Korean J Gastroenterol.
2019 May;73(5):269-275. 10.4166/kjg.2019.73.5.269.
Ophthalmologic Manifestation of Inflammatory Bowel Disease: A Review
- Affiliations
-
- 1Department of Ophthalmology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. minkim76@gmail.com
- 2Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2447596
- DOI: http://doi.org/10.4166/kjg.2019.73.5.269
Abstract
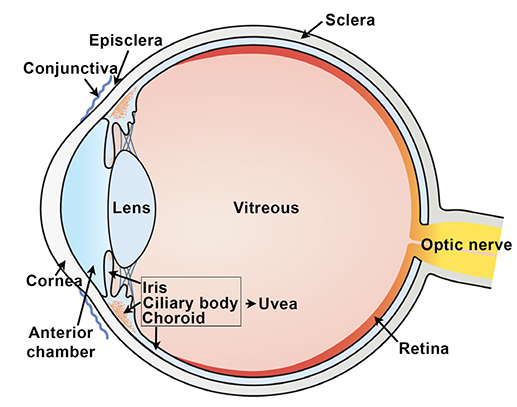
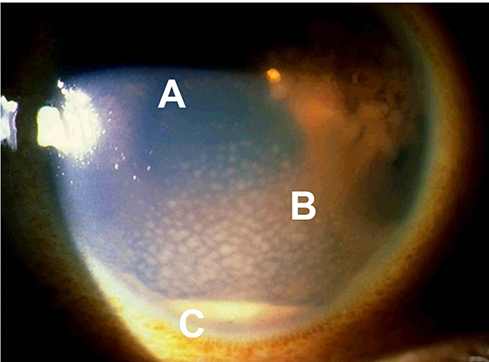
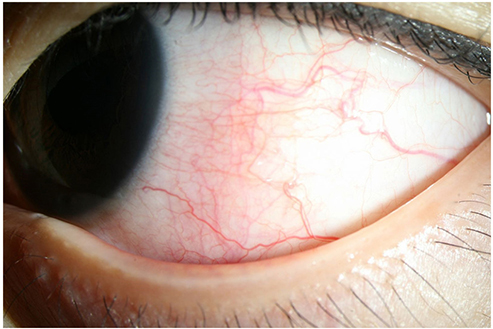
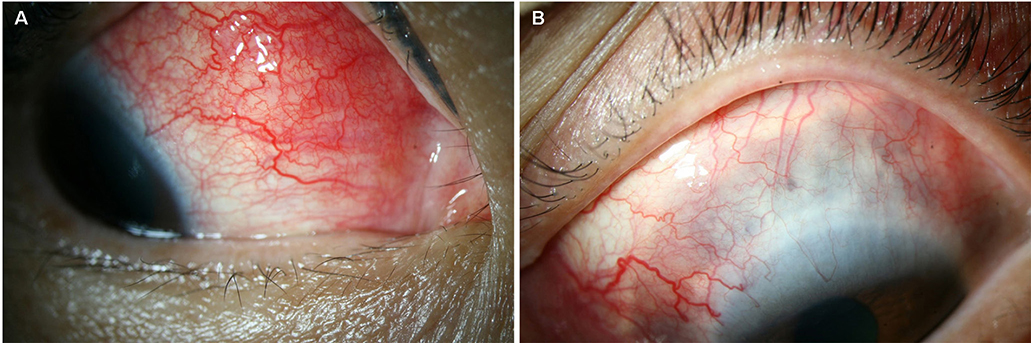
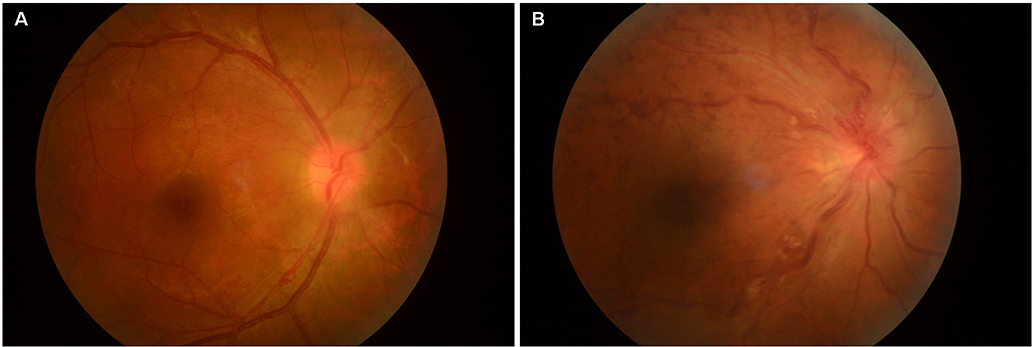
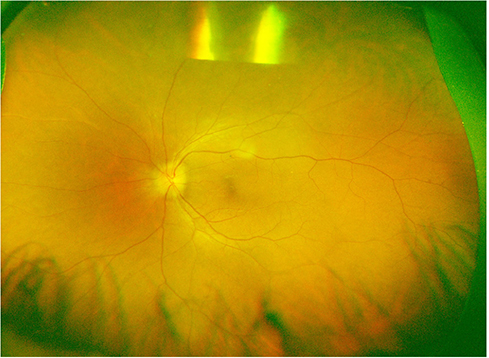
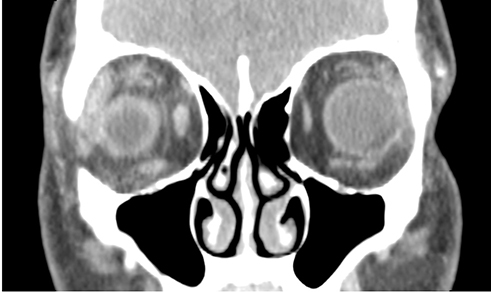
- In patients with inflammatory bowel disease (IBD), ocular extraintestinal manifestations (EIM) are less common than EIM of other systems, but they are clinically important because they can lead to complications that can cause catastrophic damage to the visual acuity and ocular structure. Anterior uveitis and episcleritis are the most common ocular EIM. Involvement of the orbit, posterior segment, and optic nerve can also occur. A variety of treatments are available ranging from topical steroids to systemic immunosuppressive therapies. The treatment of IBD is also essential if the activity of inflammatory bowel disease affects the ocular symptoms.
MeSH Terms
Figure
Reference
-
1. Silva FA, Rodrigues BL, Ayrizono ML, Leal RF. The immunological basis of inflammatory bowel disease. Gastroenterol Res Pract. 2016; 2016:2097274.
Article2. Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018; 390:2769–2778.
Article3. Jung YS, Han M, Kim WH, Park S, Cheon JH. Incidence and clinical outcomes of inflammatory bowel disease in South Korea, 2011–2014: a nationwide population-based study. Dig Dis Sci. 2017; 62:2102–2112.
Article4. Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015; 21:1982–1992.
Article5. Das KM. Relationship of extraintestinal involvements in inflammatory bowel disease: new insights into autoimmune pathogenesis. Dig Dis Sci. 1999; 44:1–13.6. Lees CW, Barrett JC, Parkes M, Satsangi J. New IBD genetics: common pathways with other diseases. Gut. 2011; 60:1739–1753.
Article7. Vavricka SR, Brun L, Ballabeni P, et al. Frequency and risk factors for extraintestinal manifestations in the Swiss inflammatory bowel disease cohort. Am J Gastroenterol. 2011; 106:110–119.
Article8. Harbord M, Annese V, Vavricka SR, et al. The first European evidence-based consensus on extra-intestinal manifestations in inflammatory bowel disease. J Crohns Colitis. 2016; 10:239–254.
Article9. Bernstein CN, Blanchard JF, Rawsthorne P, Yu N. The prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study. Am J Gastroenterol. 2001; 96:1116–1122.
Article10. Levine JS, Burakoff R. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2011; 7:235–241.11. Li YC, Li WZ, Wu CR, et al. Prevalence and characteristics of ophthalmological extra-intestinal manifestations in Chinese patients with inflammatory bowel disease. Int J Ophthalmol. 2016; 9:1476–1479.
Article12. Peyrin-Biroulet L, Van Assche G, Gómez-Ulloa D, et al. Systematic review of tumor necrosis factor antagonists in extraintestinal manifestations in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2017; 15:25–36.e27.
Article13. Yang BR, Choi NK, Kim MS, et al. Prevalence of extraintestinal manifestations in Korean inflammatory bowel disease patients. PLoS One. 2018; 13:e0200363.
Article14. Salmon JF, Wright JP, Murray AD. Ocular inflammation in Crohn's disease. Ophthalmology. 1991; 98:480–484.
Article15. Karmiris K, Avgerinos A, Tavernaraki A, et al. Prevalence and characteristics of extra-intestinal manifestations in a large cohort of Greek patients with inflammatory bowel disease. J Crohns Colitis. 2016; 10:429–436.
Article16. Bandyopadhyay D, Bandyopadhyay S, Ghosh P, et al. Extraintestinal manifestations in inflammatory bowel disease: prevalence and predictors in Indian patients. Indian J Gastroenterol. 2015; 34:387–394.17. Zippi M, Corrado C, Pica R, et al. Extraintestinal manifestations in a large series of Italian inflammatory bowel disease patients. World J Gastroenterol. 2014; 20:17463–17467.
Article18. Mendoza JL, Lana R, Taxonera C, Alba C, Izquierdo S, Díaz-Rubio M. Extraintestinal manifestations in inflammatory bowel disease: differences between Crohn's disease and ulcerative colitis. Med Clin (Barc). 2005; 125:297–300.19. Lakatos L, Pandur T, David G, et al. Association of extraintestinal manifestations of inflammatory bowel disease in a province of western Hungary with disease phenotype: results of a 25-year follow-up study. World J Gastroenterol. 2003; 9:2300–2307.
Article20. Christodoulou DK, Katsanos KH, Kitsanou M, Stergiopoulou C, Hatzis J, Tsianos EV. Frequency of extraintestinal manifestations in patients with inflammatory bowel disease in Northwest Greece and review of the literature. Dig Liver Dis. 2002; 34:781–786.
Article21. Lanna CC, Ferrari Mde L, Rocha SL, Nascimento E, de Carvalho MA, da Cunha AS. A cross-sectional study of 130 Brazilian patients with Crohn's disease and ulcerative colitis: analysis of articular and ophthalmologic manifestations. Clin Rheumatol. 2008; 27:503–509.
Article22. Nakayama LF, Bergamo VC, Conti ML, Costa LA, Moraes NSB, Ambrogini O Jr. Frequency of ophthalmological posterior segment findings in patients with inflammatory bowel disease. Arq Gastroenterol. 2018; 55:188–191.
Article23. Ernst BB, Lowder CY, Meisler DM, Gutman FA. Posterior segment manifestations of inflammatory bowel disease. Ophthalmology. 1991; 98:1272–1280.
Article24. Ghanchi FD, Rembacken BJ. Inflammatory bowel disease and the eye. Surv Ophthalmol. 2003; 48:663–676.
Article25. Felekis T, Katsanos K, Kitsanou M, et al. Spectrum and frequency of ophthalmologic manifestations in patients with inflammatory bowel disease: a prospective single-center study. Inflamm Bowel Dis. 2009; 15:29–34.
Article26. Gueudry J, Muraine M. Anterior uveitis. J Fr Ophtalmol. 2018; 41:e11–e21.
Article27. Orchard TR, Chua CN, Ahmad T, Cheng H, Welsh KI, Jewell DP. Uveitis and erythema nodosum in inflammatory bowel disease: clinical features and the role of HLA genes. Gastroenterology. 2002; 123:714–718.
Article28. Pasadhika S, Rosenbaum JT. Update on the use of systemic biologic agents in the treatment of noninfectious uveitis. Biologics. 2014; 8:67–81.29. Williams H, Walker D, Orchard TR. Extraintestinal manifestations of inflammatory bowel disease. Curr Gastroenterol Rep. 2008; 10:597–605.
Article30. Paroli MP, Spinucci G, Bruscolini A, La Cava M, Abicca I. Uveitis preceding Crohn's disease by 8 years. Int Ophthalmol. 2011; 31:413–415.31. Mielants H, Veys EM, Goemaere S, Cuvelier C, De Vos M. A prospective study of patients with spondyloarthropathy with special reference to HLA-B27 and to gut histology. J Rheumatol. 1993; 20:1353–1358.32. Thach AB, Dugel PU, Flindall RJ, Sipperley JO, Sneed SR. A comparison of retrobulbar versus sub-Tenon's corticosteroid therapy for cystoid macular edema refractory to topical medications. Ophthalmology. 1997; 104:2003–2008.
Article33. Patil SA, Cross RK. Update in the management of extraintestinal manifestations of inflammatory bowel disease. Curr Gastroenterol Rep. 2013; 15:314.
Article34. Kaplan-Messas A, Barkana Y, Avni I, Neumann R. Methotrexate as a first-line corticosteroid-sparing therapy in a cohort of uveitis and scleritis. Ocul Immunol Inflamm. 2003; 11:131–139.
Article35. Mady R, Grover W, Butrus S. Ocular complications of inflammatory bowel disease. ScientificWorldJournal. 2015; 2015:438402.
Article36. Muñoz-Fernández S, Hidalgo V, Fernández-Melón J, et al. Sulfasalazine reduces the number of flares of acute anterior uveitis over a one-year period. J Rheumatol. 2003; 30:1277–1279.37. Magro F, Portela F. Management of inflammatory bowel disease with infliximab and other anti-tumor necrosis factor alpha therapies. BioDrugs. 2010; 24:Suppl 1. 3–14.
Article38. Yilmaz S, Aydemir E, Maden A, Unsal B. The prevalence of ocular involvement in patients with inflammatory bowel disease. Int J Colorectal Dis. 2007; 22:1027–1030.
Article39. Generali E, Cantarini L, Selmi C. Ocular involvement in systemic autoimmune diseases. Clin Rev Allergy Immunol. 2015; 49:263–270.
Article40. Thomas AS, Lin P. Ocular manifestations of inflammatory bowel disease. Curr Opin Ophthalmol. 2016; 27:552–560.
Article41. Jabs DA, Mudun A, Dunn JP, Marsh MJ. Episcleritis and scleritis: clinical features and treatment results. Am J Ophthalmol. 2000; 130:469–476.
Article42. Cunningham ET Jr, McCluskey P, Pavesio C, Wakefield D, Zierhut M. Scleritis. Ocul Immunol Inflamm. 2016; 24:2–5.
Article43. Watson PG, Young RD. Scleral structure, organisation and disease. A review. Exp Eye Res. 2004; 78:609–623.
Article44. Culver EL, Salmon JF, Frith P, Travis SP. Recurrent posterior scleritis and orbital myositis as extra-intestinal manifestations of Crohn's disease: case report and systematic literature review. J Crohns Colitis. 2008; 2:337–342.
Article45. de Fidelix TS, Vieira LA, de Freitas D, Trevisani VF. Biologic therapy for refractory scleritis: a new treatment perspective. Int Ophthalmol. 2015; 35:903–912.
Article46. Ragam A, Kolomeyer AM, Fang C, Xu Y, Chu DS. Treatment of chronic, noninfectious, nonnecrotizing scleritis with tumor necrosis factor alpha inhibitors. Ocul Immunol Inflamm. 2014; 22:469–477.
Article47. Tappeiner C, Dohrmann J, Spital G, Heiligenhaus A. Multifocal posterior uveitis in Crohn's disease. Graefes Arch Clin Exp Ophthalmol. 2007; 245:457–459.
Article48. Matsuo T, Yamaoka A. Retinal vasculitis revealed by fluorescein angiography in patients with inflammatory bowel disease. Jpn J Ophthalmol. 1998; 42:398–400.
Article49. Vianna RN, Ozdal PC, Deschénes J. Multifocal choroiditis--an unusual finding in Crohn's disease. Eur J Ophthalmol. 2004; 14:345–349.50. Mason JO 3rd. Bilateral phakic cystoid macular edema associated with Crohn's disease. South Med J. 2002; 95:1079–1080.
Article51. Ishihara K, Tsujikawa A, Yodoi Y, Kameda T, Yoshimura N. Choroidal neovascularization in a patient with ulcerative colitis. Jpn J Ophthalmol. 2008; 52:515–518.
Article52. Seo Y, Kim M, Kim JH, Park JJ, Lee SC. Central retinal vein occlusion associated with ulcerative colitis. Optom Vis Sci. 2016; 93:1567–1570.
Article53. Sedwick LA, Klingele TG, Burde RM, Behrens MM. Optic neuritis in inflammatory bowel disease. J Clin Neuroophthalmol. 1984; 4:3–6.54. Hutnik CM, Nicolle DA, Canny CL. Papillitis: a rare initial presentation of Crohn's disease. Can J Ophthalmol. 1996; 31:373–376.55. Katsanos A, Asproudis I, Katsanos KH, Dastiridou AI, Aspiotis M, Tsianos EV. Orbital and optic nerve complications of inflammatory bowel disease. J Crohns Colitis. 2013; 7:683–693.
Article56. Hwang IP, Jordan DR, Acharya V. Lacrimal gland inflammation as the presenting sign of Crohn's disease. Can J Ophthalmol. 2001; 36:212–213.
Article57. Fine S, Nee J, Thakuria P, Duff B, Farraye FA, Shah SA. Ocular, auricular, and oral manifestations of inflammatory bowel disease. Dig Dis Sci. 2017; 62:3269–3279.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- How Should We Do Different Approach to Treat Inflammatory Bowel Disease by Gender Difference?
- Musculoskeletal Manifestation in Inflammatory Bowel Disease
- Abdominal Pain over 6 Months
- Ophthalmologic manifestations in patients with inflammatory bowel disease
- The Pharmacotherapy of Inflammatory Bowel Disease in Child and Adolescence