Am J Clin Pathol. 2003; 120:795–799.
Article20. Nigro KG, O'Riordan M, Molloy EJ, Walsh MC, Sandhaus LM. Performance of an automated immature granulocyte count as a predictor of neonatal sepsis. Am J Clin Pathol. 2005; 123:618–624.
Article21. Ardron MJ, Westengard JC, Dutcher TF. Band neutrophil counts are unnecessary for the diagnosis of infection in patients with normal total leukocyte counts. Am J Clin Pathol. 1994; 102:646–649.
Article22. Harris N, Jou JM, Devoto G, Lotz J, Pappas J, Wranovics D, et al. Performance evaluation of the ADVIA 2120 hematology analyzer: an international multicenter clinical trial. Lab Hematol. 2005; 11:62–70.
Article23. Kim HW, Yoon JH, Jin SJ, Kim SB, Ku NS, Jeong SJ, et al. Delta neutrophil index as a prognostic marker of early mortality in gram negative bacteremia. Infect Chemother. 2014; 46:94–102.
Article24. Hwang YJ, Chung SP, Park YS, Chung HS, Lee HS, Park JW, et al. Newly designed delta neutrophil index-to-serum albumin ratio prognosis of early mortality in severe sepsis. Am J Emerg Med. 2015; 33:1577–1582.
Article25. Chiesa C, Pellegrini G, Panero A, Osborn JF, Signore F, Assumma M, et al. C-reactive protein, interleukin-6, and procalcitonin in the immediate postnatal period: influence of illness severity, risk status, antenatal and perinatal complications, and infection. Clin Chem. 2003; 49:60–68.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of Perforation of Acute Appendicitis using the Delta Neutrophil Index Reflecting Peripheral Immature Granulocyte Count
- Diagnostic Usefulness of Basic Hematologic Tests for the Detection of Bacteremia in Febrile Patients with Neutrophilia
- Delta neutrophil index as a predictor of vesicoureteral reflux in children with febrile urinary tract infection
- Delta Neutrophil Index as a Prognostic Marker of Early Mortality in Gram Negative Bacteremia
- Delta neutrophil index in obese and non-obese polycystic ovary syndrome patients