Intest Res.
2017 Jul;15(3):380-387. 10.5217/ir.2017.15.3.380.
Ophthalmologic manifestations in patients with inflammatory bowel disease
- Affiliations
-
- 1Department of Ophthalmology, Jeju National University School of Medicine, Jeju, Korea.
- 2Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea. songhj@jejunu.ac.kr
- KMID: 2382382
- DOI: http://doi.org/10.5217/ir.2017.15.3.380
Abstract
- BACKGROUND/AIMS
Inflammatory bowel disease (IBD), including Crohn's disease (CD) and ulcerative colitis (UC), has been reported to have various ophthalmologic manifestations. The aim of this study was to evaluate the prevalence of ophthalmologic manifestations associated with IBD in Korea.
METHODS
Sixty-one patients were examined between May 2013 and October 2014. We performed complete ophthalmologic examinations.
RESULTS
Findings included 36 patients with CD and 25 with UC. The mean age of the patients was 34±16 years and disease duration was 45.3±23.9 months. Ophthalmologic manifestations were positive in 44 cases. Primary complication was diagnosed in 5 cases, as follows; iritis in 2 cases, episcleritis in one case, iritis with optic neuritis in 1 case, and serous retinal detachment in 1 case, without secondary complications. The most common coincidental complication was dry eye syndrome (DES), in 35 patients (57.4%). The prevalence of DES in the control group was 21.3%. The proportion of DES in patients with IBD was significantly higher than in the control group (P=0.002).
CONCLUSIONS
Ophthalmologic manifestations were high (72.1%) in IBD patients. Clinically significant primary ocular inflammation occurred in 8.2% of patients. The most common complication was DES. There was a higher rate of DES in patients with IBD compared to the control group. Evaluation of the eye should be a routine component in patients with IBD.
Keyword
MeSH Terms
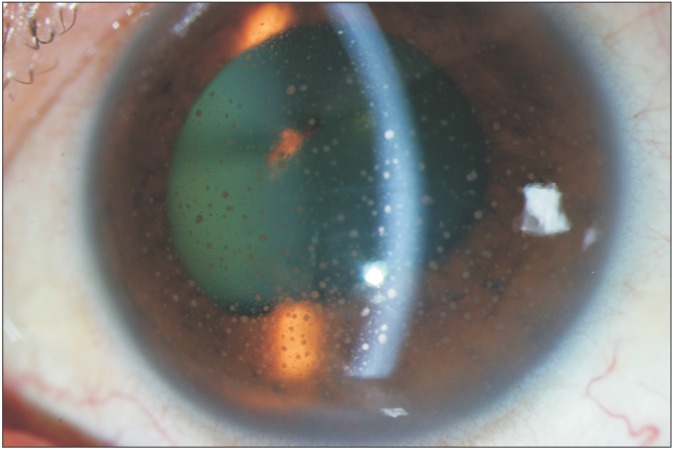
Figure
Cited by 1 articles
-
The optimal time to perform an ophthalmic examination of patients with inflammatory bowel disease
Ana Luiza Biancardi, Leandro Lopes Troncoso, Haroldo Vieira de Moraes Jr, Cyrla Zaltman
Intest Res. 2019;17(1):153-154. doi: 10.5217/ir.2018.00147.
Reference
-
1. Ernst BB, Lowder CY, Meisler DM, Gutman FA. Posterior segment manifestations of inflammatory bowel disease. Ophthalmology. 1991; 98:1272–1280. PMID: 1923366.
Article2. Knox DL, Schachat AP, Mustonen E. Primary, secondary and coincidental ocular complications of Crohn's disease. Ophthalmology. 1984; 91:163–173. PMID: 6538677.
Article3. Hu PJ. Inflammatory bowel disease in Asia: the challenges and opportunities. Intest Res. 2015; 13:188–190. PMID: 26130991.
Article4. Lee JW, Im JP, Cheon JH, Kim YS, Kim JS, Han DS. Inflammatory bowel disease cohort studies in Korea: present and future. Intest Res. 2015; 13:213–218. PMID: 26130995.
Article5. Ghanchi FD, Rembacken BJ. Inflammatory bowel disease and the eye. Surv Ophthalmol. 2003; 48:663–676. PMID: 14609712.
Article6. Felekis T, Katsanos K, Kitsanou M, et al. Spectrum and frequency of ophthalmologic manifestations in patients with inflammatory bowel disease: a prospective single-center study. Inflamm Bowel Dis. 2009; 15:29–34. PMID: 18626979.
Article7. Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015; 21:1982–1992. PMID: 26154136.
Article8. Thomas AS, Lin P. Ocular manifestations of inflammatory bowel disease. Curr Opin Ophthalmol. 2016; 27:552–560. PMID: 27585211.
Article9. Taylor SR, McCluskey P, Lightman S. The ocular manifestations of inflammatory bowel disease. Curr Opin Ophthalmol. 2006; 17:538–544. PMID: 17065922.
Article10. Winship DH, Summers RW, Singleton JW, et al. National Cooperative Crohn's Disease Study: study design and conduct of the study. Gastroenterology. 1979; 77(4 Pt 2):829–842. PMID: 38175.
Article11. Sostegni R, Daperno M, Scaglione N, Lavagna A, Rocca R, Pera A. Review article: Crohn's disease: monitoring disease activity. Aliment Pharmacol Ther. 2003; 17(Suppl 2):11–17. PMID: 12786607.12. D'Haens G, Sandborn WJ, Feagan BG, et al. A review of activity indices and efficacy end points for clinical trials of medical therapy in adults with ulcerative colitis. Gastroenterology. 2007; 132:763–786. PMID: 17258735.13. Lewis JD, Chuai S, Nessel L, Lichtenstein GR, Aberra FN, Ellenberg JH. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008; 14:1660–1666. PMID: 18623174.
Article14. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003; 22:640–650. PMID: 14508260.
Article15. Hyon JY, Kim HM, Lee D, et al. Korean guidelines for the diagnosis and management of dry eye: development and validation of clinical efficacy. Korean J Ophthalmol. 2014; 28:197–206. PMID: 24882952.
Article16. Cury DB, Moss AC. Ocular manifestations in a community-based cohort of patients with inflammatory bowel disease. Inflamm Bowel Dis. 2010; 16:1393–1396. PMID: 19998457.
Article17. Kim ES, Kim WH. Inflammatory bowel disease in Korea: epidemiological, genomic, clinical, and therapeutic characteristics. Gut Liver. 2010; 4:1–14. PMID: 20479907.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dermatologic Manifestations in Inflammatory Bowel Disease
- Renal and Urinary Manifestations of Inflammatory Bowel Disease
- Ophthalmologic Manifestation of Inflammatory Bowel Disease: A Review
- Inflammatory Bowel Disease in Pediatric Age
- Pathogenesis and clinical perspectives of extraintestinal manifestations in inflammatory bowel diseases