Korean Circ J.
2016 Sep;46(5):646-653. 10.4070/kcj.2016.46.5.646.
Patient Characteristics and the Incidence of Radiation-induced Dermatitis Following Radiofrequency Catheter Ablation
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea. seil@snu.ac.kr
- 2Department of Dermatology, Seoul National University Hospital, Seoul, Korea.
- KMID: 2389621
- DOI: http://doi.org/10.4070/kcj.2016.46.5.646
Abstract
- BACKGROUND AND OBJECTIVES
Radiofrequency catheter ablation (RFCA) exposes patients to fixed angle radiation for extended periods of time. We investigated the incidence and characteristics of radiation-induced dermatitis (RID) associated with RFCA.
SUBJECTS AND METHODS
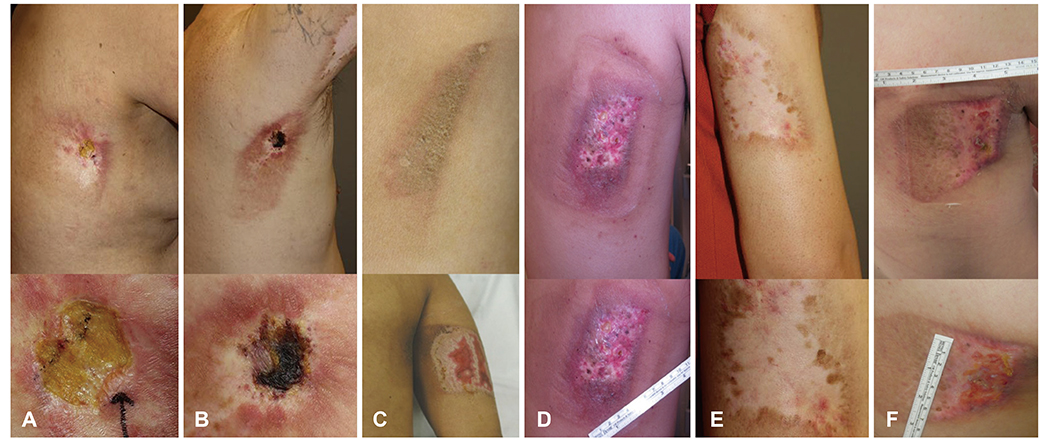
We screened 1347 consecutive patients from 2000 to 2011 who underwent RFCA for any indication and reviewed patients with dermatologic issues at the 1-month follow-up. Skin lesions were classified into three groups: most likely RID, probable RID, and possible RID.
RESULTS
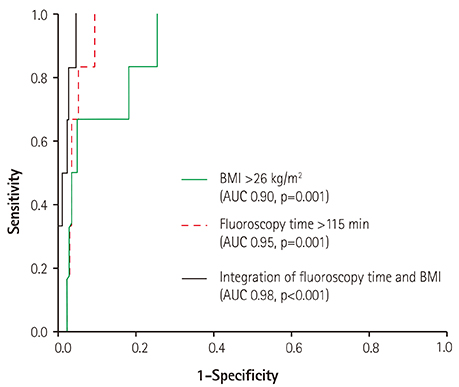
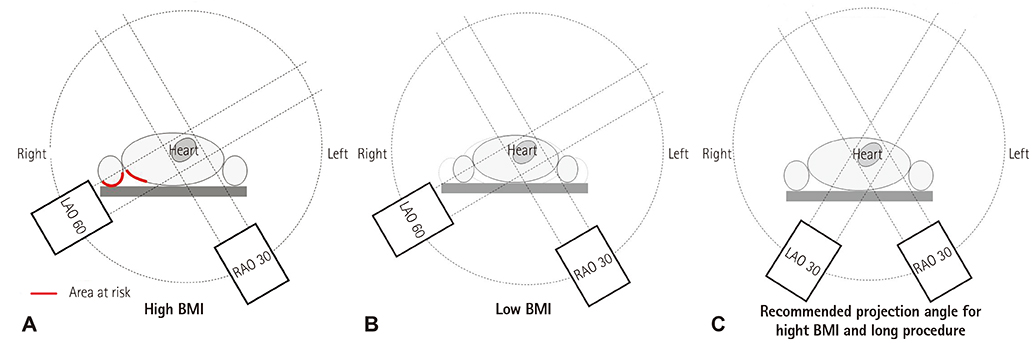
Of the 1347 enrolled patients, 12 (0.89%) experienced dermatologic issues within 1 month after RFCA, including six patients (0.45%) clinically classified as 'most likely RID' and four patients (0.30%) with 'probable RID'. Ten patients, including most likely RID or probable RID patients, developed skin lesions on the right back and upper arm. Skin lesions did not improve without meticulous treatment, and three cases required surgical intervention. We compared the RID group to the remaining 1335 patients (normal group). The mean body mass indices (BMIs) of the RID and normal groups were 29.3 and 23.9 kg/m², respectively (p<0.001). Radiation exposure times were longer in the RID group (180±31.0 vs. 47±49.9 minutes, p<0.001). We further analyzed 44 patients (6 RID cases and 38 normal patients) that had BMIs >26 kg/m2 and exposure times >115 minutes based on receiver operator characteristic curve analyses. Among the 35 patients without RID, 29 patients (82.9%) did not use biplane fluoroscopy.
CONCLUSIONS
Patients with high BMIs have a higher risk of developing severe RID with increasing fluoroscopy times using biplane fluoroscopy.
Keyword
MeSH Terms
Figure
Reference
-
1. Weiss EM, Thabit O. Clinical considerations for allied professionals: radiation safety and protection in the electrophysiology lab. Heart Rhythm. 2007; 4:1583–1587.2. Heidbuchel H, Wittkampf FH, Vano E, et al. Practical ways to reduce radiation dose for patients and staff during device implantations and electrophysiological procedures. Europace. 2014; 16:946–964.3. Koenig TR, Mettler FA, Wagner LK. Skin injuries from fluoroscopically guided procedures: part 2, review of 73 cases and recommendations for minimizing dose delivered to patient. AJR Am J Roentgenol. 2001; 177:13–20.4. Koenig TR, Wolff D, Mettler FA, Wagner LK. Skin injuries from fluoroscopically guided procedures: part 1, characteristics of radiation injury. AJR Am J Roentgenol. 2001; 177:3–11.5. Park TH, Eichling JO, Schechtman KB, Bromberg BI, Smith JM, Lindsay BD. Risk of radiation induced skin injuries from arrhythmia ablation procedures. Pacing Clin Electrophysiol. 1996; 19:1363–1369.6. Rosenthal LS, Mahesh M, Beck TJ, et al. Predictors of fluoroscopy time and estimated radiation exposure during radiofrequency catheter ablation procedures. Am J Cardiol. 1998; 82:451–458.7. Lindsay BD, Eichling JO, Ambos HD, Cain ME. Radiation exposure to patients and medical personnel during radiofrequency catheter ablation for supraventricular tachycardia. Am J Cardiol. 1992; 70:218–223.8. Vañó E, Arranz L, Sastre JM, et al. Dosimetric and radiation protection considerations based on some cases of patient skin injuries in interventional cardiology. Br J Radiol. 1998; 71:510–516.9. Glazier JJ, Dixon SR. Skin injury following prolonged fluoroscopy: early and late appearances. QJM. 2012; 105:571–573.10. Nahass GT. Acute radiodermatitis after radiofrequency catheter ablation. J Am Acad Dermatol. 1997; 36:881–884.11. Rosenthal LS, Beck TJ, Williams J, et al. Acute radiation dermatitis following radiofrequency catheter ablation of atrioventricular nodal reentrant tachycardia. Pacing Clin Electrophysiol. 1997; 20:1834–1839.12. Vlietstra RE, Wagner LK, Koenig T, Mettler F. Radiation burns as a severe complication of fluoroscopically guided cardiological interventions. J Interv Cardiol. 2004; 17:131–142.13. Wagner L. Radiation injury is a potentially serious complication to fluoroscopically-guided complex interventions. Biomed Imaging Interv J. 2007; 3:e22.14. Shope TB. Radiation-induced skin injuries from fluoroscopy. Radiographics. 1996; 16:1195–1199.15. Wagner LK, Eifel PJ, Geise RA. Potential biological effects following high X-ray dose interventional procedures. J Vasc Interv Radiol. 1994; 5:71–84.16. Mettler FA Jr, Koenig TR, Wagner LK, Kelsey CA. Radiation injuries after fluoroscopic procedures. Semin Ultrasound CT MR. 2002; 23:428–442.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Chronic Radiodermatitis following Radiofrequency Catheter Ablation for Atrial Fibrillation
- V-Y Latissimus Dorsi Musculocutaneous Flap for Reconstruction of Radiation-induced Skin Injuries on the Back
- Successful Management of Atrio-Esophageal Fistula after Cardiac Radiofrequency Catheter Ablation
- Successful Treatment of Tachycardia-induced Cardiomyopathy with Radiofrequency Catheter Ablation
- Characteristics of Intracardiac Electrogram at Successful Sites of Radiofrequency Catheter Ablation in Patients with Accessory Pathways