Investig Clin Urol.
2017 Jun;58(Suppl 1):S32-S37. 10.4111/icu.2017.58.S1.S32.
Vesicoureteral reflux and continuous prophylactic antibiotics
- Affiliations
-
- 1Department of Urology, University of Michigan, Ann Arbor, MI, USA. lted@med.umich.edu
- KMID: 2379893
- DOI: http://doi.org/10.4111/icu.2017.58.S1.S32
Abstract
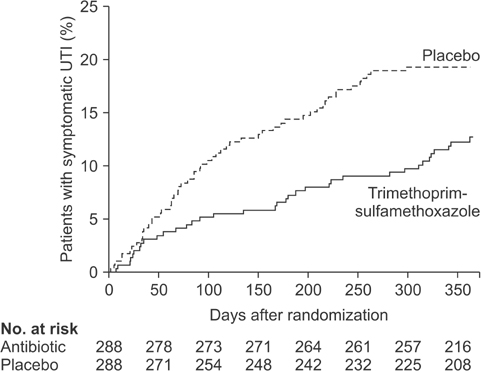
- Vesicoureteral reflux (VUR) management must be tailored based on the risk for further infections and renal scarring, gender, likelihood of spontaneous resolution, and parental preferences. Because we now understand that sterile VUR is benign and most reflux spontaneously resolves over time, the initial approach in majority of children is non-surgical with continuous antibiotic prophylaxis (CAP) and correction of bladder and bowel dysfunction. Despite increasing utilization of CAP over the past four decades, the efficacy of antibiotic prophylaxis has been questioned due to conflicting results of studies plagued with design flaws and inadequate subject sample size. The Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR) trial, which was designed to address many of the limitations from previous studies, provided much needed answers. In this review, we sought to describe the controversy surrounding VUR management, highlight the results of RIVUR trial, and discuss how the RIVUR findings impact our understanding of CAP in the management of VUR.
MeSH Terms
Figure
Cited by 2 articles
-
Susceptibility of the Index Urinary Tract Infection to Prophylactic Antibiotics Is a Predictive Factor of Breakthrough Urinary Tract Infection in Children with Primary Vesicoureteral Reflux Receiving Continuous Antibiotic Prophylaxis
Jun Nyung Lee, Kyeong-Hyeon Byeon, Myeong Jin Woo, Hee Sun Baek, Min Hyun Cho, Shin Young Jeong, So Mi Lee, Ji Yeon Ham, Yun-Sok Ha, Hyun Tae Kim, Eun Sang Yoo, Tae Gyun Kwon, Sung Kwang Chung
J Korean Med Sci. 2019;34(21):. doi: 10.3346/jkms.2019.34.e156.Pediatric vesicoureteral reflux: Slow but steady steps
Yong Seung Lee, Sang Won Han
Investig Clin Urol. 2017;58(Suppl 1):S1-S3. doi: 10.4111/icu.2017.58.S1.S1.
Reference
-
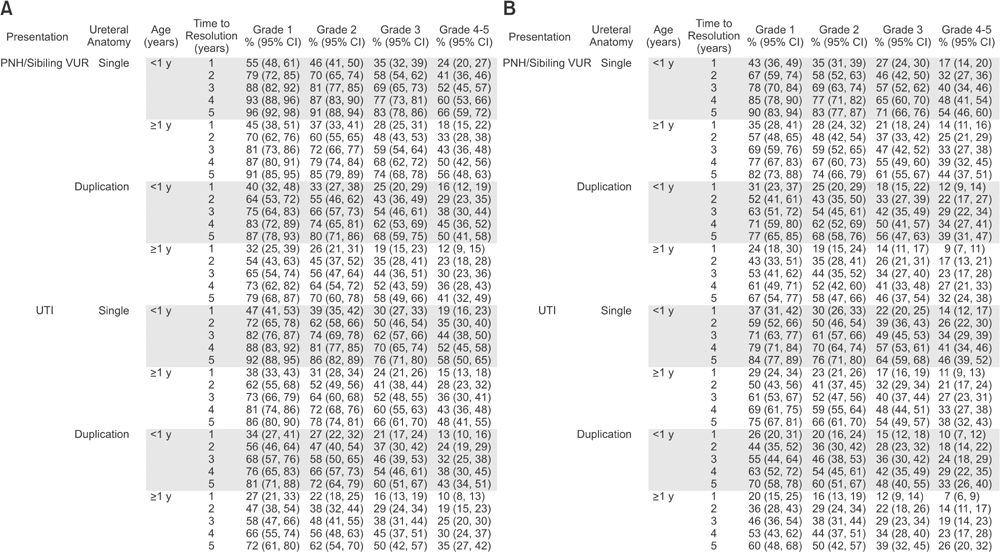
1. Tullus K. Vesicoureteric reflux in children. Lancet. 2015; 385:371–379.2. Baker R, Barbaris HT. Comparative results of urological evaluation of children with initial and recurrent urinary tract infection. J Urol. 1976; 116:503–505.3. Mackie GG, Stephens FD. Duplex kidneys: a correlation of renal dysplasia with position of the ureteric orifice. Birth Defects Orig Artic Ser. 1977; 13:313–321.4. Khoury AE, Bägli DJ. Vesicoureteral reflux. In : Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 11th ed. Philadelphia: Saunders;2016. p. 3138–3139.5. Gordon I, Peters AM, Morony S. Indirect radionuclide cystography: a sensitive technique for the detection of vesico-ureteral reflux. Pediatr Nephrol. 1990; 4:604–606.6. Massanyi EZ, Preece J, Gupta A, Lin SM, Wang MH. Utility of screening ultrasound after first febrile UTI among patients with clinically significant vesicoureteral reflux. Urology. 2013; 82:905–909.7. Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE. International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol. 1985; 15:105–109.8. Estrada CR Jr, Passerotti CC, Graham DA, Peters CA, Bauer SB, Diamond DA, et al. Nomograms for predicting annual resolution rate of primary vesicoureteral reflux: results from 2,462 children. J Urol. 2009; 182:1535–1541.9. Schaeffer AJ, Greenfield SP, Ivanova A, Cui G, Zerin JM, Chow JS, et al. Reliability of grading of vesicoureteral reflux and otherfindings on voiding cystourethrography. J Pediatr Urol. 2016; 09. 06. [Epub]. DOI: 10.1016/j.jpurol.2016.06.020.10. Silva JM, Diniz JS, Lima EM, Vergara RM, Oliveira EA. Predictive factors of resolution of primary vesico-ureteric reflux: a multivariate analysis. BJU Int. 2006; 97:1063–1068.11. Yeung CK, Sreedhar B, Sihoe JD, Sit FK. Renal and bladder functional status at diagnosis as predictive factors for the outcome of primary vesicoureteral reflux in children. J Urol. 2006; 176:1152–1156.12. Van Arendonk KJ, Madsen MT, Austin JC, Hawtrey CE, Graham MM, Cooper CS. Nuclear cystometrogram-determined bladder pressure at onset of vesicoureteral reflux predicts spontaneous resolution. Urology. 2007; 69:767–770.13. Hodson CJ, Maling TM, McManamon PJ, Lewis MG. The pathogenesis of reflux nephropathy (chronic atrophic pyelonephritis). Br J Radiol. 1975; Suppl 13. 1–26.14. Wennerström M, Hansson S, Jodal U, Stokland E. Primary and acquired renal scarring in boys and girls with urinary tract infection. J Pediatr. 2000; 136:30–34.15. Garin EH, Olavarria F, Garcia Nieto V, Valenciano B, Campos A, Young L. Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Pediatrics. 2006; 117:626–632.16. Montini G, Rigon L, Zucchetta P, Fregonese F, Toffolo A, Gobber D, et al. Prophylaxis after first febrile urinary tract infection in children? A multicenter, randomized, controlled, non-inferiority trial. Pediatrics. 2008; 122:1064–1071.17. Pennesi M, Travan L, Peratoner L, Bordugo A, Cattaneo A, Ronfani L, et al. Is antibiotic prophylaxis in children with vesicoureteral reflux effective in preventing pyelonephritis and renal scars? A randomized, controlled trial. Pediatrics. 2008; 121:e1489–e1494.18. Roussey-Kesler G, Gadjos V, Idres N, Horen B, Ichay L, Leclair MD, et al. Antibiotic prophylaxis for the prevention of recurrent urinary tract infection in children with low grade vesicoureteral reflux: results from a prospective randomized study. J Urol. 2008; 179:674–679.19. Craig JC, Simpson JM, Williams GJ, Lowe A, Reynolds GJ, Mc-Taggart SJ, et al. Antibiotic prophylaxis and recurrent urinary tract infection in children. N Engl J Med. 2009; 361:1748–1759.20. Brandström P, Jodal U, Sillén U, Hansson S. The Swedish reflux trial: review of a randomized, controlled trial in children with dilating vesicoureteral reflux. J Pediatr Urol. 2011; 7:594–600.21. RIVUR Trial Investigators. Hoberman A, Greenfield SP, Mattoo TK, Keren R, Mathews R, et al. Antimicrobial prophylaxis for children with vesicoureteral reflux. N Engl J Med. 2014; 370:2367–2376.22. Copp HL, Nelson CP, Shortliffe LD, Lai J, Saigal CS, Kennedy WA, et al. Compliance with antibiotic prophylaxis in children with vesicoureteral reflux: results from a national pharmacy claims database. J Urol. 2010; 183:1994–1999.23. Tasian G, Furth S. Narrowing the focus: what we now know (and still don't know) about antibiotic prophylaxis for children with vesicoureteral reflux. Am J Kidney Dis. 2015; 65:214–216.24. Mattoo TK, Chesney RW, Greenfield SP, Hoberman A, Keren R, Mathews R, et al. Renal Scarring in the Randomized Intervention for Children with Vesicoureteral Reflux (RIVUR) Trial. Clin J Am Soc Nephrol. 2016; 11:54–61.25. Greenfield SP. Editorial comment. J Urol. 2015; 193:5 Suppl. 1777.26. Wang HH, Gbadegesin RA, Foreman JW, Nagaraj SK, Wigfall DR, Wiener JS, et al. Efficacy of antibiotic prophylaxis in children with vesicoureteral reflux: systematic review and meta-analysis. J Urol. 2015; 193:963–969.27. de Bessa J Jr, de Carvalho Mrad FC, Mendes EF, Bessa MC, Paschoalin VP, Tiraboschi RB, et al. Antibiotic prophylaxis for prevention of febrile urinary tract infections in children with vesicoureteral reflux: a meta-analysis of randomized, controlled trials comparing dilated to nondilated vesicoureteral reflux. J Urol. 2015; 193:5 Suppl. 1772–1777.28. Williams GJ, Lee A, Craig JC. Long-term antibiotics for preventing recurrent urinary tract infection in children. Cochrane Database Syst Rev. 2001; (4):CD001534.29. Furuya EY, Lowy FD. Antimicrobial-resistant bacteria in the community setting. Nat Rev Microbiol. 2006; 4:36–45.30. Shehab N, Patel PR, Srinivasan A, Budnitz DS. Emergency department visits for antibiotic-associated adverse events. Clin Infect Dis. 2008; 47:735–743.31. Gerber JS, Bryan M, Ross RK, Daymont C, Parks EP, Localio AR, et al. Antibiotic exposure during the first 6 months of life and weight gain during childhood. JAMA. 2016; 315:1258–1265.32. Murk W, Risnes KR, Bracken MB. Prenatal or early-life exposure to antibiotics and risk of childhood asthma: a systematic review. Pediatrics. 2011; 127:1125–1138.33. Hviid A, Svanström H, Frisch M. Antibiotic use and inflammatory bowel diseases in childhood. Gut. 2011; 60:49–54.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Case-Control Study for Contralateral Vesicoureteral Reflux in Patient with Unilateral Cohen's Reimplantation: Is Contralateral Vesicoureteral Reflux Caused by Postoperative Trigonal Distortion?
- Clinical Aspects of Vesicoureteral Reflux
- Endoscopic teflon injection in vesicoureteral reflux
- Clinical Observation on Vesicoureteral Reflex Following Renal Tuberculosis
- Reflux Nephropathy in Children