Clin Endosc.
2015 Nov;48(6):542-548. 10.5946/ce.2015.48.6.542.
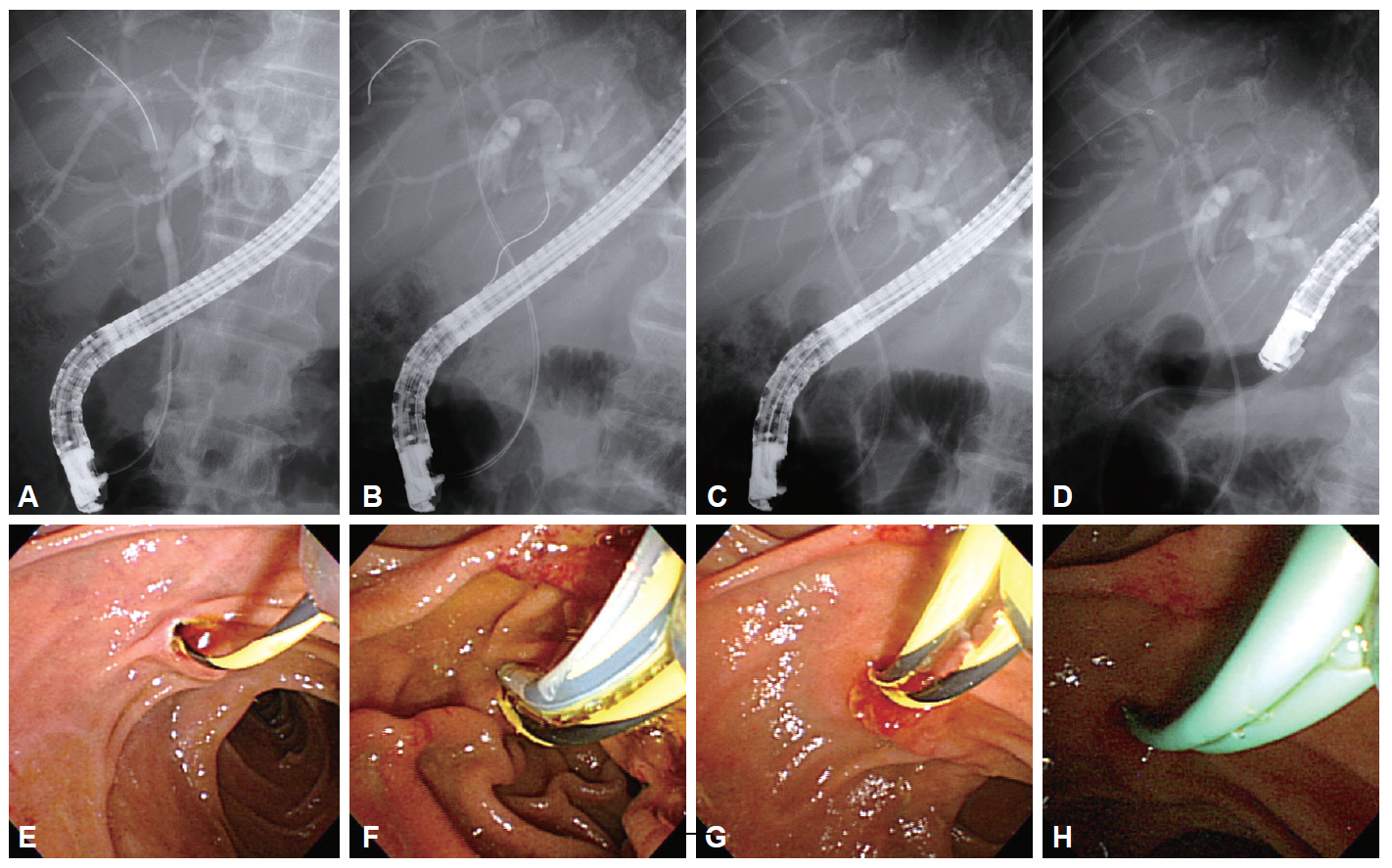
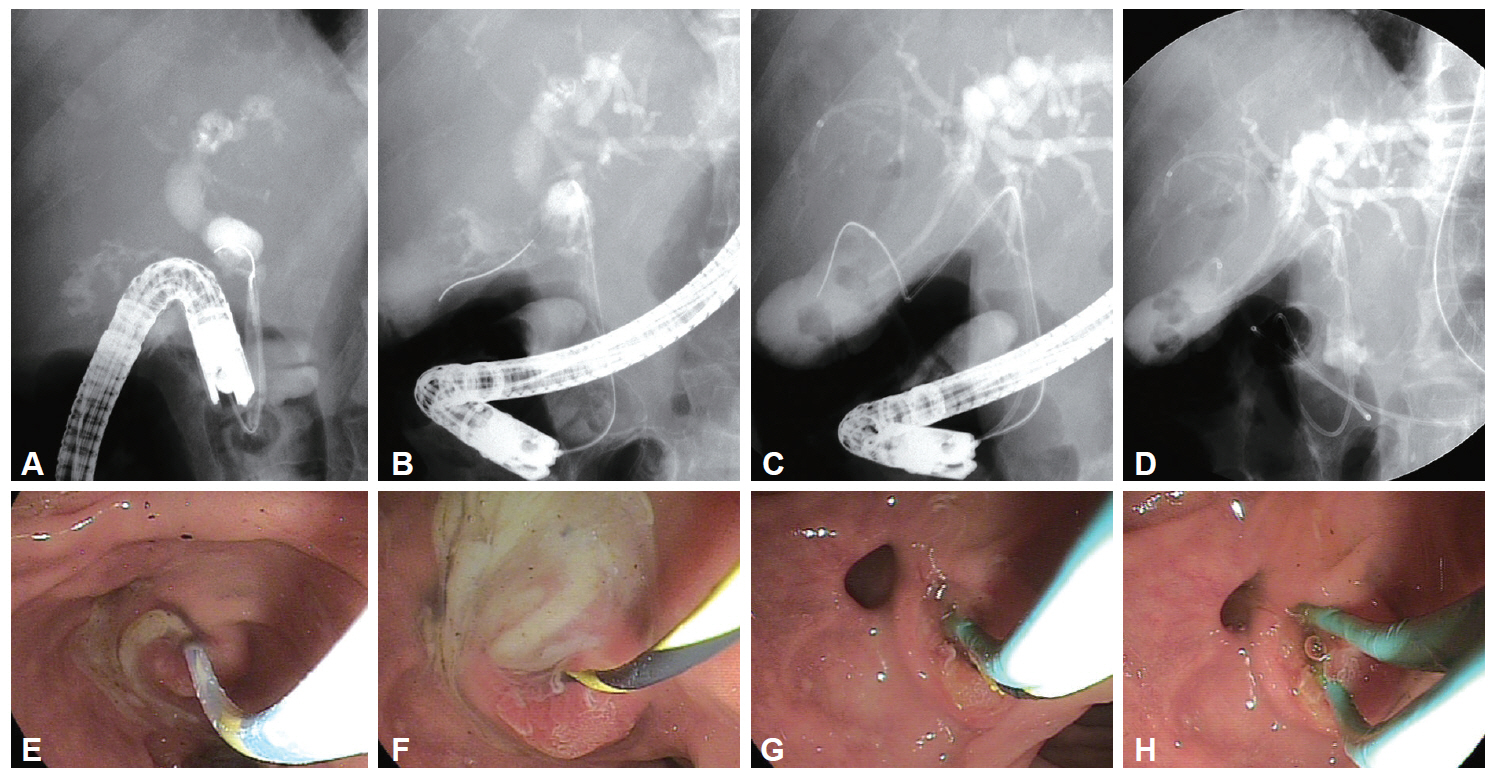
The Clinical Usefulness of Simultaneous Placement of Double Endoscopic Nasobiliary Biliary Drainage
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University School of Medicine, Jinju, Korea.
- 2Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sklee@amc.seoul.kr
- 3Department of Internal Medicine, Hanmaeum Hospital, Jeju, Korea.
- KMID: 2380413
- DOI: http://doi.org/10.5946/ce.2015.48.6.542
Abstract
- BACKGROUND/AIMS
To evaluate the technical feasibility and clinical efficacy of double endoscopic nasobiliary drainage (ENBD) as a new method of draining multiple bile duct obstructions.
METHODS
A total of 38 patients who underwent double ENBD between January 2004 and February 2010 at the Asan Medical Center were retrospectively analyzed. We evaluated indications, laboratory results, and the clinical course.
RESULTS
Of the 38 patients who underwent double ENBD, 20 (52.6%) had Klatskin tumors, 12 (31.6%) had hepatocellular carcinoma, 3 (7.9%) had strictures at the anastomotic site following liver transplantation, and 3 (7.9%) had acute cholecystitis combined with cholangitis. Double ENBD was performed to relieve multiple biliary obstruction in 21 patients (55.1%), drain contrast agent filled during endoscopic retrograde cholangiopancreatography in 4 (10.5%), obtain cholangiography in 4 (10.5%), drain hemobilia in 3 (7.9%), relieve Mirizzi syndrome with cholangitis in 3 (7.9%), and relieve jaundice in 3 (7.9%).
CONCLUSIONS
Double ENBD may be useful in patients with multiple biliary obstructions.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Can Endoscopic Nasobiliary Drainage Involving Two Catheters Be Used to Treat Various Conditions?
Dong Wook Lee, Ho Gak Kim
Clin Endosc. 2015;48(6):464-465. doi: 10.5946/ce.2015.48.6.464.
Reference
-
1. Sakata J, Shirai Y, Wakai T, Nomura T, Sakata E, Hatakeyama K. Catheter tract implantation metastases associated with percutaneous biliary drainage for extrahepatic cholangiocarcinoma. World J Gastroenterol. 2005; 11:7024–7027.
Article2. Laurent A, Tayar C, Cherqui D. Cholangiocarcinoma: preoperative biliary drainage (Con). HPB (Oxford). 2008; 10:126–129.
Article3. Park SY, Park CH, Cho SB, et al. The safety and effectiveness of endoscopic biliary decompression by plastic stent placement in acute suppurative cholangitis compared with nasobiliary drainage. Gastrointest Endosc. 2008; 68:1076–1080.
Article4. Arakura N, Takayama M, Ozaki Y, et al. Efficacy of preoperative endoscopic nasobiliary drainage for hilar cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 2009; 16:473–477.
Article5. Peng SY, Wang JW, Liu YB, et al. Surgical intervention for obstructive jaundice due to biliary tumor thrombus in hepatocellular carcinoma. World J Surg. 2004; 28:43–46.
Article6. Ikenaga N, Chijiiwa K, Otani K, Ohuchida J, Uchiyama S, Kondo K. Clinicopathologic characteristics of hepatocellular carcinoma with bile duct invasion. J Gastrointest Surg. 2009; 13:492–497.
Article7. Sherman S. Endoscopic drainage of malignant hilar obstruction: is one biliary stent enough or should we work to place two? Gastrointest Endosc. 2001; 53:681–684.
Article8. Freeman ML, Overby C. Selective MRCP and CT-targeted drainage of malignant hilar biliary obstruction with self-expanding metallic stents. Gastrointest Endosc. 2003; 58:41–49.
Article9. Kondo S, Hirano S, Ambo Y, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg. 2004; 240:95–101.10. Sakata J, Shirai Y, Tsuchiya Y, Wakai T, Nomura T, Hatakeyama K. Preoperative cholangitis independently increases in-hospital mortality after combined major hepatic and bile duct resection for hilar cholangiocarcinoma. Langenbecks Arch Surg. 2009; 394:1065–1072.
Article11. Sano T, Shimada K, Sakamoto Y, Yamamoto J, Yamasaki S, Kosuge T. One hundred two consecutive hepatobiliary resections for perihilar cholangiocarcinoma with zero mortality. Ann Surg. 2006; 244:240–247.
Article12. Kanai M, Nimura Y, Kamiya J, et al. Preoperative intrahepatic segmental cholangitis in patients with advanced carcinoma involving the hepatic hilus. Surgery. 1996; 119:498–504.
Article13. Kawakami H, Kuwatani M, Onodera M, et al. Endoscopic nasobiliary drainage is the most suitable preoperative biliary drainage method in the management of patients with hilar cholangiocarcinoma. J Gastroenterol. 2011; 46:242–248.
Article14. Hochwald SN, Burke EC, Jarnagin WR, Fong Y, Blumgart LH. Association of preoperative biliary stenting with increased postoperative infectious complications in proximal cholangiocarcinoma. Arch Surg. 1999; 134:261–266.
Article15. Maguchi H, Takahashi K, Katanuma A, et al. Preoperative biliary drainage for hilar cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 2007; 14:441–446.
Article16. Ortner MA. Photodynamic therapy for cholangiocarcinoma: overview and new developments. Curr Opin Gastroenterol. 2009; 25:472–476.
Article17. Toyota N, Takada T, Amano H, Yoshida M, Miura F, Wada K. Endoscopic naso-gallbladder drainage in the treatment of acute cholecystitis: alleviates inflammation and fixes operator’s aim during early laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 2006; 13:80–85.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The efficacy of a novel integrated outside biliary stent and nasobiliary drainage catheter system for acute cholangitis: a single center pilot study
- Endoscopic Stent Placement in the Palliation of Malignant Biliary Obstruction
- Usefulness of the double-guidewire technique for endoscopic procedures in the field of biliary and pancreatic diseases
- Review of Simultaneous Double Stenting Using Endoscopic Ultrasound-Guided Biliary Drainage Techniques in Combined Gastric Outlet and Biliary Obstructions
- The usefulness of endoscopic nasobiliary drainage(ENBD) in biliary and pancreatic disease