J Educ Eval Health Prof.
2014;11:26. 10.3352/jeehp.2014.11.26.
Assessment of professional competency and need of smoking cessation counseling for dental students
- Affiliations
-
- 1Department of Prosthodontics, Guardian College of Dental Sciences and Research Centre, Ambernath, India. rajnidable@gmail.com
- 2Department of Endodontics, SMBT Dental College and Hospital Amrutnagar, Sangamner, India.
- 3Department of Periodontics, Pravara Rural Dental College and Hospital Loni, Loni, India.
- 4Department of Prosthodontics, Dent Art Dental Hospital, Mumbai, India.
- 5Department of Orthodontics, SMBT Dental College and Hospital Amrutnagar, Sangamner, India.
- KMID: 2380945
- DOI: http://doi.org/10.3352/jeehp.2014.11.26
Abstract
- PURPOSE
The aim of this study was to analyze the smoking prevalence among dental students and to assess the need for promoting tobacco education and intervention by exploring their knowledge about smoking related risk factors. The study also examined the attitudes and practices of the students toward tobacco consumption, and their responsibilities toward the community.
METHODS
In total, 53 male students participated in the study (21 juniors and 32 seniors). The training program was divided into three modules, and the questionnaire was administered before and after the counseling sessions, which provided the comparative data on the students' views about smoking cessation.
RESULTS
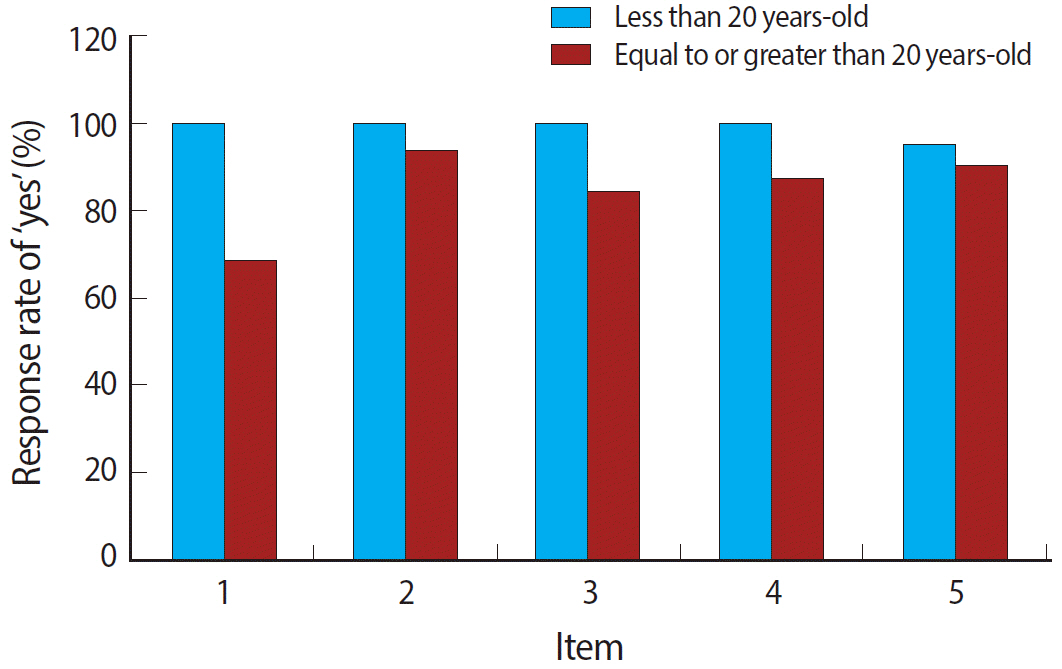
The most commonly practiced mode of tobacco consumption was found to be cigarette smoking (90.6%), while a few consumed Gutkha (9.4%). All the junior students (100%) reported to have been benefitted by the counseling program, while 68.8% of the students from the senior group reported the same. Bivariate statistical analysis was conducted using the Pearson's chi-square test for testing the difference across the age groups. P-values less than 0.05 were considered statistically significant.
CONCLUSION
Curbing tobacco influence on dental students in their initial days can ensure a smoke-free life for them, as well as prevents them from feeling embarrassed or experiencing a lack of confidence while seeing their patients. Thus, tobacco education and intervention programs can motivate the students and increase their potential to be credible advisors regarding smoking cessation.
Keyword
MeSH Terms
Figure
Reference
-
1. Ramakrishna GS, Sankara Sarma P, Thankappan KR. Tobacco use among medical students in Orissa. Natl Med J India. 2005; 18:285–289.2. Binnal A, Rajesh G, Denny C, Ahmed J. Insights into the tobacco cessation scenario among dental graduates: an Indian perspective. Asian Pac J Cancer Prev. 2012; 13:2611–2617. http://dx.doi.org/10.7314/apjcp.2012.13.6.2611.
Article3. Hashemi N. Prevalence of smoking and its causes in male students of Yasooj University of Medical Sciences. J Yasooj Univ Med Sci. 2001; 6:43–47.4. Alrsheedi M, Haleem A. Knowledge, attitude and behavior of medical and dental students towards smoking habit in Saudi Arabian universities, a comparative study. Int Dent J Stud Res [Internet]. 2012 [cited 2014 Aug 3]; 1:1–16. Available from: http://www.idjsr.com/uploads/1/1/3/3/11335549/article_5-_saudi.pdf.5. Merrill RM, Madanat HN, Cox E, Merrill JM. Perceived effectiveness of counselling patients about smoking among medical students in Amman, Jordan. East Mediterr Health J. 2009; 15:1180–1191.6. Kazmi F, Chaudhary MA, Mumtaz M, Bhatti MU, Khawaja N. Oral cancer knowledge and awareness amongst undergraduate dental students of Lahore: Pakistan. Pakistan Oral Dent J. 2011; 31:64–67.7. Fiore MC, Jaen CR, Baker TB. Treating tobacco use and dependence: 2008 update, clinical practice guideline. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service;2008.8. Uti OG, Sofola OO. Smoking cessation counseling in dentistry: attitudes of Nigerian dentists and dental students. J Dent Educ. 2011; 75:406–412.
Article9. Sinha DN, Rinchen S, Palipudi KM, Naing Shein NN, de Silva P, Khadka BB, Pednekar M, Singh G, Pitayarangsarit S, Bhattad VB. Tobacco use, exposure to second-hand smoke, and cessation training among the third-year medical and dental students in selected Member States of South-East Asia region: a trend analysis on data from the Global Health Professions Student Survey, 2005-2011. Indian J Cancer. 2012; 49:379–386. http://dx.doi.org/10.4103/0019-509X.107743.
Article10. Fotedar S, Sogi GM, Fotedar V, Bhushan B, Singh B, Dahiya P, Thakur AS. Knowledge of, attitude towards, and prevalence of tobacco use among dental students in Himachal Pradesh State, India. Oral Health Dent Manag. 2013; 12:73–79.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An assessment of smoking cessation counseling among dental hygienists
- Factors Affecting Smoking Cessation Success during 4-week Smoking Cessation Program for University Students
- Smoking Cessation Counselling Activity among Nurses in a Community
- Effect of Smoking Cessation Program for Workers in Large Size Company: Using Motivational Enhancement Counseling
- Influencing Factors on Smoking Cessation Motivation of Adult Males