J Korean Soc Spine Surg.
2017 Jun;24(2):121-128. 10.4184/jkss.2017.24.2.121.
Idiopathic Spinal Cord Herniation
- Affiliations
-
- 1Department of Orthopedic Surgery, Haeundae-Paik Hospital, College of Medicine, Inje University, Busan, Korea. sskim@paik.ac.kr
- KMID: 2385649
- DOI: http://doi.org/10.4184/jkss.2017.24.2.121
Abstract
- STUDY DESIGN: Literature review.
OBJECTIVES
The aim of this study was to provide insight into idiopathic spinal cord herniation (ISCH) in terms of clinical presentation, pathophysiology, diagnosis, classification, and treatment. SUMMARY OF LITERATURE REVIEW: ISCH is a rare disorder characterized by anterior displacement of the spinal cord through a ventral dural defect. It has increasingly been recognized and described over the past 10 years.
MATERIALS AND METHODS
Review of the English-language literature on ISCH.
RESULTS
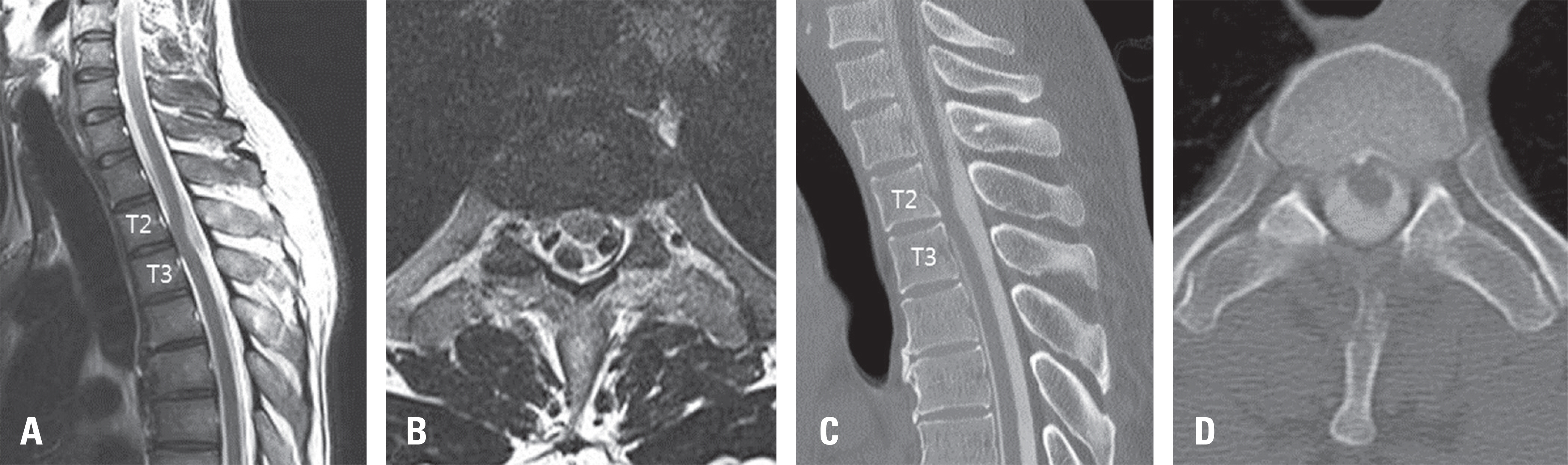
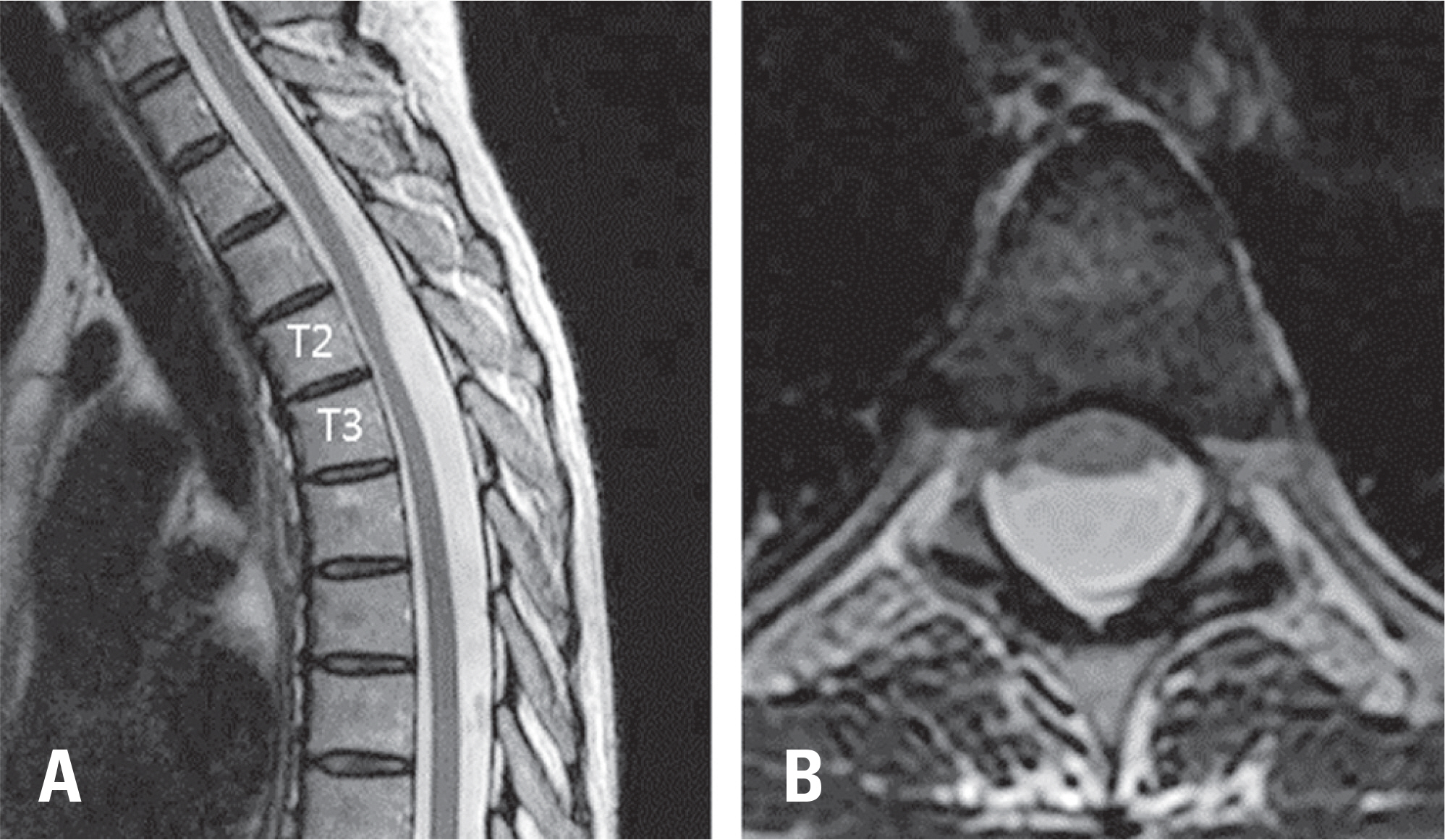
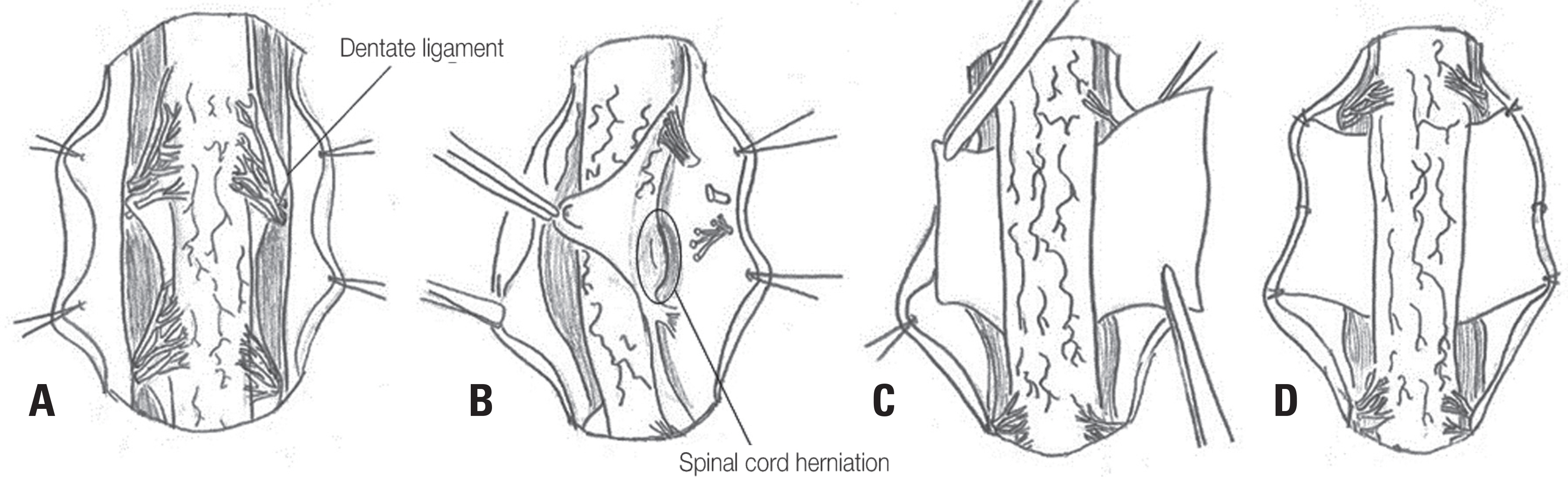
ISCH occurs in middle-aged adults with a female preponderance. The most common clinical presentation is Brown-Sequard syndrome, which can progress to spastic paraparesis. Its pathophysiology is unknown. However, some authors proposed that inflammation may play an important role in the emergence of a dural defect. Magnetic resonance imaging typically shows an anterior kink of the thoracic spinal cord with an obliteration of the ventral subarachnoid space and the widened dorsal subarachnoid space. Surgery is generally recommended for patients with motor deficits or progressive neurological symptoms. The posterior approach has been used because it allows wide exposure of the spinal cord. The surgical treatment of ISCH consists of spinal cord reduction from the ventral dural defect, which can be managed with enlargement, direct repair, or duraplasty (dural repair with a patch). In recent years, duraplasty has been used more frequently than enlargement of the dural defect.
CONCLUSIONS
ISCH causing thoracic myelopathy could be safely treated with surgical management. The possibility of this disease should be kept in mind when treating patients with progressive myelopathy.
MeSH Terms
Figure
Reference
-
1. Wortzman G, Tasker RR, Rewcastle NB, et al. Spontaneous incarcerated herniation of the spinal cord into a vertebral body: A unique cause of paraplegia. case report. J Neurosurg. 1974; 41:631–5.2. Darbar A, Krishnamurthy S, Holsapple JW, et al. Ventral thoracic spinal cord herniation: Frequently misdiagnosed entity. Spine (Phila Pa 1976). 2006; 31:E600–5.3. Chaichana KL, Sciubba DM, Li KW, et al. Surgical management of thoracic spinal cord herniation: Technical con-sideration. J Spinal Disord Tech. 2009; 22:67–72.4. Groen RJ, Middel B, Meilof JF, et al. Operative treatment of anterior thoracic spinal cord herniation: Three new cases and an individual patient data meta-analysis of 126 case reports. Neurosurgery. 2009; 64(Suppl):145–59.
Article5. Sasani M, Ozer AF, Vural M, et al. Idiopathic spinal cord herniation: Case report and review of the literature. J Spinal Cord Med. 2009; 32:86–94.
Article6. Shin JH, Krishnaney AA. Idiopathic ventral spinal cord herniation: A rare presentation of tethered cord. Neurosurg Focus. 2010; 29:E10.
Article7. Prada F, Saladino A, Giombini S, et al. Spinal cord herniation: Management and outcome in a series of 12 consecutive patients and review of the literature. Acta Neurochir (Wien). 2012; 154:723–30.8. Payer M, Zumsteg D, De Tribolet N, et al. Surgical management of thoracic idiopathic spinal cord herniation. technical case report and review. Acta Neurochir (Wien). 2016; 158:1579–82.
Article9. Nakazawa H, Toyama Y, Satomi K, et al. Idiopathic spinal cord herniation. report of two cases and review of the literature. Spine (Phila Pa 1976). 1993; 18:2138–41.10. Najjar MW, Baeesa SS, Lingawi SS. Idiopathic spinal cord herniation: A new theory of pathogenesis. Surg Neurol. 2004; 62:161–70.
Article11. Borges LF, Zervas NT, Lehrich JR. Idiopathic spinal cord herniation: A treatable cause of the Brown-Sequard syndrome: case report. Neurosurgery. 1995; 36:1028–32.12. Haber MD, Nguyen DD, Li S. Differentiation of idiopathic spinal cord herniation from CSF-isointense intraspinal extramedullary lesions displacing the cord. Radiographics. 2014; 34:313–29.
Article13. Barrenechea IJ, Lesser JB, Gidekel AL, et al. Diagnosis and treatment of spinal cord herniation: A combined experience. J Neurosurg Spine. 2006; 5:294–302.
Article14. Imagama S, Matsuyama Y, Sakai Y, et al. Image classification of idiopathic spinal cord herniation based on symptom severity and surgical outcome: A multicenter study. J Neurosurg Spine. 2009; 11:310–9.
Article15. Massicotte EM, Montanera W, Ross Fleming JF, et al. Idiopathic spinal cord herniation: Report of eight cases and review of the literature. Spine (Phila Pa 1976). 2002; 27:E233–41.16. Summers JC, Balasubramani YV, Chan PC, et al. Idiopathic spinal cord herniation: Clinical review and report of three cases. Asian J Neurosurg. 2013; 8:97–105.
Article17. Samuel N, Goldstein CL, Santaguida C, et al. Spontaneous resolution of idiopathic thoracic spinal cord herniation: Case report. J Neurosurg Spine. 2015; 23:306–8.
Article18. Watanabe M, Chiba K, Matsumoto M, et al. Surgical management of idiopathic spinal cord herniation: A review of nine cases treated by the enlargement of the dural defect. J Neurosurg. 2001; 95(Suppl):169–72.
Article19. Nakamura M, Fujiyoshi K, Tsuji O, et al. Longterm surgical outcomes of idiopathic spinal cord herniation. J Orthop Sci. 2011; 16:347–51.
Article20. Inoue T, Cohen-Gadol AA, Krauss WE. Low-pressure headaches and spinal cord herniation. case report. J Neurosurg. 2003; 98(Suppl):93–5.21. Akutsu H, Takada T, Nakai K, et al. Surgical technique for idiopathic spinal cord herniation: The hammock method. technical note. Neurol Med Chir (Tokyo). 2012; 52:238–42.22. Batzdorf U, Holly LT. Idiopathic thoracic spinal cord herniation: Report of 10 patients and description of surgical approach. J Spinal Disord Tech. 2012; 25:157–62.23. Novak K, Widhalm G, de Camargo AB, et al. The value of intraoperative motor evoked potential monitoring during surgical intervention for thoracic idiopathic spinal cord her-niation. J Neurosurg Spine. 2012; 16:114–26.
Article24. Saito T, Anamizu Y, Nakamura K, et al. Case of idiopathic thoracic spinal cord herniation with a chronic history: A case report and review of the literature. J Orthop Sci. 2004; 9:94–8.
Article25. Maira G, Denaro L, Doglietto F, et al. Idiopathic spinal cord herniation: Diagnostic, surgical, and follow-up data obtained in five cases. J Neurosurg Spine. 2006; 4:10–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Idiopathic Spinal Cord Herniation Presented as Brown-Sequard Syndrome: A Case Report and Surgical Outcome
- Unilateral Paramedian Transpedicular Approach for Repair of Anterior Transdural Spinal Cord Herniation: Report of a Case and Literature Review
- Idiopathic Spinal Cord Herniation as a Treatable Cause of Progressive Brown-Sequard Syndrome
- Spontaneous Herniation of the Thoracic Spinal Cord: A Case Report
- Idiopathic Spinal Cord Herniation at Thoracic Spine Level: A Case Report