Investig Clin Urol.
2017 Jun;58(Suppl 1):S23-S31. 10.4111/icu.2017.58.S1.S23.
Imaging studies and biomarkers to detect clinically meaningful vesicoureteral reflux
- Affiliations
-
- 1Medical University of South Carolina, Charleston, SC, USA. prasadm@musc.edu
- 2Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, USA.
- KMID: 2379892
- DOI: http://doi.org/10.4111/icu.2017.58.S1.S23
Abstract
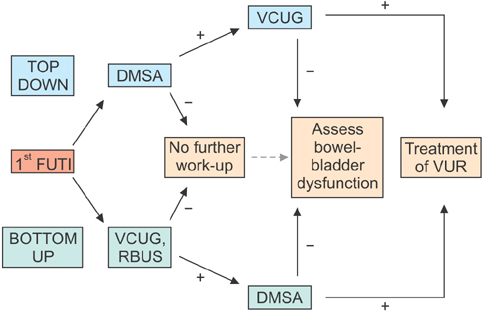
- The work-up of a febrile urinary tract infection is generally performed to detect vesicoureteral reflux (VUR) and its possible complications. The imaging modalities most commonly used for this purpose are renal-bladder ultrasound, voiding cystourethrogram and dimercapto-succinic acid scan. These studies each contribute valuable information, but carry individual benefits and limitations that may impact their efficacy. Biochemical markers are not commonly used in pediatric urology to diagnose or differentiate high-risk disease, but this is the emerging frontier, which will hopefully change our approach to VUR in the future. As it becomes more apparent that there is tremendous clinical variation within grades of VUR, the need to distinguish clinically significant from insignificant disease grows. The unfortunate truth about VUR is that recommendations for treatment may be inconsistent. Nuances in clinical decision-making will always exist, but opinions for medical versus surgical intervention should be more standardized, based on risk of injury to the kidney.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Pediatric vesicoureteral reflux: Slow but steady steps
Yong Seung Lee, Sang Won Han
Investig Clin Urol. 2017;58(Suppl 1):S1-S3. doi: 10.4111/icu.2017.58.S1.S1.
Reference
-
1. Shaikh N, Morone NE, Bost JE, Farrell MH. Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J. 2008; 27:302–308.2. Herz D, Merguerian P, McQuiston L, Danielson C, Gheen M, Brenfleck L. 5-year prospective results of dimercapto-succinic acid imaging in children with febrile urinary tract infection: proof that the top-down approach works. J Urol. 2010; 184:4 Suppl. 1703–1709.3. Smellie JM, Barratt TM, Chantler C, Gordon I, Prescod NP, Ransley PG, et al. Medical versus surgical treatment in children with severe bilateral vesicoureteric reflux and bilateral nephropathy: a randomised trial. Lancet. 2001; 357:1329–1333.4. Coulthard MG, Verber I, Jani JC, Lawson GR, Stuart CA, Sharma V, et al. Can prompt treatment of childhood UTI prevent kidney scarring? Pediatr Nephrol. 2009; 24:2059–2063.5. Coulthard MG. Vesicoureteric reflux is not a benign condition. Pediatr Nephrol. 2009; 24:227–232.6. Riccabona M, Avni FE, Blickman JG, Dacher JN, Darge K, Lobo ML, et al. Imaging recommendations in paediatric uroradiology: minutes of the ESPR workgroup session on urinary tract infection, fetal hydronephrosis, urinary tract ultrasonography and voiding cystourethrography, Barcelona, Spain, June 2007. Pediatr Radiol. 2008; 38:138–145.7. Völkl-Kernstock S, Felber M, Schabmann A, Inschlag N, Karesch L, Ponocny-Seliger E, et al. Comparing stress levels in children aged 2-8 years and in their accompanying parents during first-time versus repeated voiding cystourethrograms. Wien Klin Wochenschr. 2008; 120:414–421.8. Lee HY, Soh BH, Hong CH, Kim MJ, Han SW. The efficacy of ultrasound and dimercaptosuccinic acid scan in predicting vesicoureteral reflux in children below the age of 2 years with their first febrile urinary tract infection. Pediatr Nephrol. 2009; 24:2009–2013.9. American Academy of Pediatrics. Committee on Quality Improvement. Subcommittee on Urinary Tract Infection. Practice parameter: the diagnosis, treatment, and evaluation of the initial urinary tract infection in febrile infants and young children. Pediatrics. 1999; 103(4 Pt 1):843–852.10. Peters CA, Skoog SJ, Arant BS Jr, Copp HL, Elder JS, Hudson RG, et al. Summary of the AUA guideline on management of primary vesicoureteral reflux in children. J Urol. 2010; 184:1134–1144.11. Peters CA. Vesicoureteral reflux: seeing the trees in the forest. J Urol. 2010; 184:8–9.12. Pennesi M, Travan L, Peratoner L, Bordugo A, Cattaneo A, Ronfani L, et al. Is antibiotic prophylaxis in children with vesicoureteral reflux effective in preventing pyelonephritis and renal scars? A randomized, controlled trial. Pediatrics. 2008; 121:e1489–e1494.13. Garin EH, Olavarria F, Garcia Nieto V, Valenciano B, Campos A, Young L. Clinical significance of primary vesicoureteral reflux and urinary antibiotic prophylaxis after acute pyelonephritis: a multicenter, randomized, controlled study. Pediatrics. 2006; 117:626–632.14. Montini G, Rigon L, Zucchetta P, Fregonese F, Toffolo A, Gobber D, et al. Prophylaxis after first febrile urinary tract infection in children? A multicenter, randomized, controlled, noninferiority trial. Pediatrics. 2008; 122:1064–1071.15. Roussey-Kesler G, Gadjos V, Idres N, Horen B, Ichay L, Leclair MD, et al. Antibiotic prophylaxis for the prevention of recurrent urinary tract infection in children with low grade vesicoureteral reflux: results from a prospective randomized study. J Urol. 2008; 179:674–679.16. Craig JC, Simpson JM, Williams GJ, Lowe A, Reynolds GJ, Mc-Taggart SJ, et al. Antibiotic prophylaxis and recurrent urinary tract infection in children. N Engl J Med. 2009; 361:1748–1759.17. Subcommittee on Urinary Tract Infection. Steering Committee on Quality Improvement and Management. Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics. 2011; 128:595–610.18. RIVUR Trial Investigators. Hoberman A, Greenfield SP, Mattoo TK, Keren R, Mathews R, et al. Antimicrobial prophylaxis for children with vesicoureteral reflux. N Engl J Med. 2014; 370:2367–2376.19. Brandström P, Esbjörner E, Herthelius M, Swerkersson S, Jodal U, Hansson S. The Swedish reflux trial in children: III. Urinary tract infection pattern. J Urol. 2010; 184:286–291.20. National Institute for Health and Clinical Excellence (NICE). Urinary tract infection in under 16s: diagnosis and management. Clinical guideline 54. August 2007 [Internet]. London: National Institute for Health and Clinical Excellence;c2017. cited 2016 Dec 10. Available from: https://www.nice.org.uk/guidance/cg54.21. Guidelines for the management of acute urinary tract infection in childhood. Report of a Working Group of the Research Unit, Royal College of Physicians. J R Coll Physicians Lond. 1991; 25:36–42.22. Bush NC, Keays M, Adams C, Mizener K, Pritzker K, Smith W, et al. Renal damage detected by DMSA, despite normal renal ultrasound, in children with febrile UTI. J Pediatr Urol. 2015; 11:126.e1–126.e7.23. Narchi H, Marah M, Khan AA, Al-Amri A, Al-Shibli A. Renal tract abnormalities missed in a historical cohort of young children with UTI if the NICE and AAP imaging guidelines were applied. J Pediatr Urol. 2015; 11:252.e1–252.e7.24. Logvinenko T, Chow JS, Nelson CP. Predictive value of specific ultrasound findings when used as a screening test for abnormalities on VCUG. J Pediatr Urol. 2015; 11:176.e1–176.e7.25. Hoberman A, Charron M, Hickey RW, Baskin M, Kearney DH, Wald ER. Imaging studies after a first febrile urinary tract infection in young children. N Engl J Med. 2003; 348:195–202.26. Mahant S, Friedman J, MacArthur C. Renal ultrasound findings and vesicoureteral reflux in children hospitalised with urinary tract infection. Arch Dis Child. 2002; 86:419–420.27. Nelson CP, Johnson EK, Logvinenko T, Chow JS. Ultrasound as a screening test for genitourinary anomalies in children with UTI. Pediatrics. 2014; 133:e394–e403.28. Cooper CS, Alexander SE, Kieran K, Storm DW. Utility of the distal ureteral diameter on VCUG for grading VUR. J Pediatr Urol. 2015; 11:183.e1–183.e6.29. Alexander SE, Arlen AM, Storm DW, Kieran K, Cooper CS. Bladder volume at onset of vesicoureteral reflux is an independent risk factor for breakthrough febrile urinary tract infection. J Urol. 2015; 193:1342–1346.30. Knudson MJ, Austin JC, McMillan ZM, Hawtrey CE, Cooper CS. Predictive factors of early spontaneous resolution in children with primary vesicoureteral reflux. J Urol. 2007; 178(4 Pt 2):1684–1688.31. Arlen AM, Alexander SE, Wald M, Cooper CS. Computer model predicting breakthrough febrile urinary tract infection in children with primary vesicoureteral reflux. J Pediatr Urol. 2016; 12:288.e1–288.e5.32. Herz DB. The top-down approach: an expanded methodology. J Urol. 2010; 183:856–857.33. Wu HY, Shortliffe LD. Top-down approach for evaluation of urinary tract infection. Urology. 2010; 75:514–515.34. Gleeson FV, Gordon I. Imaging in urinary tract infection. Arch Dis Child. 1991; 66:1282–1283.35. Pohl HG, Belman AB. The "top-down" approach to the evaluation of children with febrile urinary tract infection. Adv Urol. 2009; 783409.36. Polito C, La Manna A, Rambaldi PF, Valentini N, Marte A, Lama G. Long-term evolution of renal damage associated with unilateral vesicoureteral reflux. J Urol. 2007; 178(3 Pt 1):1043–1047.37. Shaikh N, Spingarn RB, Hum SW. Dimercaptosuccinic acid scan or ultrasound in screening for vesicoureteral reflux among children with urinary tract infections. Cochrane Database Syst Rev. 2016; 7:CD010657.38. Mathews R, Carpenter M, Chesney R, Hoberman A, Keren R, Mattoo T, et al. Controversies in the management of vesicoureteral reflux: the rationale for the RIVUR study. J Pediatr Urol. 2009; 5:336–341.39. Brandström P, Nevéus T, Sixt R, Stokland E, Jodal U, Hansson S. The Swedish reflux trial in children: IV. Renal damage. J Urol. 2010; 184:292–297.40. Lim R. Vesicoureteral reflux and urinary tract infection: evolving practices and current controversies in pediatric imaging. AJR Am J Roentgenol. 2009; 192:1197–1208.41. Parvex P, Willi JP, Kossovsky MP, Girardin E. Longitudinal analyses of renal lesions due to acute pyelonephritis in children and their impact on renal growth. J Urol. 2008; 180:2602–2606.42. Grattan-Smith JD, Little SB, Jones RA. Evaluation of reflux nephropathy, pyelonephritis and renal dysplasia. Pediatr Radiol. 2008; 38:Suppl 1. S83–S105.43. Chang SL, Caruso TJ, Shortliffe LD. Magnetic resonance imaging detected renal volume reduction in refluxing and nonrefluxing kidneys. J Urol. 2007; 178:2550–2554.44. Lee SK, Chang Y, Park NH, Kim YH, Woo S. Magnetic resonance voiding cystography in the diagnosis of vesicoureteral reflux: comparative study with voiding cystourethrography. J Magn Reson Imaging. 2005; 21:406–414.45. Arthurs OJ, Edwards AD, Joubert I, Graves MJ, Set PA, Lomas DJ. Interactive magnetic resonance voiding cystourethrography (iMRVC) for vesicoureteric reflux (VUR) in unsedated infants: a feasibility study. Eur Radiol. 2011; 21:1874–1881.46. Kim JW, Lee CH, Yoo KH, Je BK, Kiefer B, Park YS, et al. Intravoxel incoherent motion magnetic resonance imaging to predict vesicoureteral reflux in children with urinary tract infection. Eur Radiol. 2016; 26:1670–1677.47. Kis E, Nyitrai A, Várkonyi I, Máttyus I, Cseprekál O, Reusz G, et al. Voiding urosonography with second-generation contrast agent versus voiding cystourethrography. Pediatr Nephrol. 2010; 25:2289–2293.48. Duran C, Valera A, Alguersuari A, Ballesteros E, Riera L, Martin C, et al. Voiding urosonography: the study of the urethra is no longer a limitation of the technique. Pediatr Radiol. 2009; 39:124–131.49. Giordano M, Marzolla R, Puteo F, Scianaro L, Caringella DA, Depalo T. Voiding urosonography as first step in the diagnosis of vesicoureteral reflux in children: a clinical experience. Pediatr Radiol. 2007; 37:674–677.50. Tse KS, Wong LS, Lau HY, Fok WS, Chan YH, Tang KW, et al. Paediatric vesicoureteric reflux imaging: where are we? Novel ultrasound-based voiding urosonography. Hong Kong Med J. 2014; 20:437–443.51. Strimbu K, Tavel JA. What are biomarkers? Curr Opin HIV AIDS. 2010; 5:463–466.52. Lee RS. Biomarkers for pediatric urological disease. Curr Opin Urol. 2009; 19:397–401.53. Kitao T, Kimata T, Yamanouchi S, Kato S, Tsuji S, Kaneko K. Urinary biomarkers for screening for renal scarring in children with febrile urinary tract infection: Pilot Study. J Urol. 2015; 194:766–771.54. Ai JW, Liu Y, Zeng XT, Lei Q, Zou L, Pei B. Angiotensin converting enzyme gene insertion/deletion polymorphism and vesicoureteral reflux in children: a meta-analysis of 14 casecontrol studies. Medicine (Baltimore). 2015; 94:e2421.55. Mahyar A, Ayazi P, Yarigarravesh MH, Khoeiniha MH, Oveisi S, Sahmani AA, et al. Serum interleukin -8 is not a reliable marker for prediction of vesicoureteral reflux in children with febrile urinary tract infection. Int Braz J Urol. 2015; 41:1160–1166.56. Parmaksız G, Noyan A, Dursun H, İnce E, Anarat R, Cengiz N. Role of new biomarkers for predicting renal scarring in vesicoureteral reflux: NGAL, KIM-1, and L-FABP. Pediatr Nephrol. 2016; 31:97–103.57. Leroy S, Bouissou F, Fernandez-Lopez A, Gurgoze MK, Karavanaki K, Ulinski T, et al. Prediction of high-grade vesicoureteral reflux after pediatric urinary tract infection: external validation study of procalcitonin-based decision rule. PLoS One. 2011; 6:e29556.58. Simões e, Valério FC, Vasconcelos MA, Miranda DM, Oliveira EA. Interactions between cytokines, congenital anomalies of kidney and urinary tract and chronic kidney disease. Clin Dev Immunol. 2013; 2013:597920.59. Coulthard MG. Do kidneys outgrow the risk of reflux nephropathy? Pediatr Nephrol. 2002; 17:477–480.60. Craig JC, Wheeler DM, Irwig L, Howman-Giles RB. How accurate is dimercaptosuccinic acid scintigraphy for the diagnosis of acute pyelonephritis? A meta-analysis of experimental studies. J Nucl Med. 2000; 41:986–993.